* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Ch 15: Blood Flow and the Control of Blood Pressure
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Jatene procedure wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Myocardial infarction wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Cardiac Muscle
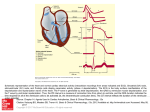
Figure 1.02. The cardiac cycle in terms of
time
Figure 1.02B. Left heart pressures
during one cardiac cycle
Figure 1.02C. Ventricular blood volume
during one cardiac cycle
Figure 1.02D. Aortic blood flow during
one complete cardiac cycle
Figure 1.02E. ECG and heart sounds
during one cardiac cycle
Figure 1.02F. Right heart pressures
during one cardiac cycle
Figure 1.05. Normal blood pressure
and oxygen saturation values
Length-tension curves (diagrams) for
skeletal and cardiac muscle
Figure 12M0. The effect of norepinephrine in
augmenting tension and rate of tension development
(Inotropicity) produced during isometric muscle
twitches
Figure 14. Bowditch effect (ie., Treppe, Staircase,
force frequency relationship)
Refractory Period:
Long, compared to skeletal muscle
Prevents tetanus, guarantees a period
of filling
Prevents ineffective tachycardia
Prevents re-entry ("circus" movement)
Two Kinds of Myocardial
Cells:
Pacemaker - exhibit automaticity (rising
phase 4 prepotential)
primary - SA nodal
reserve - SA nodal, purkinje, AV nodal
Follower - no automaticity
(stable phase 4 potential; atrium, ventricle)
Figure 3. The various ion pumps of the cell.
Figure 2M0. The three slow Ca++ channel states:
resting, active, inactive.
"d" and "f" are upper and lower gates in the channel.
Ion Channels:
Fast - initial rapid inward Na+ current. - secondary
outward K+ movement repolarization
Slow* - Ca++ moves inward, responsible for maintained
depolarization of the "plateau phase" (Phase 2)
* An increase in contraction frequency increases Ca++
movement inward, giving the "staircase" phenomenon (Treppe,
Bowditch) in cardiac muscle.
Figure 4M0. The fast sodium and slow calcium channels. The fast channel is
in its "resting" mode;
the slow channel is in its depolarization mode, ie. active state (Ca++ ions
moving through). The black dot indicates Nifedipine attachment site.
TTX = Tetrodotoxin, Nifedipine = a medically-used Ca++ channel blocker.
"m" and "h" are upper and lower gates in the Na+ channel.
"d" and "f" are upper and lower gates in the Ca++ channel.
Figure 5M0. Changes in transmembrane potential
before and during depolarization in various types of
myocardial cells.
Not all the depolarization / repolarizations look like
that in Figure 1.
Mechanisms for Changing
Pacemaker Cell
Automaticity:
Hyperpolarize/hypopolarize overdrive
suppression
Alteration of slope (rate of rise) of prepotential (diastolic potential)
Alteration of threshold; e.g. epinephrine
increases gCa++ (hypopolarizes),
acetylcholine increases gK+
(hyperpolarizes)
Factors Determining
Action Potential
Conduction Velocity:
Amplitude & rate of change of action potential increasing velocity, decreasing time
- if large, more likely to depolarize adjacent cells
Anatomy of conducting cells - increased diameter,
increases conduction velocity
- number of interconnections
- longer nexus junctions (Purkinje cells)
"Cable Properties" of the conducting system
Factors Affecting
Conduction Through the
AV Junction:
Speeds Catecholamines *
Atropine - blocks Acetylcholine
Quinidine - inhibits vagal effects
Slows Acetylcholine * *
Digitalis - central vagal (parasympathetic) stimulation
Inhibitors of acetylcholine esterase, Ca++ antagonists (e.g. verapamil)
An increased number of impulses arriving at AV junction increases
refractoriness
Various Conditions of
Muscle Contraction:
Isotonic
Unloaded
Preloaded
Afterloaded (to less than isometric)
Isometric
Comparing isotonic and isometric muscle
contractions.
