* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Cardiology Conference
Remote ischemic conditioning wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Heart failure wikipedia , lookup
Rheumatic fever wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Electrocardiography wikipedia , lookup
Myocardial infarction wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Atrial septal defect wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Congenital heart defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
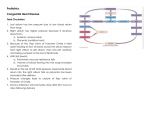
Cardiology Conference Gatchalian, Gaw, Geraldoy, Geronimo, Geronimo, Geronimo December 22, 2010 C.F. 2 months old / male CC: Fever Gestational History Birth History • • • • • 16 y/o primigravid G1P1 (1001) Prenatal check-up (?) - ferrous sulfate (unrecalled dose and duration of intake) No viral exposure 1 month of pregnancy – (+) alcohol and smoking 4 month of pregnancy – (+) UTI – completed cephalexin 500mg/cap q6 and amoxicillin 500mg/cap q8 x 7 days • • • • Full term 3.2 kg (N 3-3.5 kg) via NSD, singleton, cephalic presentation at a local hospital No complications APGAR not known C.F. 2 months old / male CC: Fever Feeding History • Mixed breastfeeding and milk formula • No feeding difficulty • (-) cyanosis • No regular check-up Developmental • At par with development History C.F. 2 months old / male CC: Fever • Incessantly crying and irritable • 2 episodes of vomiting of previously ingested food, ~1/2 cup/episode 2 days PTA • (-) cyanosis, good appetite • Crying and irritability persisted • Fever 38°C, colds with whitish nasal discharge and difficulty in breathing 1 day PTA • Health center – 0.65% NaCl drops 1-2 drops/nostril q8 and paracetamol 100mg/mL 0.5mL prn for fever Few hours PTA • Symptoms persisted • ADMISSION Review of Systems • • • • • • • • • • General: (-) noticeable weight loss Cutaneous: (-) rashes, (-) discoloration HEENT: (-) ear discharge, (-) epistaxis, (-) gum bleeding Respiratory: refer to HPI Cardiovascular: refer to HPI GI: (-) diarrhea, (-) constipation GUT: yellow urine, (-) edema of the hands and feet Extremities: (-) swelling, (-) joint swelling Nervous/Behaviour: (-) tremors, (-) convulsions Hematopoietic: (-) pallor, (-) easy bruisability Immunization History • • • • • Received the following at a local health center: BCG 1 Hepatitis B 1 DTP 1 OPV1 – Next dose due on December 27, 2010 Family Profile Age/ Gender Relation to the patient Educational Attainment Occupation Health P. F 17 y/o Male Father 3rd year high school Student Healthy C. R 16 y/o Female Mother High School graduate Housewife Healthy A.C 63 y/o Male Grandfather 2nd year college Government employee Healthy Y.C 54 y/o Female Grandmother 2nd year college Housewife (+) RHD Family History • • • • • (+) Rheumatic Heart Disease – maternal grandmother (-) HPN (-) Diabetes Mellitus (-) Pulmonary Tuberculosis (-) Allergies Socioeconomic and Environmental History • • • • • • • Four bedroom house made of wood and concrete Well lit and well ventilated Garbage is collected daily, no segregation Purified water from a water refilling station. Baby bottles also sterilized Stray cats Second hand smoke Physical Examination • General Survey: awake, alert, in respiratory distress with alar flaring, ill looking, well-nourished, well-hydrated • Vital Signs: HR 140 bpm, RR 70 cpm Temp 36.0 °C Wt 4.7 kg (z=below 0 normal) Ht: 49 cm (z= below -3 severely stunted) BMI: 19.58 (z= above 2 overweight) • Head circumference 37 cm, chest circumference 36 cm, abdominal circumference 40 cm • Skin: Warm, moist skin, pink in color, good skin turgor, no rashes, no jaundice Physical Examination • HEENT: normocephalic, anterior fontanel open, symmetric head, (-) scalp lesions, symmetric face; Eyeballs not sunken, pink palpebral conjunctiva, anicteric sclerae, pupils 2-3 mm ERTL; Midline nasal septum, (+) whitish nasal discharge; Moist buccal mucosae, nonhyperemic posterior pharyngeal wall; Supple neck, (-) palpable lymph nodes Physical Examination • Lungs/Chest: Symmetric chest expansion, (+) subcostal retractions, (+) crackles on both upper lung fields • Cardiovascular: adynamic precordium, no precordial bulge, (-) Harrison’s groove, (+) holosystolic murmur at the lower left parasternal area grade 4/6 • Abdomen: globular abdomen, normoactive bowel sounds, soft, non tender, no masses • Spine: midline, (-) sacral dimpling, (-) tufts of hair • Genitalia: Penis 2cm, testes descended bilaterally, no phimosis, no discharge • Extremities: full peripheral pulses, no cyanosis, no clubbing Neurologic Examination • Cerebrum: alert • Cranial nerves: Pupils isocoric, 2-3mm ERTL, (+) direct and consensual light reflex, (-) gross facial asymmetry, (+) gag reflex • Cerebellum: (-) no involuntary movements • Motor: (-) rigidity, (-) spasticity, (-) Flaccidity • Meningeal Signs: (-) nuchal rigidity, (-) Brudzinski’s, (-) Kernig’s, (-) tonic neck reflex Subjective Salient Features Pertinent Positives Pertinent Negatives • 2 months old/ Male • Born to a 16 year old primigravid • Prenatal check-up (?) • (+) Smoking and alcohol – 1st month of pregnancy • (+) UTI, treated – 4th month of pregnancy • Full term, NSD • No viral exposure • No complications at birth • Normal birth weight 3.2 kg • No feeding difficulties • At par with development • (+) URTI • Acyanotic • (+) RHD – maternal grandmother Objective Salient Features Pertinent Positives • Awake, alert, in respiratory distress with alar flaring, ill looking, wellnourished • PR 140 bpm, RR 70 cpm Temp 36.0 °C • (+) whitish nasal discharge • Symmetric chest expansion, (+) subcostal retractions, (+) crackles on both upper lung fields • Adynamic precordium, no precordial bulge, (-) Harrison’s groove, (+) holosystolic murmur at the lower left parasternal area grade 4/6 Pertinent Negatives • Warm, moist skin, pink in color • Full peripheral pulses, no cyanosis, no clubbing Presenting manifestation • • • • • • Incessant crying and irritable Vomiting Fever Development at par with age Alert, awake respiratory distress with alar flaring – symmetrical chest expansion – RR: 70 cpm (tachypneic); – (+) subcostal retractions – (+) crackles on both lung fields • Ht: 49 cm ( z=-3 severely stunted; BMI: 19.58 ( z= above 2 overweight) • (+) holosystolic murmur at the left parasternal area • small defects: physical findings are primarily cardiac manifestations • moderate-to-large defects: growth may be affected • Infants with small defects – normal vital signs. – Physiologic splitting of S2 is usually retained – harsh, holosystolic murmur is loudest along the lower left sternal border (LSB), and it is well localized. • Small defects can produce a high-pitched or squeaky noise. • Infants with moderate defects – normal length and decreased weight • Poor weight gain is a sensitive indicator of congestive heart failure (CHF). – – – – mild tachypnea, tachycardia, and an enlarged liver The precordial activity is accentuated. The murmur associated with thrill A holosystolic harsh murmur is most prominent over the lower LSB. – The intensity of the pulmonary component is usually normal or slightly increased. – a diastolic rumble may be detected in the mitral area. • This rumble suggests functional mitral stenosis secondary to a large left-to-right shunt and indicates a surgical-level shunt • Infants with large ventricular septal defects – signs of CHF are present • tachycardia, tachypnea, and hepatomegaly • cardiomegaly – The murmur is holosystolic but poorly localized and is usually associated with a diastolic rumble ASD • first heart sound may be normal or split – best appreciated at the upper left sternal border and may be transmitted to the lung fields. – second heart sound becomes widely split and fixed • fixed splitting of S2 is an important diagnostic finding in atrial-level shunting PDA • history of premature birth, perinatal distress, or perinatal hypoxia may be present • If the left-to-right shunt is large, precordial activity is increased • The apical impulse is laterally displaced • A thrill may be present in the suprasternal notch or in the left infraclavicular region • The first heart sound is typically normal. The second heart sound (S2) is often obscured by the murmur • Continuous machinery murmur AS • may present as congestive heart failure in the first week of life that mimic sepsis • Often, neonates with aortic stenosis are asymptomatic but present with a systolic murmur PS • • • • Most are asymptomatic cardiac murmurs that are detected during routine examination. moderate or severe pulmonary stenosis : exertional dyspnea. severe or critical obstruction: signs of systemic venous congestion Physical findings depend on the degree of obstruction. – – – – – – – – – – healthy and are well developed. trivial, mild, or moderate stenosis, and many with severe stenosis, are acyanotic A thrill may be felt in the suprasternal notch and at the left upper sternal border (pulmonic area) precordial thrill first heart sound may be normal; second heart sound is widely split A fourth heart sound may be heard at the left lower sternal border in patients with severe obstruction An ejection systolic click is heard along the left sternal border An ejection systolic murmur of grade II-VI to V-VI is best heard at the left upper sternal border with radiation into infraclavicular regions, axillae, or back. Hepatosplenomegaly may develop in cases of CHF. Peripheral pulmonary stenosis (commonly encountered in the neonate) is usually associated with a grade II/VI systolic murmur that radiates into the posterior lung fields and axillae coA • • • • • • Early presentation: poor feeding, tachypnea, and lethargy and progress to overt CHF and shock. Late presentation: Patients often present after the neonatal period with hypertension or a murmur Other presenting symptoms may include headaches, chest pain, fatigue, or even lifethreatening intracranial hemorrhage. Many patients are asymptomatic except for the incidentally noted hypertension. As with history, physical examination may conveniently separate patients into 2 groups: those who present early with heart failure and those who present later with hypertension. Early presentation – – – – Neonates: tachypnea, tachycardia, and increased work of breathing and may even be moribund with shock. blood pressure discrepancies