* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
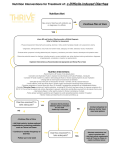
Download Probiotics and Various States of Diarrhea
Survey
Document related concepts
Lactase persistence wikipedia , lookup
Intestine transplantation wikipedia , lookup
Lactose intolerance wikipedia , lookup
Human microbiota wikipedia , lookup
Gastrointestinal tract wikipedia , lookup
Small intestinal bacterial overgrowth wikipedia , lookup
Transcript
Probiotics and Various States of Diarrhea By Lindsay Clapp-Hansen Medical Nutrition Therapy November 25, 2002 Probiotics • Microbes found in the food supply that enhance human health. • Criteria: bacteria of human origin, able to adhere to the intestinal mucosa, have potential to colonize in the GI tract, can produce antimicrobial substances, stable against bile, HCl, and other acids, enzymes, and oxygen, and determined to be safe and effective. Altered Disease States Probiotics have been thought to improve or ameliorate a plethora of states, the most commonly reported upon are: • Various states of diarrhea • Inflammatory Bowel Disease • H. Pylori Ulcers • Urinary Tract Infections • Vaginal Candida Overgrowth • Cancer of the Gastrointestinal (GI) Tract What has Scientifically Based Research to Support the Claims? After reviewing a majority of the research and literature relative to probiotic use in humans, it is clear that diarrhea is the condition most beneficially treated by probiotic therapy. This can include diarrhea associated with antibiotics, travel, gastroenteritis, lactose intolerance, and Inflammatory Bowel Disease. These areas were reviewed. Diarrhea Described Diarrhea is frequent loose stools, along with an excessive loss of fluid and electrolytes (K & Na especially), abdominal cramping, pain, and often presence of a fever. It can be acute or chronic, and is secondary to an underlying disease or condition or pathogenic bacteria within the GI tract. Types of Diarrhea 1. 2. 3. 4. Osmotic—a result of poorly absorbed nutrients that enter into the large intestine => a solute-related osmotic shift Secretory—usually a result of bacterial or viral infections, which causes excessive secretion of electrolytes and water by the intestinal epithelium Exudative– mucosal damage combined with a build up of blood, mucous, and plasma proteins in the colon Limited Contact Mucosal—caused by insufficient blending of chyme and decreased exposure to the intestinal epithelium Antibiotic Associated Diarrhea This is the most well studied area of probiotics, because antibiotic associated diarrhea is evident in 20% of all people on antibiotic therapy which provides a good sample. Cause- by the antibiotic therapy destroying the normal, health-promoting gut flora as well as the pathogenic bacteria. Result- the healthy bacteria that usually protects the GALT and the intestinal epithelium is not there, this enables pathogenic bacteria to bind to the available receptors How Probiotics Aide in Decreased Antibiotic-Associated Diarrhea: • The probiotics promote increase production of the synergistic bacteria, thus increasing the quantity in the intestine & decreasing the number of available receptor sites Antibiotics & Probiotics Tested • In 1989 the largest study on antibiotic-associated diarrhea and probiotic intervention was completed. This spurned more interest in the area. • Prospective, double-blind, placebo-controlled trial • N =180 hospital patients on antibiotics • Experimental: Received S. boulardii in conjunction with antibiotics. • Results: There was a 13% decrease in overall diarrhea symptoms when comparing the experimental to the control. 1999 Quantified Study Released A study using clear dosage levels was published in 1999. It examined 119 children (2wks-12.8 yrs) on antibiotics. Half were given a placebo and half a 2 * 10^10 colony forming units of Lactobacillus GG twice a day. This was examined over a three month period. During this time careful stool frequency and consistency logs were maintained by the parents of subjects. Results 1. There was a 11% decrease of diarrhea in the initial two weeks of probiotic therapy when comparing the experimental group to control. 2. By the third week, there was a 30% decrease difference between the two groups. Confounds • The study in 1989 was lacking in clearly quantifiable values of probiotic dose. • The study that was completed in 1999 was a break through because there were standardized amounts of probiotics given. However, the age range of children does not enable a clear dose per weight determination to be made. • In all of the studies reviewed concerning antibiotic-related diarrhea, there were one or more of the following confounds: lack of specific detail of amount and consistency of diarrhea and the quantity and viability of the probiotic strains administered. There leaves much to be researched. Conclusion for Antibiotic Associated Diarrhea • There is a basis to believe that probiotics, through competitive exclusion by the enhancement of intestinal micro flora, are able to lessen the frequency and duration of diarrhea. • More needs to be done in order to create clinically applicable recommendations. Traveler’s Diarrhea • It has been estimated that 20-50% of all people who travel are struck by diarrhea. The frequency and duration is associated with the destination and location of the traveler. • Cause: it is presently unknown, but believed to be due to a change in ingested microbial content and stress. Pathogenic E. coli is usually protagonist. • Result: unknown, however results in diarrhea. Tested Probiotic Affect on Traveler’s Diarrhea • In 1993, a study was conducted that stated 47% of Americans traveling to Mexico were able to avoid Traveler’s diarrhea when a prophylactic dosage of Lactobacillus GG was administered daily. • This study was one of many, but is in accordance with the majority of published studies. Traveler's Diarrhea Continued • Other trials conducted showed a HUGE range from >50% reduction with the supplementation of probiotics to none at all. • However, in all of the studies that compared various ages, the outcome showed diminished diarrhea within the elderly population when taking a probiotic supplement. This shows that overall GALT and immune function are related to how a person will respond to microbes. This calls for studies to be conducted on the elderly to determine if probiotics could diminish nursing home GIrelated distress. Infectious Diarrhea • Infectious diarrhea can be induced by any pathogenic virus or bacteria. Rotaviral diarrhea will be