* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Slide 1
Cysticercosis wikipedia , lookup
Chagas disease wikipedia , lookup
Brucellosis wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Typhoid fever wikipedia , lookup
Neonatal infection wikipedia , lookup
Hepatitis C wikipedia , lookup
Tuberculosis wikipedia , lookup
Hepatitis B wikipedia , lookup
Schistosomiasis wikipedia , lookup
Marburg virus disease wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Trichinosis wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Gastroenteritis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Meningococcal disease wikipedia , lookup
Leptospirosis wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
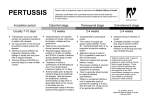
What is Pertussis Bordetella pertussis also referred to as Whooping Cough Whooping cough is a disease caused by a fastidious pathogen that invades the respiratory system. This pathogen secretes a toxin that disrupts the normal function of cilia in the lungs, resulting in a severe cough. Gram-negative, aerobic coccobacillus Humans are the only known host of pertussis. Bordetella pertussis is found in the mouth, nose, and throat Incidence Pertussis occurs year-round, peaking in the later part of the year. Annual incidence peaks every three to five years. Adolescents and adults represent over half of the reported cases nationally. Even among highly vaccinated populations, waning immunity leads to a substantial number of susceptible older children and adults. Outbreaks are more likely in fall and winter during cold and flu season Adolescents and adults can serve as an important reservoir for transmission to young infants, who are at increased risk for serious complications Prevalence Prevalence: Not all cases of whooping cough are reported or even diagnosed. Many cases of whooping cough are misdiagnosed due to individuals who have partial immunity (had only some of the required vaccinations) because their cough is less severe and mimics a common cold. There are approximately 40,000,000 cases of whooping cough reported annually across the world. In 2010, approximately 27,550 cases were reported in the United States, the most since 1959. source: CDC Whooping cough is the most common vaccine-preventable disease seen in the U.S. Symptoms Clinical symptoms of pertussis are similar to those of other infections: Runny nose No or low grade fever Cough These symptoms also appear with croup or bronchiolitis respiratory syncytial virus (RSV) in children, viral or bacterial pneumonia, and other causes of chronic cough in adults therefore, isolation of the bacterium and confirmation of the pertussis diagnosis if very important, particularly if an outbreak is suspected. Symptoms appear between 6 to 21 days (average 7 – 10) after exposure Pertussis: Three Stages Catarrhal stage (prodromal stage; indistinguishable from the common cold): Runny nose Sneezing Mild cough Low-grade fever Malaise Paroxysmal stage: After a week or two, Pertussis can be distinguished from the common cold by the paroxysm associated with coughing.; cough ending in a high-pitched inspiratory “whoop” sound, hence the name whooping cough. Coughing fits can last up to 12 weeks (which is why whooping cough is often referred to as the “100 day cough”). Fever is absent or minimal. Convalescent stage: Period of recovery as the cough slowly becomes less violent and the respiratory system begins to heal. May take up to 3 weeks to completely recover from B. pertussis. People with mild pertussis may have a persistent cough but without the whooping sound Transmission When an infected person coughs or sneezes, tiny germladen droplets are sprayed into the air and breathed into the lungs of those nearby. Pertussis is transmitted through respiratory and nasal secretions. A coughing attack can be very forceful; the velocity of air from a vigorous cough through the nearly closed vocal cords can approach 500 miles per hour. Pertussis is transmitted through droplets Transmission Pertussis is highly contagious Want proof? A person with pertussis will infect almost everyone in their household if those people aren’t vaccinated. As many as 80% of immunized household contacts of symptomatic cases acquire infection, mainly because of waning immunity. People with pertussis should avoid contact with others until they have been treated with antibiotics for five days Think Pertussis THINK of pertussis in anyone with the following symptoms, regardless of vaccination history: A cough in a person who has been notified of a close exposure to pertussis, A paroxysmal cough of any duration, with whooping, posttussive vomiting/gagging or apnea, or A persistent cough of unknown etiology, lasting more than seven days. Pertussis can strike at an age Diagnostic Testing Several types of laboratory tests are commonly used for the diagnosis of Bordetella pertussis. Culture is considered the gold standard because it is the only 100% specific method for identification. Other tests that can be performed include : polymerase chain reaction (PCR) and serology Serologic tests are more useful for diagnosis in later phases of the disease. For the CDC single point serology, the optimal timing for specimen collection is 2 to 8 weeks following cough onset, when the antibody titers are at their highest; however, serology may be performed on specimens collected up to 12 weeks following cough onset. Diagnostic Testing Culture testing is the criterion standard for B pertussis