* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download STI
Tuberculosis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Sarcocystis wikipedia , lookup
Gastroenteritis wikipedia , lookup
Anaerobic infection wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Trichinosis wikipedia , lookup
Human papillomavirus infection wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Hepatitis B wikipedia , lookup
Schistosomiasis wikipedia , lookup
Hepatitis C wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Epidemiology of syphilis wikipedia , lookup
Microbicides for sexually transmitted diseases wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Neonatal infection wikipedia , lookup
Herpes simplex wikipedia , lookup
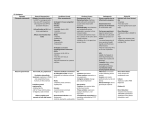
Sexually Transmitted Infections Tory Davis, PA-C STD? STI? VD? a.k.a. Venereal Diseases Increasingly, the term sexually transmitted infection (STI) is used: a person may be infected, and may potentially infect others, without showing signs of disease. An STI is an illness that is spread through sexual contact: Vagina/penis, vulva/vulva, oral sex, and anal sex. Other routes: kissing, IV drug administration, sharing of sex toys, childbirth or breastfeeding. Facts 65 million of people living in the US with STI 15 million of new STI cases each year 2/3 of all STIs occurs in people 25 yrs of age or younger one in four new STI cases occur in teenagers one in four Americans have genital herpes, and 80% of those with herpes are unaware they have it at least one in four Americans will get STI at some point in their lives One in Four CDC study released last year shows that 26% of teen girls has at least one of the most common STIs – HPV – Chlamydia – Trich – HSV Taking the History: The 5 Ps Partners Prevention of Pregnancy Protection from STDs Practices Past History of STDs Partners “Do you have sex with men, women, or both?” “In the past 2 months, how many partners have you had sex with?” “In the past 12 months, how many partners have you had sex with?” Prevention of pregnancy Are you or your partner trying to get pregnant? – If no, what are you doing to prevent pregnancy? Do you use condoms? Protection from STIs “What do you do to protect yourself from STIs and HIV?” Do you use condoms? – How often? Always, sometimes, or rarely? – – If “never:” “Why don’t you use condoms?” If “sometimes”: “In what situations or with whom do you not use condoms?” Practices “To understand your risks for STDs, I need to understand the kind(s) of sex you have had recently.” “Have you had vaginal sex, meaning ‘penis in vagina sex’”? – If yes, “Do you use condoms: never, sometimes, or always?” “Have you had anal sex, meaning ‘penis in rectum/anus sex’”? – If yes, “Do you use condoms: never, sometimes, or always?” “Have you had oral sex, meaning ‘mouth on penis/vagina/anus’”? – If yes, “Do you use a dental dam?” Past History of STIs “Have you ever had an STI?” “Have any of your partners had an STI?” – Additional questions to identify HIV and hepatitis risk “Have you or any of your partners ever injected drugs? “Have any of your partners exchanged money or drugs for sex?” “Is there anything else about your sexual practices that you think I might need to know about?” STIs Characterized by… Genital Ulcers: HSV, Syphilis, Chancroid Urethritis/Cervicitis: Gonorrhea, Chlamydia Vaginal Discharge: Bacterial vaginosis, Trichomoniasis, candidiasis Other: PID, Epididymitis/prostatitis, HPV/genital warts, proctitis/proctocolitis/enteritis Ectoparasites: Pediculosis pubis, scabies (covered in derm) Diseases Characterized by Genital Ulcers Herpes (*MC) Syphilis Chancroid Associated with increase risk of HIV Diagnosis based on history and physical is often inaccurate. Chancroid Cause: gram-negative bacillus—Haemophilus ducreyi Incubation: 3-5 days Initial lesion is a vesicopustule that breaks down to form a painful, soft ulcer with a necrotic base, surrounded by erythema Multiple lesions develop by autoinoculation Frequent inguinal adenitis often develops Well established cofactor for HIV transmission (10% may be infected). Chancroid Epi Transmission of H. ducreyi is almost exclusively by sexual contact Hygiene and cleanliness