+ indicates it occurs; - does not occur
Figure 6M0. Isometric and isotonic skeletal muscle
twitches following a single action potential
Figure 9M0. Isometric twitch tension as it is
influenced by preload (ie. initial length, Frank-Starling
mechanism)
Figure 10M0. Velocity of muscle shortening and power
output as each is influenced by increasing afterload
Figure 8M0. Velocity of shortening (isotonic
contraction) as it is altered by afterload and preload
Effects of Increased
Preload on Velocity of
Shortening, etc:
Increased velocity of shortening
(isotonic) at any given afterload
Unaltered Vmax at zero afterload
Increased muscle length
Increased tension development
(isometric)
Effects of Afterload on
Velocity of Shortening:
Maximum at no load
Zero at maximum load (isometric)
Intermediate with some, not maximum
load
Effects of Increased Inotropicity on Velocity
of Shortening, etc.:
Increased velocity of shortening
(isotonic) at any given afterload
Increased Vmax at zero afterload
Same muscle length
Increased tension development
(isometric), and increased rate of
contraction and relaxation
Figure 13M0. Velocity of muscle shortening and the
influence of a catecholamine such as norepinephrine
(Inotropicity) in modifying the relationship
Figure 7M0. Mechanisms for altering isometric tension
in cardiac muscle vs skeletal muscle
Factors Affecting Heart
Rate:
Leading to an INCREASE:
decreased activity of baroreceptors in the arteries, LV, and pulm. circ. (1)
inspiration (2)
excitement, anger, most painful stimuli (1)
hypoxia (1?)
exercise (1)
norepinephrine (1) , epinephrine
thyroid hormones
fever
Bainbridge reflex Leading to a DECREASE:
increased activity of baroreceptors in the arteries, LV, and pulm. circ. (2)
expiration (1)
fear, grief (2)
stimulation of pain fibers in trigeminal nerve
increased intracranial pressure (Cushing Reflex) (1)
Actions of Vagal Parasympathetic Neurons to the
Heart (through release of acetylcholine)
...... Site ................................ Action .......................................... Affecting
......
sino-atrial node ................... decreases heart rate ........... chronotropicity
atrio-ventricular node ............ slowed AV conduction ..... chronotropicity
atrio-ventricular node .. delayed conduction / increased refractoriness
……………………………………………………………..chronotropicity
Note: There are few/no parasympathetic nerve endings on the
ventricular myocardium, so while acetylcholine is a potential negative
inotrope for the ventricles, it is not released there.
Figure 2.01. Schematic of vagal escape. Acetylcholine
release from parasympathetic ends on the SA node
and AV node & Junctional tissue increases refractoriness
and depresses conduction velocity.
Intense stimulation will stop ventricular depolarization, ie.
contraction. Reserve pacemakers come into play.
Control of Cardiac
Performance: STROKE
VOLUME:
Extrinsic:
Release of the following substances from the sympathetic and parasympathetic sympathetic branches of the
autonomic nervous system, affect inotropicity:
norepinephrine (+) - neural
acetylcholine (-) - neural*
epinephrine (+) - blood borne These actions are mediated through cardiopulmonary receptors, such as the
carotid sinus (aortic) baroreceptors, carotid (aortic) body chemoreceptors, central chemo-receptors, venae
cavae/atrial volume receptors (Bainbridge), and the ventricular volume receptors.
Attention: Inotropicity (ie. contractility) and strength of contraction are not synonomous. Increased /
decreased strength of contraction can be achieved by changing preload
(ie. Frank-Starling) with no change in inotropicity. Inotropicity reflects the biochemical state within
the muscle (eg. Ca<SUP++< sup>, ATP), not simply the positioning of the thick and thin
myofilaments as determined by stretch.
Intrinsic:
Frank-Starling - through preload (heterometric autoregulation)
afterload - through increased / decreased arterial blood pressure acting on aortic valve.
Anrep effect - laboratory curiousity?
Bowditch effect } (homeometric autoregulation) (Treppe, Staircase)
environment - ischemia, O2, CO2
cardiac hypertrophy - longterm effect
* In actual fact, there are few parasympathetic fibers in the ventricular myocardium, so ACH has little
practical effect physiologically on ventricular inotropicity (contractility).
