* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
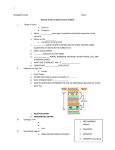
Download Growth Curve (four phases)
History of virology wikipedia , lookup
Horizontal gene transfer wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Quorum sensing wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Microorganism wikipedia , lookup
Trimeric autotransporter adhesin wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Phospholipid-derived fatty acids wikipedia , lookup
Antibiotics wikipedia , lookup
Disinfectant wikipedia , lookup
Human microbiota wikipedia , lookup
Triclocarban wikipedia , lookup
Marine microorganism wikipedia , lookup
Bacterial taxonomy wikipedia , lookup
Biological Characteristics of Bacteria •The Growth, Survival & Death of Microorganism •Cultivation of Microorganism •Microbial Metabolism The growth of microorganisms Growth is the orderly increase in all the components of an organism such as size and/or population number. The rule for bacteria growth can be described as single cell dynamics and population dynamics Growth: single cell dynamics Bacteria multiply by binary fission, the process in which a parent cell splits into two daughter cells with approximately equal size. a. Bacterial cell first can been seen to enlarge or elongate. a b. Then followed by the formation of transverse membrane and new cell wall. b c. The new membrane and cell wall grow inward from the outer layers. c d. The cell divided into two daughter cells. d Growth: single cell dynamics •Under optimal conditions, the average time required for a population of bacteria to double in number (for complete cell division) is called as generation time or doubling time. •The generation time for many common bacteria is 20-30 min, for a few of slow-growing bacteria such as Tuberculosis bacteria might be up to 18-20 h. Growth: population cell dynamics •When microorganisms are grown, due to some factors such as nutrient limitation and waste accumulation, growth rate cannot maintain for a long time. •If a liquid medium is incubated with microbial cells, and the number of viable bacterial cells per milliliter is measured and plotted, we can obtain a curve that called as growth curve. •Normally characterized by the phases lag, log (or exponential) growth, stationary growth, and death. How to Graph Bacterial Growth (i) (I) Measuring the numbers of bacteria. Common methods include: a) Turbidity: to measure the total bacteria (live and dead) in liquid cultures. This is usually quantitated with a spectrophotometer, the absorption wavelength at 600 nm will be measured. b) Colony counting method: that means counting the colony numbers on a medium plate after inoculated with a known volume of bacterial liquid culture. Measuring total bacteria (live + dead) in liquid culture——Turbidity (Cloudiness) The cloudiness of a liquid media caused by bacteria growth that are generally invisible to the naked eye, similar to smoke in air. Measuring viable bacteria colony A visible cluster of bacteria growing on the surface of or within a solid medium, presumably cultured from a single cell How to Graph Bacterial Growth (ii) (II) Plotting the log of turbidity or number of living cells versus time is referred to as the growth curve (four or six phases): Growth Curve (four phases) Growth curve (six phases) A: lag phase, B: acceleration phase, C: log (exponential) phase, D: deceleration phase, E: stationary phase, F: death phase Y-axis presents the log number of living cells X-axis presents the period of time (usually in hours) The curve can be divided into six phages represented by the letters A-F What are the characteristics of bacteria in each phase? Growth curve (four phases) •The Lag Phase (A and B): Bacteria are becoming "acclimated" to the new environmental conditions (pH, temperature, nutrients, etc.) (A). Enzymes and intermediates are formed and accumulate until they are present in concentrations that are permit growth (B). An increase in bacterial mass per unit of volume, but no increase in cell count. The metabolism of the bacteria adapts to the conditions of the nutrient medium. Growth curve (four phases) •The Exponential/log Phase (C): Conditions are optimal for growth. The living bacteria population increases rapidly with time at an exponential growth in numbers, and the growth rate increasing with time. The bacteria are suitable for biochemical and morphological identification, The bacteria are suitable to use for drug sensitivity test Growth curve (four phases) •The