are important determinants of contagiousness The incidence in the U.S. has declined; <1,500 cases/year Prostitution is a major cause of spread (seen a lot during Korean and Vietnam wars) Chancroid Dx Hx PE Bacterial culture for H. ducreyi Chancroid Treatment Azithromycin 1 g orally once OR Ceftriaxone 250 mg intramuscularly (IM) OR Ciprofloxacin 500 mg orally BID for 3 days OR Erythromycin base 500 mg po TID for 7 days Syphilis Cause: spirochete (gram neg bac-t) Treponema pallidum Capable of infecting any organ or tissue in the body. Risk of transmission 30-50% in partner with primary syphilis. Three stages: primary, secondary, and late (tertiary) syphilis Also congenital and neurosyphilis Syphilis Epidemiology -Humans are only known host -Transmission by direct contact with infectious lesions, generally through sexual contact -The incidence is highest in sexually active 2029 year olds -Incidence: 70,000 case/year or about 7 per hour in the US -Higher risk for men, esp MSM Primary Syphilis 2-6 weeks after exposure Chancre- genital ulcer, painless with clean base and firm, indurated borders Regional lymphadenopathy 10-30 days post exposure, heals in 3-6 weeks Secondary Syphilis 2-8 weeks after chancre onset “The Great Imitator”- nonspecific sx: malaise, fatigue, HA, fever, sore throat Generalized lymphadenopathy Papulosquamous dermatosis- Pale, red discrete round lesions with scaling over surface on palms, soles, trunk Condyloma lata-papules coalesce and become large, flat highly contagious lesions Highly infectious mucous membrane lesions Secondary Syphilis Condyloma latamoist, flat, confluent plaques Latent syphilis Period of time between P/S and tertiary syphilis where lab tests will be positive, pt is infected, but no clinical signs Only infectious in pregnancy and transfusion Tertiary Syphilis 1-30 years after initial infection Late benign tertiary syphilis (gumma) Cardiovascular syphilis Neurosyphilis Gumma May form 1 to 10 years after initial infection Destructive granulomatous lesions affect any area Responds rapidly to treatment Cardiovascular Syphilis Begins 5 to 10 years after initial infection Clinically seen 20-30 years after infection Obliterative endarteritis of vasa vasorum Ascending aorta develops aortic insufficiency and aneurysm Neurosyphilis Occurs in 10% of untreated pts HA, mental deterioration, personality change plus 1. 2. 3. 4. 5. 6. 7. Tremor of lips, tongue or hands Argyll-Robertson pupil – look up Seizures Ataxia Aphasia Hyperreflexia Cognitive changes, can evolve into psychosis Screening for Syphilis Non-treponemal tests VDRL (Venereal Disease Research Laboratory) test. Screen for antibodies, not specific to T. pallidum RPR- rapid plasma reagin- antibody EIA- enzyme immunoassay test Diagnosing SyphilisTreponemal tests Fluorescent treponemal antibody absorption (FTA-ABS) test. Detects antibodies to T pallidum. Use after 3 weeks post-exposure. Blood or spinal fluid. Treponema pallidum particle agglutination assay (TPPA). Same as above, but blood only. Darkfield microscopy. Uses special microscope to examine fluid or tissue from a chancre. Mainly to diagnose syphilis in an early stage. Treatment -Benzathine penicillin G 2.4 million units IM once (if infected < 1 year) If PCN allergic -Doxycycline, ceftriaxone, azithromycin Alternate tx for pregnancy, congenital, latent, neurosyphilis, and postexposure prophylaxis (look-ups) Response to Treatment No definitive test of cure, reassess clinically and serologically in 6-12 months Consider treatment failure if symptoms persist or titer remains 4x normal If treatment failure; CSF testing, HIV testing, and benzathine penicillin G weekly x 3 weeks Tuskegee Syphilis Study 1932-1972 "The United States government did something that was wrong—deeply, profoundly, morally wrong. It was an outrage to our commitment to integrity and equality for all our citizens... clearly racist." —President Clinton's apology for the Tuskegee Syphilis Experiment to the eight remaining survivors, May 16, 1997 Genital Herpes Chronic, life-long viral infection caused by human herpesviruses Subclinical primary infections more common than clinically manifestations HSV persists in a latent state for the