Figure 2.02. Frank-Starling (or ventricular function)
curve. See cardiac muscle length-tension curve.
The black curve defines a single inotropic state.
Major Factors Determining
Myocardial Stretch:
Total blood volume
Body position relative to the earth and
gravity pull
Intrathoracic pressure
Intrapericardial pressure
Venous tone
Pumping action of the skeletal muscle
Atrial contribution to ventricular filling
Figure 2.03. Some factors contributing to afterload. What
are shown here are the effects of increased vascular
resistance and vascular compliance. Another major factor
not shown is heart dimension, ie. a dilated heart sustains
greater afterload at the same arterial or ventricular
pressure than a smaller heart (a larger heart has larger radii
of curvature and through the Law of Laplace is at greater
mechanical disadvantage relative to internal pressure than
a smaller heart).
Major factors determining myocardial contractile
state (ie. inotropicity)
Sympathetic nerve impulses (normal)
Circulating catecholamines (normal)
Force-frequency relation (Bowditch, Treppe, Staircase) Normal)
Various natural inotropic agents (normal)
Digitalis, other non-natural inotropic agents (medical)
Anoxia, hypercapnia, acidosis (pathologic)
Pharmacologic depressants (medical / pathologic)
Loss of myocardium (pathologic)
Intrinsic depressants (normal / pathologic)
Attention: Inotropicity (ie. contractility) and strength of contraction are not synonomous.
Increased / decreased strength of contraction can be achieved by changing preload
(ie. Frank-Starling) with no change in inotropicity. Inotropicity reflects the biochemical
state within the muscle (eg. Ca<SUP++< sup>, ATP), not simply the positioning of the
thick and thin
myofilaments as determined by stretch.
Figure 2.04. Two Frank-Starling curves demonstrating
altered inotropicity; Blue - lower inotropicity; Green higher inotropicity.
Inotropic agents:
Positive:
Catecholamines (epinephrine, norepinephrine,
isoproterenol)
Ca++
Cardiac glycosides (digitalis) Negative:
Ischemia/hypoxia
Acetylcholine
Heart Failure
Stages of the cardiac
cycle
The cardiac cycle as a
loop, independent of time
Figure 2.05. Changing pump conditions: A, changing
preload; B, changing afterload; C, changing
contractile state
.
Note: Review loop-display
changing afterload,
preload remains constant
Alterations in contractile state: using systolic reserve
volume (more complete emptying), through enhanced
inotropicity
Figure 2.07. Major factors contributing to cardiac
output - Summary
Figure 2.06. Mechanisms of cardiac
hypertrophy. Concentric and Eccentric
Hypertrophy
Changes in Gene
Expression in Cardiac
Overload:
Quantitative changes:
Coordinated increase in protein (myosin, actin, myoglobin, Ca++ channels,
mitochondria, surface membrane) and RNA (m, r and t) synthesis.
Regulated at a transcriptional and at the translational level.
Adaptational, because it multiplies contractile units and decreases wall
stress. Qualitative changes:
Several shifts in isoforms (myosin, creatine kinase, actin, tropomyosin,
LDH, Na+-K+, ATPase, and SR protein).
Due to an isogene change in expression (myosin).
Adaptational because it decreases Vmax. and improves heat production.
Figure 10. Velocity of muscle shortening and power
output as each is influenced by increasing afterload
Ejection Fraction
EF = (EDV - ESV) / EDV
or
EF = SV / EDV, e.g. EF = 100 ml / 150 ml = 0.66
Note: SV = EDV - ESV
Figure 2.09. Assessment of ventricular performance.
PEP, LVET, and the ratio of PEP / LVET.
Figure 2.08. Factors
affecting pre-ejection
period
Figure 2.10. Range of ejection fractions. The normal range
may extend to 0.82 or 0.84.
Values below 0.15 are usually incompatible with life.
Note: The heart wall may be said to display normal kinesis,
hypokinesis, hyperkinesis, akinesis (no motion), dyskinesis
(paradoxical wall motion).
