* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Early Management of the Infant with Suspected
Management of acute coronary syndrome wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Heart failure wikipedia , lookup
Aortic stenosis wikipedia , lookup
Electrocardiography wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Myocardial infarction wikipedia , lookup
Atrial septal defect wikipedia , lookup
Congenital heart defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
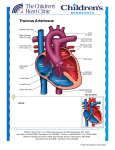
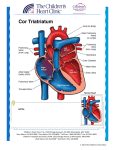
Diagnosis and Early Management of the Infant with Suspected Congenital Heart Disease Introduction • Congenital heart disease occurs in 1% of liveborn infants • Almost 1/2 of all cases of congenital heart disease are diagnosed during the 1st week of life • The most frequently occuring anomalies seen during the 1st week are: PDA, D-transposition of the great arteries, hypoplastic left heart syndrome, TOF, and pulmonary atresia Indications for Fetal Echocardiography Maternal Risk Factors Associated With Congenital Heart Disease • Congenital heart disease • Cardiac teratogen exposure – Lithium – Amphetamines – Alcohol – Anticonvulsants: phenytoin, valproic acid, carbamazepine, and trimethadione – Isotretinoin Maternal Metabolic Disorders or Infection • • • • • Diabetes mellitus PKU Hyperthyroidism Lupus, collagen vascular disease Rubella, CMV, Coxsackie, Parvovirus Fetal Risk Factors Associated With Congenital Heart Disease • Trisomies, Turner’s syndrome, abnormal karyotype • Congenital malformations: duodenal atresia, TEF, omphalocele, diaphragmatic hernia, renal dysgenesis, and hydrocephalus • Fetal arrhythmias • IUGR • Nonimmune hydrops • ?2 vessel cord Cyanosis • Etiology: CV, pulmonary, airway obstruction, neurological, neuromuscular, or hematological (methemoglobinemia or polycythemia) • Infants can appear cyanotic when the deoxygenated Hgb concentration is at least 3g/dL; it is not related to the percent saturated • 2 babies with sats of 80%: one with a hgb of 20g/dL and 4g/dL of desaturated hgb will be cyanotic, but an anemic infant with 10g/dL with 2g/dL deoxygenated hgb will not be cyanotic Evaluation • ABC’s • PE: murmur, pulses, precordium, respiratory status, HSM, color, capillary refill • 4 ext BPs: if SBP >10mmHg in right hand compared to lower ext, concerning for arch anomaly (though if normal may not rule it out) • Pre/post ductal saturations: if see a difference >5%, concerning for PPHN or left heart abnormalities Evaluation (Continued) • Hyperoxia test: baseline pre-ductal ABG when infant in room air, then repeat on 100% FiO2 • Reason for ABG and not just sats: with a saturation of 100%, you can have a PaO2 of 80 or 300; very different • CXR: cardiomegaly; normal, increased, or decreased pulmonary vascularity • EKG • Echo Interpretation of hyperoxia test: From Harriet Lane Handbook FiO2= 0.21 PaO2 (%sats) FiO2 =1.00 PaO2 (%sats) PaCO2 Normal 70 (95%) >200 (100%) 35 Pulmonary Dz 50 (85%) >150 (100%) 50 Neurologic Dz 50 (85%) >150 (100%) 50 Methemoglobinemia 70 (95%) >200 (100%) 35 Cardiac Dz Separate circulation (T GA no VSD) Restricted PBF ( TA +PS, PA, PS + no VSD, TOF) <40 (<75%) <50 (85%) 35 < 40 (<75%) <50 (<85) 35 <150 (<100%) 35 Complete mix no restricted PBF 50 (85%) (Truncus, TAPVR, Single Vent, T GA +VSD, TA no PA or PS) PPHN PFO no R->L shunt PFO + R->L shunt Preductal Post ductal 70 (95%) <40 (<75%) <40 (<75%) <40 (75%) Variable Variable 35-50 35-50 Specific Heart Disease Abnormalities Cyanotic With Decreased Pulmonary Blood Flow • • • • • • Tetrology of Fallot Ebsteins Anomaly Tricuspid Atresia with PA or PS Pulmonary atresia with intact septum Critical pulmonic stenosis PPHN Right Sided Obstructive Lesions • • • • • • • Cyanosis No respiratory distress Normal pulses and perfusion Single second heart sound Murmur Moderate to marked hypoxemia CXR: normal to large sized heart, decreased pulmonary blood flow (PBF) Tetralogy of Fallot Tetrology of Fallot Ebstein’s Anomaly Ebstein’s Anomaly Tricuspid Atresia Tricuspid Atresia EKG : QRS axis •Tricuspid atresia with PS or PA with intact ventricular septum: superior (0— -90) •Critical PS or PA : 0 to 90 degree quadrant •TOF and TOF with PA: 90-180 degree quadrant Cyanotic With Increased Pulmonary Blood Flow • d-Transposition of the great vessels • Truncus arteriosus • Total anomalous pulmonary venous return, above diaphragm • Single ventricle • Endocardial cushion defect Inadequate Mixing Lesions • • • • • • • Cyanosis Mild tachypnea Normal pulses Single heart sound Murmur ABG: marked hypoxemia, + acidosis CXR: cardiomegaly, normal or increased PBF Transposition of the Great Arteries d - Transposition of the Great Vessels Truncus Arteriosus Truncus Arteriosus Lesions with Poor Gas Exchange • • • • • • Cyanosis Marked tachypnea Fair perfusion, normal pulses May or may not have a single heart sound May or may not have a murmur CXR: normal heart size, pulmonary congestion Total Anomalous Pulmonary Venous Return Total Anomalous Pulmonary Venous Return Left Sided Obstructive Lesions • • • • • Coarctation of aorta, interrupted aortic arch Hypoplastic left heart syndrome Aortic stenosis Mitral stenosis Total anomalous pulmonary venous return, below diaphragm Left Sided Obstructive Lesions • • • • • • • • • Grey or ashen color Tachypnea Poor perfusion Decreased pulses/differential pulses Single second heart sound Murmur + gallop Hepatomegaly ABG: metabolic acidosis CXR: cardiomegaly with increased PBF Coarctation of the Aorta Hypoplastic Left Heart Syndrome Hypoplastic Left Heart Syndrome Aortic Stenosis Acyanotic With Increased Pulmonary Blood Flow • • • • VSD ASD PDA Endocardial cushion defect Ventricular Septal Defect Ventricular Septal Defect Atrial Septal Defect Atrioventricular Canal Patent Ductus Arteriosus Initial Stabilization • ABC’s: Volume resuscitation, ionotorpic support, correction of metabolic acidosis, r/o sepsis • Intubate if needed, titrate Fi02 to keep Sp02 80%85% to prevent pulmonary overcirculation • Placement of umbilical lines • Infants who present in shock within the first 3 weeks of life, consider ductal dependent lesions • Use of PGE1 (0.025 to 0.1mcg/kg/min) Stabilization for Transport • • • • Reliable vascular access Intubation if on PGE1, OG placement Oxygen delivery, Sp02 Monitor HR, tissue perfusion, blood pressure, and acid-base status • Calcium and glucose status (increased risk for DiGeorge) Prostaglandin E1 • Failure to respond: diagnosis incorrect, older infant with unresponsive ductus, ductus absent, obstructed pulmonary venous return • Clinical deterioration after PGE1: obstructed blood flow out of pulmonary veins or left atrium, HLHS with restrictive FO, TGA with intact ventricular septum and restrictive FO, obstructed TAPVR, mitral atresia with restrictive FO PGE 1 - Side Effects • Common: Apnea, fever, leukocytosis, cutaneous flushing, and bradycardia. • Uncommon: seizures, hypoventilation, hypotension, tachycardia, cardiac arrest, sepsis, diarrhea, DIC, fever • Rare: urticaria, bronchospasm, hemorrhage*, hypoglycemia, and hypocalcemia *inhibits platelet aggregation