* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Uses, Indications and Types of Pacemakers Available to
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Myocardial infarction wikipedia , lookup
Jatene procedure wikipedia , lookup
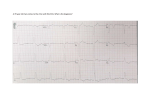
Electrocardiography wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
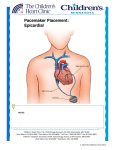
Pacemakers: The Recommendations and Guidelines for our patient population today. By: Michelle Miller OMSIII Millcreek Hospital May 31, 2006 Objectives and Learning Topics • Recommendations for Pacemaker Therapy • Types of Pacemakers • The most appropriate Pacemakers for each condition • Contraindications and Warnings Pace yourself for the Facts on Pacemakers. • First Pacemaker was implanted in 1958 • In the USA 300,000 people have pacemaker • • • implants per year. Worldwide 900,000 people have pacemaker implants per year. First Pacers were Fixed Rate Pacers today we use Rate Responsive Pacemakers. Most Conditions Requiring Pacers are Bradyarrythmias/Tachyarrythmias. Class Recommendations from the ACC/AHA for Pacemaker Therapy • Class I: Conditions for which there is evidence and/or general agreement that a given procedure or treatment is beneficial, useful, and effective. • Class II: Conditions for which there is conflicting evidence and/or a divergence of opinion about the usefulness/efficacy of of a procedure or treatment. Class Recommendations Continued • Class IIa: Weight of evidence/opinion is in favor • • of usefulness/efficacy Class IIb: Usefulness/ efficacy is less well established by evidence/opinion Class III: Conditions for which there is evidence and/or general agreement that a procedure /treatment is not useful/ effective and in some cases may be harmful. Levels of Evidence that support recommendations of Pacemaker Therapy – Level A: Data derived from multiple randomized clinical trials involving a large number of individuals – Level B: Data derived from a limited number of trials involving comparatively small numbers of patients or from well-designed data analysis of nonrandomized studies or observational data registries – Level C: Consensus of expert opinion was the primary source of recommendation Overview of “A BAD BEAT STORY” • • • • • • • • • • AV block Bifascicular and trifascicular block AV block associated with myocardial infarction Sinus node dysfunction Hypersensitive Carotid Sinus Syndrome (CSS) Vasovagal Syncope (VVS) Tachyarrhythmias/Prevention of Tachycardias Hypertrophic Cardiomyopathy Pacing after cardiac transplantation Children and adolescents with Congenital Heart Conditions. Symptomatic Indications for Pacer Therapy • Syncope or pre-syncope • Dizziness • Congestive heart failure • Mental confusion • Palpitations • Shortness of breath • Exercise intolerance Recommendations for Pacemaker Therapy In AV Block • Class I: 1.)Third Degree Block and Type II second-degree AV block at any anatomic level, associated with any one of the following conditions: -Bradycardia with symptoms (C) -Arrhythmias and other medical conditions that require drugs that result in symptomatic bradycardia. (C) -documented periods of asystole greater than or equal to 3.0 seconds or any escape rate less than 40 BPM in awake or symptom free pts. (B,C) Continued AV Block Pacemaker Recommendations Class I: Third Degree Block and Type II seconddegree AV block at any anatomic level, associated with any one of the following conditions: -After catheter ablation of the AV junction. (B,C) -Postoperative AV block that isn’t expected to resolve. (C) -neuromuscular diseases with AV block, such as myotonic muscular dystrophy, Kearns-Sayre syndrome, Erb’s dystrophy, with or without symptoms, because there may be unpredictable progression of AV conduction diseases. (B) AV Block Pacemaker Recommendations • Class I : 2.)Second Degree AV Block regardless of type or site in the presence of symptomatic bradycardia. (B) • Class IIa: • 1.Asymptomatic third degree AV block. (B,C) • 2.Asymptomatic type II second-degree AV block occurs with a narrow QRS. (B) • 3.Asymptomatic type I second-degree AV block at intraor infra- His levels found at electrophysiologic study performed for other indications. (B) • 4.First or second degree AV block with symptoms of pacemaker syndrome. (B) Recommendations for Pacemaker Therapy with Bifascicular and trifascicular block. • Class I: 1. Intermittent Third Degree AV Block. (B) 2. Type II Second Degree AV Block (B) 3.Alternating Bundle Branch Block (C) Class IIA: 1.Syncope not to be due to AV block when other likely causes have been excluded. (B) 2.Incidental findings at electrophysiologic study of markedly prolonged HV interval (greater than or equal to 100 milliseconds.) (B) 3. Incidental finding at electrophysiological study of pacing induced infra-His block that is not physiologic (B) Recommendations for Permanent Pacing S/P Acute MI • Class I: 1. Persistent second-degree AV block in the His 2. 