Figure 3.01. Blood flow distribution and arteriovenous
oxygen differences. The term "oxygen content" actually
means
"oxygen
concentration".
Arterial O2 concentration is constant, while venous O2
concentration varies from organ to organ, tissue to tissue
Ischemia
Increased A-V O2 diff. at rest usually
indicates ischemia. Ischemia is relieved by:
increasing blood flow
decreasing O2 consumption Increased A-V
lactate indicates inadequate flow; heart
usually uses lactate, in ischemia it produces
lactate
The concept of Cardiac
Reserve
Figure 3.02. The concept of
cardiovascular reserve. Cardiac
Output is in units of liters
Fick Equation:
Cardiac output (L/min.) = O2 uptake (ml
O2/min.) / A-V O2 diff. (ml O2/L blood)
For Example: C.O. = 250/ (0.19 - 0.14) = 5100
ml/min.
O2 uptake = 250 ml/min.; Arterial O2 content =
0.19 ml/ml; Venous O2 content = 0.14 ml/ml
Figure 3.03. A dye-dilution
curve
Figure 3.04. Effects of different levels
of exercise (work) on cardiovascular
function
Figure 3.05. Redistribution of cardiac
output with increased exercise /
workload
Figure 3.06. Specific blood
flow in various organs and
tissues
Figure 3.07. The coronary
vessels
Figure 3.11. An angiogram of normal coronary vessels in an opened
heart preparation (vessels filled with radiopaque material). On right
is the horizontal main right coronary artery with small dscending
twigs. On the left is the major left descending ramus and the
horizontal major left circumflex ramus. Between these two are
several large diagonal branches. The vessels show progressively
diminishing lumina with no irregular narrowings or obstructions.
Thallium Study
Examine the images below obtained during exercise
stress and at rest for a normal patient. Note the
uniform distribution in the walls of both right and left
ventricle
Figure 1. The conduction system for the cardiac action potential. Normally
the SA node depolarizes first and then the rest of the atria. After a delay at
the AV junctional tissue, the action potential is conducted down the AV node,
to the AV bundle, to the bundle branches, to the Purkinje fibers, and then to
the right and left ventricles.
Figure 1M0. Electrophysiologic changes during the
cardiac cycle, including threshold current,
transmembrane potential and ion conductances over
time. The circled numbers identify the five phases of
the process.
The 5 Phases of Myocardial Cell
Electrophysiology (follower cells only):
Phase 4 Polarized Cell; (-) inside, (+) outside; due mainly to Na+ & K+ ion
positioning and higher permeability of membrane to K+, allowing loss
of intracellular (+) charge.
Phase 0 Cell Depolarization; greatly increased membrane permeabilty to Na+
ions, which rush in through fast channels, down conc. gradient,
reversing cell polarity (fast current).
Phase 1 Partial Repolarization; loss of Na+ conductance, & transient influx of Clions and outflow K+ ions.
Phase 2 Plateau; due to the slow inward flow of Ca++ ions through slow
channels (i.e. increased Ca++ conductance) (also some inward
movement of Na+ through slow channels and outward movement of
K+). Phase 2 includes most of the absolute refractory period.
Phase 3 Rapid Repolarization; decreased Ca++ conductance and increased K+
conductance, thus K+ moves out; inside of cell again becomes (-)
relative to outside; Na+/K+ pump re-establishes distribution of ions.
Supranormal excitabilty present early in phase 3, thus greatest chance
of ectopic beat.
Table 6. HIERARCHY OF PACEMAKERS
BASED ON INTRINSIC FIRING RATES
________________________________
_______________________
Sinoatrial Node .............................. 70 per min.
Atrioventricular Node .................. 60 per min.
Ventricle ....................................... 30-40 per min.
__________________________________
_____________________
Figure 7. Sequence of depolarization / repolarization of the
heart.
Figure 2. Sequence of cardiac excitation and associated changes in
the ECG.
Figure 3. The Einthoven Triangle, showing Leads I, II
and III.
Figure 4. A moving dipole and how it is
"sensed" in front, behind and at oblique
angles
Figure 11. Configuration of the standard limb leads,
situated in the frontal (coronal) plane.