remainder of the host’s life in the sensory ganglia, then reactivation lesions appear in the distal sensory nerve distribution HSV 1 and 2 Etiology HSV-1 primarily transmitted by nonsexual routes, (ie infected saliva) – Causes cold sores and oropharynx stomatitis HSV-2 is usually transmitted sexually or maternally – causing genital herpes and neonatal infections – also it has been linked epidemiologically with carcinoma of the cervix Etiology This rough rule of HSV-1 above the waist and HSV-2 below the waist is no longer strictly true: – approximately 20% of genital herpes cases are due to HSV-1 – HSV-2 may induce oropharyngeal infections Epidemiology Risk of infection is approximately 75% following contact with a symptomatic case. At least 50 million persons in the United States have genital HSV infection. Genital Herpes (cont) HSV type 2 usually involves the genital tract, latent virus is in presacral ganglia Typical lesions are grouped, painful, small, and vesicular Asymptomatic shedding is possible and establishing a first episode of HSV-2 is difficult. Incubation is 2-7 days Diagnosis Usually done clinically however the classical painful multiple vesicular or ulcerative lesions are absent in many infected persons. May be detected by viral cultures of vesicular fluid or direct fluorescent antibody staining of scraped lesions may confirm diagnosis Presence of intranuclear inclusions and multinucleated giant cells on a Tzank preparation is supportive of a diagnosis of herpes viral infections. Who Gave it to Me? Often difficult to tell Latent period Difficult counseling Emphasize prevention of spread Treatment Antivirals – Acyclovir – Famcyclovir – Valacyclovir Dose and duration depends: – First episode – Recurrent episodes – Suppression Diseases Characterized by Urethritis and Cervicitis Gonoccocal infections Chlamydial infections Non-gonococcal infections Gonorrhea Caused by Neisseria gonorrhoeae a.k.a. “the clap” Can affect urethra, cervix, rectum, conjunctiva (ophthalmia neonatorum), oropharynx Gonococcal Epi 700,000 cases in US/year – But since a number of GC infections are asymptomatic or not reported it is estimated that there are 1-2 million total cases/year in the U.S Humans=only host Transmitted sexually Gonorrhea Symptoms Often asymptomatic – contributes spread Male: dysuria, purulent or mucopurulent urethral discharge – (word of the day: gleet) Female: vaginal discharge (actually from cervix), dysuria, post-coital bleeding, inter-menstrual bleeding Complications Men: epididymitis, prostatitis, proctitis Women: vaginitis, salpingitis, pelvic inflammatory disease Both: disseminated GC-systemic complication following the dissemination of gonococci from the primary site via the bloodstream. (arthralgias, fever, rash) Diagnosis 1. 2. 3. Evaluation of the presenting symptoms and sexual history Gram stain of urethral exudates and Culturing for N. gonorrhoeae Dual Therapy Patients with GC should be treated routinely with a regimen effective against C. trachomatis.—10-30% coinfection rates Once you dx GC, you don’t even have to test for chlamydia because it is more cost effective to treat for it. Gonorrhea Treatment Ceftriaxone 125 mg IM in a single dose OR Cefixime 400 mg orally in a single dose or 400 mg by suspension (200 mg/5ml) PLUS TREATMENT FOR CHLAMYDIA IF CHLAMYDIAL INFECTION IS NOT RULED OUT NB- fluoroquinolones no longer recommended due to resistance Gonorrhea-infant During childbirth, gonococci infect the conjunctivitis, pharynx, respiratory tract and gastrointestinal tract of the body. Routine prophylaxis with 1% AgNO4 or 0.5% erythromycin or 1% tetracycline applied directly to the eye following birth prevents opthalmia neonatorium Chlamydia Chlamydia Very common STI caused by Chlamydia trachomatis 1,030,911 reported cases in 2006 in US- likely very underreported “The Silent Disease” asymptomatic in 75% of women and 50% of men Chlamydia Symptoms Female: dysuria, vaginal discharge, lower abdominal pain, low back pain, nausea, fever, dysparunia, bleeding between menstrual periods Male: dysuria, urethral irritation, penile discharge Both- commonly- NO SYMPTOMS Complications Chlamydia is one of most common causes of infertility