infection, owing to its high specificity (100%) for identification. The best time frame for nasopharyngeal specimen collection for culture testing is within the first 2 weeks of cough onset, when viable bacteria are present. Diagnostic Testing The best, but most difficult way is to try to detect the causative organism (Bordetella pertussis) in the back of the nose. This usually involves passing a swab on a wire through a nostril to the back of the throat and sending it to a medical lab to culture the material. This may take 5 to 7 days. If Bordetella pertussis or parapertussis grows this is usually taken as proof that it is whooping cough. Communicability of Pertussis Patients are most infectious early in the illness, but communicability may persist for three weeks after onset of cough. During the first week of illness, symptoms resemble “the common cold,” and paroxysmal coughing gradually develops during the second week of illness. Antimicrobial therapy decreases communicability and may limit the spread of disease. Prevent The Spread Advise patients with suspect pertussis to stay home from school, work, or other activities during which they could expose others until they have completed five full days of appropriate antimicrobial treatment. The bacteria is shed in nasopharyngeal secretions (droplets) and spreads when secretions get into mucous membranes such as the mouth, nose, eyes, or non-intact skin, especially when droplets are disseminated during coughing and sneezing. The incubation period for pertussis is usually 7 to 10 days, but can range from four to 21 days. Exception: If onset of cough was more than three weeks prior, the patient is no longer infectious, even if the cough persists. Communicability / Infectiousness Cases are potentially infectious for the first three weeks of cough. Inform patients with suspected pertussis to stay at home and avoid close contact with others until they have: Completed the fifth day of an appropriate antibiotic OR Had cough symptoms for at least three weeks. VDH Definition of close contact: within 3 feet of infected patient for: (a)1 hr continuous period, or (b) 10 hrs/week. Infectiousness after Antibiotic Patients are considered to be non-infectious after completing the fifth day of appropriate antimicrobial treatment; however, they should complete the full regimen to avoid bacterial relapse. Some health care providers are prescribing a one- or -three-day course of azithromycin (Zithromax®) in place of the five-day course that is currently one of the standard pertussis treatment options. While this may be appropriate for some respiratory illnesses, the data from published randomized clinical trials using a three-day course for treatment of pertussis are insufficient. The standard recommendations for a five-day course will remain unchanged until new data from comparative studies are available. Assessing Potential Contacts Contacts of pertussis cases may include: Household members (who stay overnight in the same household) Day care contacts in the same home day care or in the same classroom within a day care center (in part because of the increased severity of disease in very young children) Persons who have had direct face-to-face contact with an infectious pertussis case during coughing or sneezing Students participating in extracurricular activities with a pertussis case at least 10 hours per week Other persons spending at least 10 hours per week with an infectious case, during which time they are frequently in close proximity (i.e., within arm’s length) Other contacts identified by public health in an outbreak situation Local public health will work with the patient and the community to identify close contacts Prophylaxis Antimicrobial prophylaxis of close contacts: Antimicrobial prophylaxis (same regimen as therapy for cases) may be recommended to patients who are asymptomatic but are close contacts of pertussis cases. Antimicrobial prophylaxis is recommended if exposure to an infectious case occurred within the previous 21 days (the maximum incubation period for pertussis). Asymptomatic contacts receiving prophylaxis should not be excluded from their usual activities. Symptomatic contacts should be evaluated as suspect pertussis cases. In general, antimicrobial prophylaxis isn't recommended until there has been laboratory confirmation of the suspect case. Post Exposure for Healthcare Workers Data on the need for postexposure antimicrobial prophylaxis in T-dap immunized HCWs are inconclusive. If 21 days have lapsed since onset of cough in the index cause, chemoprophylaxis has limited value. Source: American Academy of Pediatrics Red Book Immunization of Case Contacts Immunization of case contacts In addition to providing antimicrobial therapy to case contacts, providers should assess pertussis vaccination status. Use DTaP or Tdap depending on the age of the case contact. • Give DTaP to catch-up children under age 7 years for any vaccinations due or overdue. There are two Tdap vaccines: •Adacel, licensed for persons age 11 through 64 years •Boostrix, licensed for persons age 10 years and older • Give Tdap to children age 7-10 years who have an incomplete DTaP schedule or who have never received a primary series of tetanus, diphtheria, and pertussis. In this instance, initiate a primary series giving Tdap as the first dose, followed by a dose of Td one month later, and a second Td six months later. This off-label use is ACIP recommended. • Give Tdap is routinely at age 