Maximum Stationary Phase (D and E): With the exhaustion of nutrients and accumulation of metabolic wastes, the growth rate has slowed to the point where the growth rate equals the death rate (D). Effectively, there is no net growth in the living bacteria population (E). The bacteria produce spores, toxins (e.g. exotoxin) and antibiotics. Growth curve (four phases) •The Decline Phase (F): The living bacteria population decreases with time, due to a lack of nutrients and toxic metabolic by-products. In many cases (but not always) the bacteria autolyse (during the death phase) and the turbidity decreases. Growth curve maximum retardation E Growth rate A Lag Zero B Acceleration Increasing C Exponential /Log Constant D Retardation Decreasing E Maximum stationary Zero F Decline/death Negative D F C Section Phase /exponential growth /decline B A acceleration Biological Characteristics of Bacteria • The Growth, Survival & Death of Microorganism • Cultivation of Microorganism • Microbial Metabolism What are the requirements for bacterial growth? Bacterial chemical components • Water: free water and compound water. • Inorganic salt: phosphus, potassium, magnesium, calcium, nitrium, etc. • Protein: 50-80% of dry weight according bacterial kinds and age. • Sugar: mainly distributing in cell wall and capsule. • Lipids: composed of lipid, fatty acid, wax, etc. • Nucleic acid: RNA and DNA. Sources of metabolic energy • fermentation An enzyme-induced chemical change in organic compounds that takes place in the absence of oxygen. The change usually results in the production of organic acids and energy • respiration The process cells use to convert the energy in the chemical bonds of nutrients to ATP energy. Aerobic respiration Anaerobic respiration Sources of metabolic energy •photosynthesis Reduction of an oxidant via a specific series of electron carriers establishes the proton motive force. Respiration: the energetically favorable oxidation of organic matter by an electron acceptor such as oxygen Photosynthesis: the reductant and oxidant are created photochemically by light energy absorbed by pigments in the membrane Bacterial Nutrition and Growth •Nutrient Requirements: Water Carbon source (C) Nitrogen source (N) Inorganic salts Growth factors Sulfur source (S) Phosphorus source (P) •Environmental factors for bacteria growth: Temperature Gas (oxygen) pH Osmotic pressure Nutrient Requirements 1) Carbon source Based on their source of carbon including nitrogen, bacteria are divided into two groups : Autotrophs and Heterotrophs. Autotrophs: This group of bacteria has a more complete enzyme system so they can obtain energy and various nutrients from simple compounds such as carbon from CO2. None of these organisms are pathogenic ! Heterotrophs: This group of bacteria has a simpler set of enzymes so they must use organic carbon for growth. It can be further divided into: Parasitic bacteria: grow in and feed on a different organism. Saprophytic bacteria: obtain their nutrients from dead or decaying organic matter. Most of pathogenic bacteria are parasitic bacteria. Some saprophytic bacteria cause disease by acting on food to produce toxins. Nutrient Requirements 2) Nitrogen source A major component of proteins, nucleic acids, and other compounds. Nitrogen fixation: The ability to assimilate N2 reductively via NH3. This process requires a large amount of metabolic energy and is readily inactivated by oxygen. It is a property unique to prokaryotes, especially in divergent bacteria, that have evolved quite different biochemical strategies to protect their nitrogen-fixing enzymes from oxygen. Nutrient Requirements 3) Mineral source In formulating a medium for the cultivation of most microorganisms, it is necessary to provide sources of potassium, magnesium, calcium, and iron, usually as their ions (K+, Mg2+, Ca2+, and Fe2+). Required for appropriate osmotic pressure. Additionally, also needed to stabilize or activate certain enzymes. Nutrient Requirements 4) Growth factors A growth factor is an organic compound which a cell must contain in order to grow but unable to synthesize. A number of different growth factors are required for bacterial growth such as amino acids, purines, pyrimidines, and some certain vitamins. Environmental factors for bacteria growth 5) pH Most bacteria have a narrow optimal pH range. Neutralophiles: grow best at neutral pH (pH 6.0-8.0, 7.5) Some can survive/grow - Acidophiles (pH 1.0-6.5 ) - Alkaliphiles (pH 9.0-11 ) Internal pH is regulated by a