in women Unless screened for, infections can easily be missed until after significant damage done to reproductive tract- ie: tubal scarring Diagnosis Urine “dirty-catch” Cervical swab Urethral swab Culture, PCR, nucleic acid amplification, DNA probe, ELISA, EIA Treatment Azithromycin or doxycycline Coinfection with gonococcal infection is common; therefore, dual therapy is recommended. Reinfection is common because partner is not treated! Abstinence should be continued until 7 days after single-dose regimen or after completion of a 7-day regimen. “Non-gonoccocal urethritis” Diagnosed if Gram-negative intracellular diplococci cannot be identified on urethral smear. C. trachomatis is a frequent cause (15-55%) Confirmation of chlamydial infection is important because of partner referral. Complications: epididymitis, prostatitis and Reiter’s syndrome Etiology Most cases are unknown Ureaplasma urealyticum, Mycoplasma genitalium, T. vaginalis and HSV Diagnostic criteria Mucopurulent or purulent discharge Gram stain demonstrating > 5 WBCs (or intracellular Gram-positive diplococci) Positive leukocyte esterase test on first void urine or microscopic examination of firstvoid urine demonstrating >10 WBCs/HPF *All patients should be tested for gonococcal and chlamydial infections Non-GC Urethritis Treatment Same as chlamydia Azithromycin Doxycycline Diseases Characterized by Vaginal Discharges Bacterial vaginosis Trichomoniasis Vulvovaginal candidiasis *NB: vulvovaginal candidiasis and bacterial vaginosis are not usually STD—often diagnosed in women being evaluated for STDs Bacterial Vaginosis Clinical syndrome resulting in the replacement of Lactobacillus with high concentrations of anaerobic bacteria (Gardenerella, Mycoplasma) Most common cause of vaginal discharge and malodor. Pt c/o FISHY ODOR, worse after intercourse. Associated with multiple sex partners, new sex partner, douching; not thought to be sexually transmitted but women who have never been sexually active rarely affected NB-treating sexual partner not beneficial BV Diagnostic Criteria 1. 2. 3. 4. Requires 3 of the following: Homogenous, white discharge that smoothly coats vaginal wall The presence of clue cells of microscopic exam (pic next slide) pH >4.5 Fishy odor of discharge before or after KOH Clue cells Bacteria cover cell wall of epithelial cells Treatment Metronidazole 500 mg orally twice/day for 7 days or Metronidazole gel 0.75% one applicator intravaginally once/day x 5 days or Clindamycin cream 2%, one full applicator intravaginally at bedtime Trichomoniasis Caused by anaerobic protozoan T. vaginalis Most men are asymptomatic, while women have symptoms characterized by a diffuse, malodorous musty smelling, yellow-green discharge with vulvar irritation Increases risk of HIV infection Trich Diagnosis History, Physical exam Microscopy Culture Treatment Recommended Regimens Metronidazole 2 g orally in a single dose OR Tinidazole 2 g orally in a single dose FYI Vaginal trichomoniasis in pregnancy has been associated with adverse pregnancy outcome, premature rupture of the membranes, preterm delivery, and low birth weight Vulvovaginal Candidiasis Usually caused by C. albicans but occasionally by other species of Candida Sx included pruritus and vaginal discharge, vaginal soreness, vulvar burning, dyspareunia and dysuria. 75% of all women will have 1 episode of VVC, 45% will have more than 1 episode Diagnosis Clinically by pruritus and erythema in the vaginal area; white thick discharge is common. – Typically described as cottage cheese discharge Also yeast/pseudohyphae on wet mount or culture positive for Candida. Usually pH <4.5 10-20% of women may harbor Candida Normal—if asymptomatic do not treat Treatment Several of the –azole drugs to choose from (Butoconazole, clotrimazole, Miconazole, etc.) 1, 3, 7 day tx pv qhs Available OTC and by rx Oral agent available Fluconazole 150 mg orally, single dose- by rx only, hepatic metabolism PID Pelvic Inflammatory Disease PID Spectrum of inflammatory disorders of the upper female genital tract, including endometritis, salpingitis, tubo-ovarian abscess, and pelvic peritonitis—typically polymicrobial. STDs such as N. gonorrhoeae and C. trachomatis