11-12 years. However, do not wait for the pre-adolescent check-up to provide Tdap to household contacts; give it as early as age 10 years. • Give Tdap to adolescents and adults age 13 and older who have not yet received a Tdap. Give the dose regardless of the interval since the last Td. Make special effort to give Tdap to all persons who have or will have contact with children under age 1 year. • Give Tdap during every pregnancy, regardless of any doses given before pregnancy, preferably between weeks 27 and 36. Vaccination Diphtheria, Tetanus, and Pertussis Vaccines There are several formulations of vaccines used to prevent diphtheria, tetanus and pertussis. Some are combined with vaccines to prevent other diseases and reduce the total number of shots that someone receives at one office visit. DTaP, Tdap, and the most commonly used vaccines in the U.S. Td vaccines One of these (DTaP) is given to children younger than 7 years of age, and two (Tdap and Td) are given to older children and adults. Tdap is similar to Td but also containing protection against pertussis. Adolescents 11 through 18 years of age (preferably at age 11-12 years) should receive a single dose of Tdap. One dose of Tdap is also recommended for adults 19 years of age and older who did not get Tdap as an adolescent. Expectant mothers should receive Tdap during each pregnancy, preferably at 27 through 36 weeks. Tdap should also be given to 7-10 year olds who are not fully immunized against pertussis. Tdap can be given no matter when Td was last received. Updated Aug 2013 (Upper-case letters in these abbreviations denote fullstrength doses of diphtheria (D) and tetanus (T) toxoids and pertussis (P) vaccine. Lower-case “d” and “p” denote reduced doses of diphtheria and pertussis used in the adolescent/adultformulations. The “a” in DTaP and Tdap stands for “acellular,” meaning that the pertussis component contains only a part of the pertussis organism.) Both DTaP and Tdap protect against whooping cough, tetanus, and diphtheria. Vaccination Efficacy Pertussis vaccine is about 85% protective against pertussis infection For adolescents and adults, the Tdap vaccine has reduced diphtheria and pertussis vaccine dose to prevent local reactions (swelling, redness and pain) after immunization. Prevention Herd immunity does not completely protect unvaccinated children from pertussis. While vaccination provides the best protection from pertussis, some simple, basic hygiene steps can reduce the transmission: wash hands with soap and water cover up coughs and sneezes do not share cups and silverware In the hospital setting implement Droplet Precautions until 5 days after approx antimicrobial therapy; or if an antimicrobial therapy not initiated, until 3 weeks after onset of cough. Life Long Immunity ? Does the disease trigger long lasting immunity? Whooping cough does not trigger long lasting immunity. In fact, it is recommended that vaccinated adults repeat their vaccinations every 5-10 years to fully protect themselves against B. pertussis. Neither infection nor immunization provides lifelong immunity The Risk of Epidemic R0: (Reproductive ratio): The R0 of pertussis is 12-17, depending on geographical location. Because the R0 is greater than one, pertussis has the potential to become an epidemic unless vaccinations are used to increase the immunity of the population. In The News January 15, 2015 The CDC recommends a strategy called “cocooning”, which is a theory that if everyone who is in contact with a newborn is vaccinated, this should dramatically decrease the risk of pertussis being transmitted to an infant. A 25 day-old baby in Santa Barbara, CA died this week from pertussis, commonly known as whooping cough . The disease can be easily prevented by the DTaP or Tdap vaccines (also protect against tetanus and diphtheria), which can be given to infants as early as 6 weeks to 2 months old. According to the California Department of Public Health, infants who are too young to be fully immunized or those who are not vaccinated are most vulnerable to severe and fatal cases of pertussis. In 2014, 66 of the pertussis hospitalizations cases were children four months of age or younger. Whooping cough, an old disease causing havoc in a new era In Review Whooping cough (pertussis) is a highly contagious respiratory tract infection. Pertussis is a caused by the gram-negative coccobacillus Bordetella pertussis. Pertussis is transmitted by droplet transfer (usually from sneezing or coughing) from an infected person. In most cases, a negative pertussis result indicates the absence of whooping cough. In Review, cont. •Adults are the most common source of pertussis infection in infants. •Infants are at the greatest risk of serious complications, including death, from pertussis. Approximately half of infants less than 1 year of age who get pertussis are hospitalized. •The Centers for Disease Control and Prevention (CDC) estimates that worldwide, there are an estimated 16 million cases of pertussis and about 195,000 deaths per year. Since the 1980s, there has been an increase in the number of reported cases of pertussis in the US. •In adults, whooping cough can cause coughing spells that can affect breathing, eating, and sleeping. It can lead to cracked ribs and hospitalization. •Vaccination of pregnant women with Tdap is especially important to help protect infants. Pregnant women should get the vaccine late in the second trimester or in the third trimester for each pregancy.