set of proton transport systems in the cytoplasmic membrane, including a primary, ATP-driven proton pump. Environmental factors for bacteria growth 6) Temperature Different microbial species are vary widely in their optimal temperature ranges for growth: Mesophilic forms 30-37 ℃ All human microbial pathogens belong to this forms Psychrophilic forms 15-20 ℃ Thermophilic forms 50-60 ℃ High Temperature static action cidal action 6) Temperature Heat-shock response: a transient synthesis of a set of "heat-shock proteins," when exposed to a sudden rise in temperature above the growth optimum. These proteins appear to be unusually heatresistant and to stabilize the heat-sensitive proteins of the cell. Cold shock response: the killing of cells by rapid as opposed to slow cooling. Environmental factors for bacteria growth 7) Gas Requirements According to the requirement of O2 during bacteria growth, bacteria can be divided into four groups: Aerobic Anaerobic 1. Obligate aerobe: Growth No growth 2. Microaerophile: Growth at low O2 No growth 3. Obligate Anaerobe: No growth Growth 4. Facultative aerobe: Growth Growth Obligate aerobes • grow in presence of oxygen • no fermentation • oxidative phosphorylation (Electron transfer through the cytochrome system liberating free energy which is transformed into high-energy phosphate bonds) Microaerophile (Microaerophilic bacteria) grow – low oxygen (2-5%) killed – high oxygen Obligate anaerobes • • • • no oxidative phosphorylation fermentation killed by oxygen lack certain enzymes: 2+superoxide dismutase O +2H H2O2 catalase H2O + O2 peroxidase H2O /NAD NADH Facultative anaerobes • fermentation and oxidative phosphorylation • aerobic respiration • survive in oxygen Cultivation methods Concerning two parts: I. Choice of suitable medium II. Isolation of bacteria for pure culture I. Choice of suitable medium Medium (I) (1) raise a crop of cells of a particular species that is on hand; (2) determine the numbers and types of organisms present in a given material; (3) isolate a particular type of microorganism from a natural source. Medium (I) • A classification of media based on their respective usages: Basic medium Enrichment medium Selective medium Differential medium Basic medium: supplies only the minimal nutritional requirements of a particular microorganism. e.g. broth Enrichment medium: Nutrient broth, nutrient agar, peptone water are commonly used in enrichment media. e.g. blood agar plate Selective medium: Supports the growth of desired bacteria while inhibiting the growth of many or most of the unwanted ones, either by adding one or more selective agents which is a "poison" to the unwanted bacteria but not harmful to desired bacteria, or by including certain nutrients for the desired ones and deleting certain nutrients for the unwanted ones. e.g. L-G medium for M. tuberculosis Differential medium This medium allows two or more different bacteria to grow, but it contains dyes and/or other components upon which different bacteria act in various ways to produce a variety of end products or effects (usually by showing different colors). e.g. SS agar Medium (II) • Classification according to physical condition (according to the content of solidifying agent): liquid medium Solid medium Semi-solid medium • Agar •The major solidifying agent used in bacteriological media. • An polysaccharide gum that extracted from certain red algae. • Agar can be dissolved at 100 C, and solidified at about 43 C. •Added 1.5-2.0% of Agar for solid plates or slanted media, 0.1-0.5% for semisolid media. Usage of different media • liquid medium Used to obtain a large number of bacteria, and to perform drug sensitivity test and bacterial growth assay. The bacteria grown in liquid medium will display some certain characteristics of bacteria (alignment and clustering) that can't be seen easily in solid media. • Phenomena of bacterial growth in liquid medium (i) forming cloudiness in broth (growth with uniform turbid pattern), (i) forming a ring at the top of broth (growth with suspension pattern) (ii) forming sediment at the bottom of broth (growth with sedimentary pattern) i ii iii Solid medium Used to obtain a large number of bacteria, isolate identical clones of bacteria (colony), and to perform drug sensitivity test. A colony is a bacterial cluster which propagated (multiplied) from a single initial bacterial cell (So a colony is a pure bacterial culture). Colony can be used to determine the original bacterial numbers by counting colonies and