Figure 12. Configuration of the augmented
limb leads, situated in the frontal (coronal)
plane.
Figure 13. Configuration of the precordial (chest)
leads, situated in the transverse (horizontal) plane.
Figure 5. Standard terminology for the ECG (Lead aVf, 75
beats/min.).
Figures 9. Method for accurately determining
mean electrical axis of the heart (ventricles)
- Step 1.
Figures 10. Method for accurately determining mean
electrical axis of the heart (ventricles) - Step 2. Go to
Step 1
Figure 8. Electrocardiograms of two individuals, one
sedentary and one an endurance athlete (Standard paper
speed 25 mm/sec., large horizontal squares 200 msec.,
small squares 40 msec.)
Figure 6. Comparison of the ECG's of an office worker
and an athlete. (Standard paper speed 25 mm/sec.,
large horizontal squares 200 msec., small squares 40
msec.)
Figure 14. Normal sinus rhythm. Impulses originate at
the SA node at the normal rate. All complexes are
evenly spaced; rate 60 - 100/min. PR interval 120 - 200
msec
Figure 15. Sinus bradycardia. Impulses originate at
the SA node at a slow rate. All complexes are normal,
evenly spaced; rate <60/min. PR interval 120 - 200
msec.
Figure 16. First degree AV block. Fixed but prolonged
PR interval. P wave precedes each QRS complex but
PR interval, although uniform, is >0.2 sec. (>5 small
boxes).
Figure 17. Second-degree heart block: Mobitz I or
Wenchebach. Progressive lengthening of the PR
interval with intermittent dropped beats.
Figure 21. Third-degree (complete) heart (AV) block. There is no
relationship between P waves and QRS complexes: QRS rate is
slower than P wave rate. Impulses originate at both the SA node (P
waves) and below the site of block in the AV node (junctional
rhythm) conducting to the ventricles. Atria and ventricles depolarize
independently, QRS complexes are less frequent; regular at 20 to
40/min but normal in shape
Figure 22. Third-degree (complete) heart (AV) block. There
is no relationship between P waves and QRS complexes:
QRS rate is slower than P wave rate. Impulses originate at
SA node (P waves) and also below the site of block in
ventricles (idioventricular rhythm). Atria and ventricles
depolarize independently, QRS complexes are less frequent;
regular at 20 to 40/min but wide and abnormal in shape.
Figure 18. Junctional rhythm. Impulses originate in the AV node or
AV junctional tissue, with retrograde and antegrade transmission.
In this example, retrograde transmission is taking place into the
atria, giving an inverted P wave. The ventricular rate is slower than
with sinus rhythm and the QRS is narrow. If there is also sinus node
depolarization, a normal-appearing P wave may be present. If a
wandering pacemaker is present in the atria, inverted P waves can
precede the QRS complex
Figure 19. Idioventricular rhythm. No P waves
(ventricular impulse origin). Rate <40 / min.; QRS >
0.10 sec.
Figure 20. Intraventricular conduction defect (IVCD),
including right or left bundle branch block. Wide QRS
(2-1/2 small boxes), often notched, preceded by P
wave with normal PR interval.
Figure 23. Wandering atrial pacemaker. Impulses
originate from varying points in atria. Variation in
wave contour, PR interval, PP and thus RR intervals.
Figure 24. Atrial flutter. Impulses travel in circular
course in atria, setting up regular, rapid (220 to
300/min.) flutter (F) waves without any isoelectric
baseline. Ventricular rate (QRS) is regular or irregular
and slower depending upon the degree of block.
Figure 25. Atrial fibrillation - impulses take random,
chaotic pathways in atria. Baseline coarsely or finely
irregular; P waves absent. Ventricular response (QRS)
irregular, slow or rapid
Figure 26. Ventricular tachycardia. Arrow shows
slowed conduction in the margin of the ischemic area,
which permits a circular course of impulses and reentry
with
rapid
repetitive
depolarization.
Figure 27. Ventricular fibrillation.
Figure 28. The effect of increases in
serum K concentration on the ECG
the end