between the upper and lower extremities and reduced or absent lower extremity pulses to palpation In patients with low cardiac output and ventricular dysfunction, pulses may be diminished diffusely, and BP gradients may seem minimal The murmur associated with coarctation of the aorta may be nonspecific yet is usually a systolic murmur in the left infraclavicular area and under the left scapula. Differential diagnosis CHD Cyanotic Noncyanotic Noncyanotic Difficulty breathing (dyspnea) Frequent respiratory infections in children Sensation of feeling the heart beat Shortness of breath (palpitations) in Fast breathing adults Hard breathing Shortness of Paleness breath with Failure to gain activity weight Fast heart rate Sweating while feeding Frequent respiratory infections VSD ASD Bounding pulse Fast breathing Poor feeding habits Shortness of breath Sweating while feeding Tiring very easily Poor growth PDA Abdominal distention Cyanosis in some patients Chest pain Fainting Fatigue Poor weight gain or failure to thrive in infants Dizziness or fainting Breathlessness with with severe blockage Shortness of breath activity Shortness of breath headache Pounding Chest pain Sudden death Chest pain Fainting, weakness, Cold feet or legs or dizziness with Failure to thrive activity Poor growth Palpitations AS PS CoA Clinical Impression Congenital Heart Disease Pneumonia VENTRICULAR SEPTAL DEFECT Ventricular Septal Defect • most common ACHD (25%) • SYNONYMS * Roger’s disease * Interventricular septal defect * Congenital cardiac anomaly Ventricular Septal Defect • Physical size of the VSD is a major determinant of the size of the left-to-right shunt • Restrictive VSD (usually <0.5 cm2) - right ventricular pressure is normal • Large nonrestrictive VSDs (usually >1.0 cm2)- right and left ventricular pressure is equalized Anatomical Classification • Membranous/ perimembranousVSD – Most common CHD (males>females) • • Muscular VSD – “Swiss cheese” VSD • Supracristal VSD – Least common ANCILLARY PROCEDURES ECHOCARDIOGRAPHY • Two-dimensional (2D) and Doppler colorflow mapping • May be used to identify the type of defect in the ventricular septum, size of the shunt and the degree of pulmonary hypertension ECHOCARDIOGRAPHY Size of Defect Results Small restrictive VSDs Normal tracing Medium-sized VSDs Broad, notched P wave characteristic of left atrial overload • Signs of LV volume overload — deep Q and tall R waves with tall T waves in leads V5 and V6 • Signs of atrial fibrillation are often present Large VSDs Right ventricular hypertrophy with rightaxis deviation. With further progression, the ECG shows biventricular hypertrophy; P waves may be notched or peaked. ECG OF PATIENT CHEST RADIOGRAPHY Size of Defect Radiographic Findings Small VSDs Normal Medium-sized VSDs Minimal cardiomegaly Borderline increase in pulmonary vasculature may be observed Large-sized VSDs Gross cardiomegaly with prominence of both ventricles, the left atrium, and the pulmonary artery Interstitial infiltrates are seen in both perihilar areas. The heart is not enlarged. Diaphragms are slightly flattened with intact costophrenic sulci Impression: Consider Pneumonia with mild hyperaeration TREATMENT Initial medical treatment for infants • Cardiac glycoside (digoxin 10-20mcg/kg per day) • Loop diuretics (furosemide 1–3 mg/kg per day) • ACE inhibitors (captopril 0.5–2 mg/kg per day) CARDIAC GLYCOSIDES • possess positive inotropic activity, which is mediated by inhibition of sodium-potassium adenosine triphosphatase (ATPase). • also reduces conductivity in the heart, particularly through the AV node; therefore, they have a negative chronotropic effect • used to slow the heart rate in supraventricular arrhythmias, especially atrial fibrillation. ACE INHIBITORS • Used to treat CHF • May be of use to treat systemic afterload SURGICAL CLOSURE • involved placing a restrictive band across the main PA. • proposed since pulmonary vascular disease as a result of unimpeded flow to the lungs was recognized as a dreaded complication of a ventricular septal defect • with low mortality and morbidity INDICATIONS FOR SURGICAL REPAIR • • • • Uncontrolled CHF Growth failure Recurrent respiratory infection Prolapse of aortic valve cusp The contribution of pulse oximetry to the early detection of congenital heart disease in newborns Romaine Arlettaz, Andrea Seraina Bauschatz, Marion Mönkhoff , Bettina Essers, Urs Bauersfeld Eur J Pediatr (2006) 165: 94–98 Objectives • To determine the effectiveness of a pulseoximetric screening performed on the first day of life for the detection of congenital heart disease in otherwise healthy newborns • To determine if a pulse-oximetric screening combined with clinical examination is superior in the diagnosis of congenital heart disease to clinical examination alone Methods • Study design: prospective multi-centre study • Zurich, Switzerland; May 2003 to May 2004 • Population: infants above 35 weeks of gestation (n=3,262) Methods Results Results Conclusion • Postductal pulse-oximetric screening in the first few days of life is an effective means for detecting cyanotic congenital heart disease in otherwise healthy newborns