covered here. • Rotavirus attacks the GI tracts of newborns and infants, and because of this it can be well isolated and studied in relation to probiotic dosing. • Rotavirus induces biphasic diarrhea, initially osmotic and then secretory. What Probiotics Do to Combat Rotaviral Diarrhea 1. Stabilize the intestinal micro flora that’s been altered by rotavirus (through reproduction promotion) 2. The above results in reduced gut permeability, which lowers the rate rotavirus can bind to the GALT and cause gastroenteritis 3. Probiotics reduce the length of time rotavirus in the intestine (due to competitive exclusion) 4. Probiotics increase the amount of IgA that the body produces to fight infection. Key Study: Rotavirus & Probiotics • In 1997, a prospective, randomized, placebocontrolled trail was carried out to determine how Lactobacillus reuteri affected rotavirus. • Children between the ages of 6-36 months were brought into the study post admit for rotaviralassociated diarrhea • There were three groups: placebo, 1 dose of 10^10 cfu, and 1 dose of 10^7 cfu. The treatment was given once daily for five days. Results for Rotaviral Study • Results showed that the duration of diarrhea in the placebo group was 2.5 days in length as compared to 1.9 days with the 10^7 dose, and 1.5 with the 10^10 dose. • Additionally, stool cultures show that there was significant probiotic colonization in the GI tract in both test groups. • This study, as well as others, shows that there is a clear correlation between oral administration of a probiotic strain and diminished rotaviral diarrhea. • More must be researched to establish a clinically meaningful therapy. Lactose Intolerance • Lactose intolerance presents in 70-100% of adults worldwide. • Probiotics function as a lactase isomer. When probiotics deteriorate, they produce B-D-galactosidase from the cell wall. This is an isomer of lactase which then destroys ingested lactose. B-D-Galactosidase • In order for the B-D-galactosidase to appear in the GI tract, the probiotic must be ingested in a viable state, and then breakdown. • This means that frozen yogurt and pasteurized yogurt are not as effective as fresh yogurt, because they do not produce the B-D-Galactosidase. Yogurt Conundrum • So why is pasteurized yogurt tolerated? • One study states that is it the decreased intestinal transit time, which means that the lactose spends less time as an undigested molecule within the large intestine. If the lactase were to spend a longer period of time in the large intestine, fermentation and osmotic diarrhea would result. • Other studies state that pasteurized yogurt causes a delay in gastric emptying and orocecal transit time, because the probiotics and organic acids they produce result in a lower osmotic load. So now what? • There must be more research on how non-viable (aka pasteurized) probiotics alter the lactose intolerants GI tract that makes the person able to consume lactose-containing yogurt. • Over and over again the B-D-galactosidase has been seen to break down lactose, so non-heat treated yogurt is acceptable. • Overall, the viable probiotics have been seen to have a positive effect on lactose intolerant consumption of dairy. Additionally, there is some manner in which non-viable microbes are aiding in the acceptability of lactose in the intolerant individual. Inflammatory Bowel Syndrome • IBD includes both Crohn’s and ulcerative colitis. The cause of these disease states are unknown, but it is believed to be due to genetics and immunlogic deficiencies. These disease states present when there is an imbalance in the gut micro flora. • The current method of treating IDB flare ups is with antibiotics. • In 1997, a double-blind study was conducted that examined a probiotic (non-pathogenic E. coli) and an antibiotic (mesalazine). • The study included 120 adults, with inactive colitis. They were divided into the two test groups. Over a three moth period, they were asked to assess the frequency, intensity, and an overall health assessment. • Results: The results were not clinically significant, the E. coli group had a 16% rate of controlled flare up, where as the mesalazine had an 11% rate. Not Clinically Significant, but Still Significant • Although the 11% vs. 16% is not clinically different, this shows that the probiotic was nearly as effective as the antibiotic. • Because IBD patients are immunosuppressed, the reduction in antibiotic associated diarrhea would improve the overall quality of life. • By taking the probiotic therapy instead of the antibiotic, there would be commensal bacterial growth within the intestine, which would act as a barrier against ingested pathogens and promote the production of IgA immune response within the gut IBD & Probiotics • Although it seems that probiotics could at some point be an alternative therapy for IBD, it is not possible now, because standardized doses must be determined. More research must be done to determine if antibiotic-associated diarrhea in the IBD patient can be significantly reduced. • After reviewing the literature, the consensus is that probiotics as a supplement are not altering IBD significantly. Probiotic Research Overall • The studies that have been completed are limiting because there are not standardized amounts, there is a large variation in the strain used for experimentation, the viability of the microbes are not tested pre-experimentation. • More must be done so that this potentially beneficial supplement can be used in practice Conclusion • Probiotics are able to decrease the length/incidence of antibiotic-induced diarrhea through competitive exclusion. • Probiotics were seen to decrease the severity and length of traveler’s diarrhea, especially among the elderly. • Rotaviral-associated diarrhea cases were positively altered when oral probiotics were administered. Conclusion • Lactose intolerance and probiotics is still controversial. Viable probiotics clearly have a positive function. Pasteurized probiotics are an unknown area at present. • IBD is likely not significantly altered through probiotic supplementation, however probiotics could potentially be used instead of antibiotics to control flare-ups, which may decrease the incidence of antibiotic-associated diarrhea. Areas of Research • The correlation between probiotic therapy and increased production of IgA. • Determining the best strains and the quantities that are needed to support intestinal health promotion. • Research that has minimal confounds so that it will be honored by the scientific community.