to evaluate viability of bacteria (colony forming units, CFU). Semisolid medium Test the motility of bacteria (a bacterium has a flagellum or flagella whether or not ) Positive: bacteria grow into the medium give cloudiness to the medium. Negative: bacteria grow in situ. Cultivation methods II. Isolation of bacteria in pure culture •In order to study the properties of a given bacterium, it is necessary to handle it in pure culture (free of all other types of bacteria). •Several methods are used to get pure-culture purpose: a) Plating pour-plate method Streaking b) Dilution Pour-plate method A suspension of bacteria is mixed with melted agar at 50 C and poured into a dish. When the agar solidifies, the bacterial cells are immobilized in the agar and grow into colonies after incubation. If the suspension was sufficiently dilute, the colonies will be well separated. Pour Plate Streaking Procedure: 1. Flame the loop and streak a loopful of broth culture as at A in the diagram. 2. Reflame the loop and cool it. 3. Streak as at B to spread the original inoculum over more of the agar. 4. Reflame the loop and cool it. 5. Streak as at C. 6. Reflame the loop and cool it. 7. Streak as at D. 8. Incubate the plate inverted. Streaking Dish Wire loop Colony (pure culture) By spreading a large amount of bacteria over the surface of a plate, the amount of bacteria is diluted and individual cells are spread. From these individual cells a single colony arises. • Dilution •A much less reliable method for pure culture. a) The suspension is serially diluted and samples of each dilution are plated. b) If only a few samples of a particular dilution exhibit growth, it is presumed that some of these cultures started from single cells. Steps in isolation and identification •Sample collection •Isolation (pure culture) •Identification (microscopy and biochemical) •Classification (species, type) •Susceptibility to antibiotics • Sample collection: Depending on the disease suspected, different types of specimens can be taken for culture, e.g. stool for diarrhoea, and urine for urinary tract infection. • Susceptibility to antibiotics A pure culture of bacteria can be tested for antibiotic resistance by evenly swabbing it over an agar plate and pressing discs of antibiotic into the agar. After a period of incubation, sensitivity or resistance to the antibiotic can be determined by measuring the zone that forms around the disc. Large zones mean the bacteria are sensitive to the drug Small or nonexistent zones are signs of resistance. Biological Characteristics of Bacteria • The Growth, Survival & Death of Microorganism • Cultivation of Microorganism • Microbial Metabolism Microbial Metabolism Metabolism refers to all the biochemical reactions that occur in a cell or organism. 1) pathways for the interconversion of focal metabolites 2) assimilatory pathways for the formation of focal metabolites 3) biosynthetic sequences for the conversion of focal metabolites to end products 4) pathways that yield metabolic energy for growth and maintenance. Microbial Metabolism The key concepts of glycolysis, Krebs Cycle, oxidative phosphorylation have been or will be discussed in biochemistry. Concentrates here are put on the products of bacterial metabolism with medical importance (e.g. bacterial pathogenesis). for laboratory diagnosis or for • Medical Important Metabolic Products 1. anabolic processes (synthesis or build up) 2. catabolic processes (decomposition or break down) Catabolic Products and Biochemical Testing a. Carbohydrate Fermentation Tests Medium: Carbohydrate fermentation broth with a Durham tube (a small inverted vial filled with the carbohydrate fermentation broth). If gas is produced during fermentation of the sugar, it is trapped at the top of the Durham tube and appears as a bubble. pH indicator: phenol red a. Carbohydrate Fermentation Tests Principle: Because the type of enzyme(s) produced by bacteria is genetically controlled, the fermented pattern of sugars may be unique to a species, but may be different between different species. Fermentation products are usually acid (lactic acid, acetic acid etc.), neutral (ethanol etc.) or gases (carbon dioxide, hyrogen, etc). a. Carbohydrate Fermentation Tests Result: positive yellow color yellow color with gas bubble negative red color, no gas bubble b. Methyl Red (MR) Test Medium: contains glucose and peptone Indicator: methyl Red All enterics oxidize glucose for energy; however the end products vary depending on bacterial enzymes. b. Methyl