3. Purkinje system with bilateral bundle-branch block or third degree AV block within or below the His-Purkinje system s/p MI. (B) Transient advanced (second or third degree ) infranodal AV block and associated bundle branch block. (Use Electrophysiology for exact site.) (B) Persistent and symptomatic 2nd and 3rd Degree AV Block. (C) Recommendations for Permanent Pacing in Sinus Node Dysfunction • Class I: 1.Sinus node dysfunction with documented symptomatic bradycardia, including frequent sinus pauses that produce symptoms. (C) 2.Symptomatic chronotropic incompetence (C) Class IIA: 1. Sinus Node dysfunction occurring spontaneously or as a result of necessary drug therapy with heart rate less then 40 BPM when a clear association between significant symptoms consistent with bradycardia and it hasn’t been documented.(C) 2. Syncope of unexplained origin when major abnormalities of sinus node function are discovered or provoked in electrophysiologic studies.(C) Recommendations for Pacing that detect and pace to terminate tachycardias. • Class I: NONE • Class IIa: Symptomatic recurrent SVT that is reproducibly terminated by pacing in the unlikely event that catheter ablation and /or drugs fail to control the arrhythmia or produce intolerable side effects. (C) Pacing Recommendations to Prevent Tachycardia • Class I: Sustained paused – dependent VT, with or without prolonged QT, in which the efficacy of pacing is thoroughly documented. (C) • Class IIA: High risk patients with congenital long QT syndrome. (C) Recommendations for Pacing Neurocardiogenic Syncope (ex.Hypersensitive Carotid Sinus; Vasovagal Syncope) • Class I: Recurrent syncope caused by carotid sinus • • stimulation; minimal carotid sinus pressure induces ventricular asystole of more than 3 seconds duration in the absence of any medication that depresses the sinus node or AV conduction. (C) Class IIA: 1. Recurrent syncope without clear, provocative events and with a hypersensitive cardioinhibitory response. (C) 2. Significantly symptomatic and recurrent neurocardiogenic syncope associated with bradycardia documented spontaneously or at the time of the tilt table testing. (B) Recommendations for hypertrophic cardiomyopathy • Class I: Use class I indications for sinus node dysfunction or AV block.(C) Recommedations s/p Cardiac Transplant • Class I: Symptomatic bradyarrhythmias/chronotropic incompetence not expected to resolve and other Class I indications for permanent pacing.(C) Recommendations for pacing in Children, Adolescents and Patients with Congenital heart disease. • Class I: 1. Advanced 2nd or 3rd degree AV Block associated with 2. 3. 4. bradycardia, ventricular dysfunction, or low cardiac output. (C) Sinus Node Dysfunction with correlation of symptoms during age-inappropriate bradycardia. The definition of bradycardia varies with the patient’s age and expected Heart Rate. (B) Postoperative advanced 2nd and 3rd degree AV block that isn’t expected to resolve or persists at least 7 days after surgery. (B, C) Congenital 3rd degree AV Block in the infant with a ventricular rate <50 BPM or with congenital heart disease and ventricular rate < 70 BPM. (B,C) Recommendations for pacing in Children, Adolescents and Patients with Congenital heart disease continued…. • 5. Congenital third degree AV Block with a wide QRS escape rhythm, complex ventricular ectopy or ventricular dysfunction. (B) • 6. Sustained pause-dependent VT, with or without prolonged QT, in which the efficacy of pacing is thoroughly documented. (B) Recommendations for pacing in Children, Adolescents and Patients with Congenital heart disease continued…. • Class IIa: 1.Bradycardia-tachycardia syndrome with the need for long-term antiarrhythmic treatment other than digitalis. (C) 2.Congenital 3rd Degree AV block beyond the first year of life with an average heart rate less than 50 bpm, abrupt pauses in ventricular rate that are two or three times the basic cycle lenghth, or associated with symptoms due to chronotropic incompetence. (B) 3. Long-QT sydrome with 2:1 AV or 3rd Degree AV Block. (B) 4. Asymptomatic sinus bradycardia in the child with complex congenital heart disease with resting heart rate less than 40 bpm or pauses in ventricular rate more than 3 seconds. (C) 5.Patients with Congenital Heart Disease and impaired hemodynamics due to sinus bradycardia or loss of AV synchrony. (c) Types of Pacemakers • Single Chamber Pacemaker: 1. Uses 1 lead in the right atria (VDD) OR 2. Uses 1 lead in the right ventricle (VVI) • Dual Chamber Pacemaker (DDD): 1. A lead in both the Right Atria and Right Ventricle. • Biventricular Pacemaker (DDDR) / (VAT): 1. Uses three leads: One in the right atrium, one in the right