are often guilty; however microorganism that comprise the vaginal flora (anaerobes, Gardenerella, H flu, enteric Gram-negative rods) have also been associated with PID PID Epidemiology High morbidity in US – Annually: 850 k cases, 212 k admissions, 115 k surgeries Risk factors: – Multiple sex partners – History of previous PID – Menstruation (why?) – IUD use (but OCPs decrease risk) – Marital status (single women are at higher risk) – Asymptomatic gonococcal infection in either sexual partner. Presentation Can be subtle and therefore lead to inflammatory sequelae in the upper reproductive tract. In all settings, no single historical, physical, or laboratory finding is both sensitive and specific. PID Criteria Minimum criteria: – Uterine/adenexal tenderness – Cervical motion tenderness (CMT) Additional criteria: – – – – – – Oral temp > 101 F Abnormal cervical discharge Presence of WBC on vaginal secretions Elevated sed rate Elevated c-reactive protein Laboratory documentation of cervical infection with GC or chlamydia PID Criteria Most specific criteria – Endometrial biopsy with histopathologic evidence of endometritis – Transvaginal sonography or MRI showing thickened, fluid filled tubes with or without free fluid – Laparoscopic abnormalities consistent with PID Sequelae PID = most common cause of involuntary infertility in women. Dissemination to liver resulting in a perihepatitis Fitz-Hugh-Curtis syndrome; "Violin Strings" form between the abdominal wall and liver capsule (may occur in both gonococcal and nongonococcal types of PID) – can be diagnostic. Unilateral or bilateral ovarian abscesses (with mortality from rupture) Tubal occlusion, scarring, and adhesions (can cause chronic abd pain) Who gets admitted? Surgical emergencies can’t be excluded (ie: appendicitis) Pregnant Patient does not respond to oral antimicrobial therapy Patient unable to follow or tolerate outpatient regimen Patient has severe illness, nausea and vomiting, or high fever Patient has tubo-ovarian abscess Treatment (parenteral) Regimen A – Cefotetan 2 g IV every 12 hours OR Cefoxitin 2 g IV every 6 hours PLUS Doxycycline 100 mg orally or IV every 12 hours Regimen B – Clindamycin 900 mg IV every 8 hours PLUS Gentamicin loading dose IV or IM (2 mg/kg of body weight), followed by a maintenance dose (1.5 mg/kg) every 8 hours. Single daily dosing may be substituted. Treatment (Oral) Ceftriaxone 250 mg IM in a single dose PLUS Doxycycline 100 mg orally twice a day for 14 days WITH OR WITHOUT Metronidazole 500 mg orally twice a day for 14 days HPV Human Papillomavirus – Genital warts (Condylomata Acuminata) – Also cause cervical cancer- will be covered in greater depth in WH section in spring HPV More than 30 types of HPV can infect the genital tract Most are asymptomatic, unrecognized, or subclinical Visible warts are HPV types 6 or 11 Other types strongly associated with cervical neoplasms (16, 18, 31, 33, and 35) Genital Warts Flat, papular, or pedunculated growths on the genital mucosa Incidence ~ 1,000,000/year in US – That’s a lot of warts Most frequently affected are the penis, vulva, vagina, cervix, perineum, and perianal area Perfect use of condoms risk of HPV infection by 70% Pathophys HPV invades cells of the basal layer of the epidermis, penetrating skin and mucosal microabrasions in the genital area Following latent period (months-years), viral DNA, capsids, and particles are produced. Host cells become infected and develop the morphologic atypical koilocytosis of genital warts Genital Wart Diagnosis The application of 3%–5% acetic acid (vinegar) usually turns HPV-infected genital mucosal tissue to a whitish color (Clinical test) Biopsy Treatment Goal: removal of symptomatic lesions, may or may not eradicate or eliminate infectivity Options: – Podofilox 0.5% solution or gel or Imiquimod 5% cream (patient applied) – Cryotherapy or Podophyllin resin 10-25% or surgical removal (provider administered) Prevention Gardasil- HPV vaccine against HPV 6, 11, 16, and 18 Could prevent 90% of genital warts Licensed for use in girls 9-26 Now approved for males age 9-26 for prevention of HPV infection and genital warts – Being studies for penile/rectal cancer prevention