Red (MR) Test For bacteria (e.g. E. coli ) that produces acids, causing the pH to drop below 4.4. When the pH indicator methyl red is added to this acidic broth it will be cherry red (a positive MR test). For bacteria (e.g. Klebsiella and Enterobacter) that produce more neutral products from glucose (e.g. ethyl alcohol, acetyl methyl carbinol). In this neutral pH the growth of the bacteria is not inhibited. The bacteria thus begin to attack the peptone in the broth, causing the pH to rise above 6.2. At this pH, methyl red indicator is a yellow color (a negative MR test). Result: c. Voges-Proskauer (VP) Test Medium: contains glucose and peptone Indicator: Barritt's A (alpha-napthol) and Barritt's B (potassium hydroxide) When these reagents are added to a broth in which acetyl methyl carbinol is present, they turn a pink-burgundy color (a positive VP test). This color may take 20 to 30 minutes to develop. E. coli does not produce acetyl methyl carbinol, but Enterobacter and Klebsiella do. c. Voges-Proskauer (VP) Test d. Citrate Utilization Test The citrate test utilizes Simmon's citrate media to determine if a bacterium can grow utilizing citrate as its sole carbon and energy source. Growth of bacteria in the media leads to development of a Prussian blue color (positive citrate). e. Indole Test The test organism is inoculated into tryptone broth, a rich source of the amino acid tryptophan. Indole positive bacteria such as E. coli produce tryptophanase, an enzyme that cleaves tryptophan, producing indole and other products. When Kovac's reagent is added to a broth with indole in it, a dark pink color develops. Indol test Methyl test VP test Citrate utilization test I M Vi C test E. coli C. perfringens I M Vi C + — + — — + — + • f. Hydrogen Sulfide (H2S ) formation To determine the ability of a bacterium to produce hydrogen sulfide (H2S) by enzymatic reaction on amino acids such as cysteine, cystine and methionine. The hydrogen sulfide combines with ferrous sulfide (Fe2S) in the triple sugar iron (TSI) agar to form a black to dark insoluble precipitate. • g. Urease Test Medium: urea agar slant Indicator: phenol red Principle: The hydrolysis of urea by urease produces ammonia and carbon dioxide. The formation of ammonia alkalinizes the medium, and the pH is detected by the color change from light orange to pink-red. Positive result: pink-red color Negative result: light orange What are the medically important anabolic products of bacteria? Synthetic Products • Pyrogens • Toxins and Invasive Enzymes • Antibiotics • Vitamins • Bacteriocins • Pigments • Pyrogens • the products of many bacteria, especially gram-negative bacteria, which resulting in fever when injected into animals or humans. • They are polysaccharides in cell wall (G+ bacteria) or LPS (G- bacteria). • They are highly resistant to high heat (not being destroyed heating at 121C for 15-20 min), but can be destroyed by heating to 250 C for 30 min. • They can be removed from most fluid materials by adsorption using special materials. • Toxins and Invasive Enzymes • According to difference on the chemical composition, toxicity, bioactivity, antigenicity and so on, bacterial toxins can be divided into exotoxin (polypeptide or protein) and endotoxin (LPS). • Invasive enzymes secreted by bacteria can help bacteria to invade host. So they contributed to the pathogenesis of bacteria. • Antibiotics • The substance produced by many fungi and a small number of bacteria that selectively kill or inhibit other organisms. • Vitamins • A few bacteria produce various vitamins, e.g. some certain bacteria growing in the intestine produce vitamin K. This action is thought to be beneficial to the host. • Bacteriocins • Substances produced by specific strains of bacteria that are lethal against other strains of the same or related species. • They are protein or lipopolysaccharide-protein complexes. • pigments • Produced by a small number of bacteria with characteristic colors. I) water soluble Pseudomonas aeruginosa can produce a green water soluble pigment, so that the color is distributed throughout the culture. II) liposoluble Staphylococcus aureus can produce a golden yellow liposoluble pigment and this color only show in their colonies. • Help to identify some of bacteria. Pseudomonas aeruginosa produces a blue-green pigment, which diffuses into the medium giving the plate a characteristic color. Staphylococcus aureus produces a golden yellow pigment and give the colonies this color. The medical significance