ventricle and one in the left ventricle. “Fantastic 4” Factors influenced by the Pacemaker • Heart rate increase • Stroke volume maximization • Atrial based pacing • Normal ventricular activation sequence Rate Responsive Pacing in the presence of Respiratory Function. • Minute ventilation can be measured by measuring the changes in electrical impedance across the chest cavity to calculate changes in lung volume over time How a Rate Responsive Device Works! Pulse Generator Circuitry Piezoelectric crystal Battery The Leads Cathode Anode The Crystal Senses mechanical activity from the pacer and signals electrical activity Transvenous Leads Passive Fixation Lead tines are lodged Into the Trabeculae Active Fixation Leads are extended into the endocardium of the Heart, this allows for them to position anywhere in the heart. Myocardial and Epicardial leads Leads are applied directly to the heart. They are fixed to the wall by: 1.Epicardial Stab in 2.Myocardial Screw in 3.Suture on Arrythmias that require Single Chamber Atrial Pacing • Sinus Node Dysfunction with NML AV and Intraventricular Conducting System. • Paroxysmal Atrial Fibrillation. • ***Dual Chamber Pacing occurs for Sinus Node Dysfunction and PAF with there is abnormal AV conduction seen of EP studies. Arrhythmias that require Dual Chamber Pacing • 1. Sinus Sick Syndrome • 2.Chronic Second Degree Type II heart block. • 3. Chronic Third Degree Heart block • 4. Recurrent Adams Stokes Syndrome. • 5. Symptomatic Bilateral Bundle Branch Block when tachyarrhythmias and other Block causes are ruled out. Arrhythmias that require Single Chamber Ventricular Pacing 1. Significant bradycardia and Nml Sinus Rhythm with rare episodes of AV Block or Sinus Arrest. Arrhythmias that require Biventricular Pacing: 1. Chronic Atrial Fibrillation Treating Advanced CHF in pts with major intraventricular conduction defects predominantly LBBB. Rate Responsive Device: 1. Chronotropic Incompetence. Contraindications For… • 1. Dual Chamber Pacers and single chamber pacers: Not • • • indicated for Chronic Atrial Flutter/Fibrillation or Silent Atria, these particular pacers show no benefit in txt of the conditions. 2. Single Chamber Ventricular Pacer: relatively contraindicated in pt demonstrating “Pacemaker Syndrome”. 3. Single Chamber Atrial Pacing: relatively Contraindicated in pt having AV conduction compromise. 4.Rate Modulated Pacing: may be inappropriate for pt who experience angina or other symptoms of myocardial dysfunction at higher sensor driven rates. Warnings For Pacemaker Pts. • To prevent damage to the electrode/tissue interface: 1. Avoid Sources of Magnetic and Electromagnetic Radiation. -MRI -Hydraulic Shock wave lithotripsy -No therapeutic ultrasounds within 6 inches of the pacemaker. References • Gregoratos, Gabriel et al. ACC/AHA/NASPE 2002 Guideline Updatefor Implantation of Cardiac Pacemakers and Antiarrhythmia Devices. http://www.acc.org.clinical/guidelines/pacemaker/I_indications.htm 2002. • Pacemaker Implantation. http://heartpoint.com/pacemakers.html#anchor510098 • How do Pacemakers Work? British Heart Foundation. www.bhf.org.uk/hearthealth/index.asp?secID=1&secondlevel=79&th irdlevel=475&artID1632 • Pacemakers. The Cleveland Clinic Heart and Vascular Institute. http://www.clevelandclinic.org/heartcenter/pub/tests/procedures/pa cemakers.htm Review Questions 1. A 65 yo white female presents in the ER s/p syncopal episode. She states this has happened “a couple times” before. Her EKG shows atrial fibrillation with LBBB. On physical exam she has no neurologic deficits, her heart is irregularly, irregular and her lungs are CTA. Dr. D’Amico is consulted and determines that this patient would benefit from a pacemaker. Being the astute resident/student that you are you determine the best pacer therapy for this particular patient’s condition would be: A. B. C. D. E. Fixed, Single Chamber Ventricular Pacemaker Rate Modulated, Single Chamber Ventricular Pacemaker Fixed, Biventricular Pacemaker Rate Modulated, Biventricular Pacemaker Rate Modulated, Dual Chamber Pacemaker Review Questions A 55 yo hispanic male presents with his chief complaint of SOB and intermittent dizziness times 1 month. His O2 Sats at 100% on 2L NC. On physical exam there are no neurologic deficits, bradycardia, Lungs are CTA. CT was negative, but his EKG had some interesting finding the PR interval was fixed at .24 seconds and there is one dropped QRS complex. With a ratio being 2 PR intervals to 1 QRS. This type of arrhythmia is: A.Second Degree Type one AV Block (Wenkebach) B.Second Degree Type two AV Block C.Second Degree Type two Advanced AV Block D.Third Degree AV Block Review Questions Using the previous questions arrhythmia, does this pt. qualify for pacemaker therapy according to the recommendation guidelines by the ACC and AHA? A. YES B. NO