of these products Products Medical significance pyrogen toxin Pathogenicity of bacteria Invasive enzyme Antibiotic Vitamin Treatment of infectious diseases Bacteriocin Identification of bacteria pigment Antibiotics and Antibiotic Resistance Antibiotics Antibiotics are powerful medicines that fight bacterial infection Literal translation • anti – against • biotic – living things How antibiotics work Antibiotics can be either • Broad Spectrum – Kill a wide range of bacteria e.g. Penicillin • Narrow Spectrum – Kill a specific type or group of bacteria e.g. Isoniazid, Rifampicintablets Antibiotics work in one of two ways • Bactericidal – Kills the bacteria • Bacteriostatic – Prevents the bacteria from dividing Miracle Cure? – Before the 1930s there were no treatments for bacterial infections – Following the discovery of penicillin industry started searching for more antibiotics in nature – Streptomycin was the first drug to have an effect on tuberculosis – a condition previously untreatable – Surgeons could attempt more dangerous operations Miracle Cure? Overuse of antibiotics can damage our normal/good bacteria. – Many antibiotics prescribed by the doctor are broad spectrum – These kill the body’s good bacteria as well as the bad – With the good bacteria gone there is more room for bad microbes to invade! Miracle Cure? Antibiotics resistance Many bacteria have developed the ability to become resistant to antibiotics. These bacteria are now a major threat in our hospitals. Antibiotic resistant bacteria include Methicillin Resistant Staphylococcus aureus (MRSA) Antibiotic Resistance The Causes – Overuse • Antibiotics used to treat infections when they are not needed or not effective i.e. for the flu – Misuse • Not completing a prescribed course • Using antibiotics not prescribed for you Bacterialcidal Mechanism Cell Membrane Cell Wall Mitochondria DNA Ribosomal Complex Bacterialcidal Mechanism • Damaging or inhibiting synthesis of the bacterial cell wall (penicillins, cephalosporins, monobactams, carbapenems, bacitracin, vancomycin, cycloserine, fosfomycin) • Damaging or inhibiting synthesis of the cell membrane (polymyxins) Bacterialcidal Mechanism • Metabolizing or inhibiting DNA synthesis of nucleic acids (rifampin, nitrofurantoins, nitromidazoles) • Modifying ribosomal energy metabolism (sulfonamides, trimethroprim, dapsone, isoniazid) • Inhibiting ribosomal protein biosynthesis (aminoglycosides, tetracyclines, chloramphenicol, erythromycin, clindamycin, spectinomycin, mupirocin, fusidic acid) Acquired Bacterial Resistance Virus Plasmid Acquired Bacterial Resistance • Receiving a plasmid bearing a resistance gene from another bacterium directly • Receiving a resistance gene from other bacterium by viral transfection • Chromosomal mutation • DNA scavenged from dead bacteria Mechanisms of resistance Imipenem resistant Pseudomonas aeruginosae Streptococcus pneumoniae resistance to penicillins MRSA penicillin binding protein PBP2A Tetracycline Penicillins, Cephalosporins Mechanisms of resistance • Antibiotic modification: some bacteria have enzymes that cleave or modify antibiotics: e.g. β-lactamase inactivates penicillin • Denied access: membrane becomes impermeable for antibiotic: e.g. imipenem • Pumping out the antibiotic faster than it gets in: e.g. tetracyclines • Altered target site: antibiotic cannot bind to its intended target because the target itself has been modified • Production of alternative target (typically enzyme): e.g. Alternative penicillin binding protein (PBP2a) in MRSA Loss of Antibiotic Resistance • Antibiotic resistant bacteria are at a selective disadvantage - they must expend energy and resources to manufacture proteins that confer resistance • The prevalence of resistant bacteria declines after antibiotics are withdrawn How antibiotic resistance can be prevented – Antibiotics should be the last line of defence NOT the first • Most common infections will get better by themselves through time, bed rest, liquid intake and healthy living. – Only take antibiotics prescribed by a doctor – If prescribed antibiotics, finish the course. – Do not use other peoples or leftover antibiotics • they be specific for some other infection Summary 1) Definitions: pyrogen, antibiotic and acteriocin 2) Bacteria growth curve, especially the characteristics and application of log phase and maximum stationary phase. 3) The medically important antibiotic products of bacteria 4) The requirements of bacterial growth 5) The mode of bacterial reproduction