* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Metabolic Changes and Nutritional Management of Surgical Patients
Survey
Document related concepts
Transcript
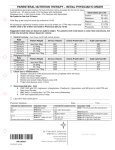
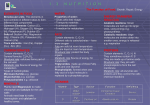
Metabolic Changes and Nutritional Management of Surgical Patients James Taclin C. Banez, MD, FPSGS, FPCS Majority of surgical patients: ► well nourished / healthy ► uncomplicated major surgical procedure ► has sufficient fuel reserve ► can withstand brief period of catabolic insult and starvation of 7 days Postoperatively: ►can resume normal oral intake ►supplemental diet is not needed Surgical Patients that Needs Nutritional Support ► To shorten the postoperative recovery phase and minimize the number of complications: 1. Chronically debilitated from their diseases or malnutrition. 2. Suffered severe trauma, sepsis or surgical complications Metabolic Changes in Surgical Patients Metabolic events brought about by STIMULI: 1. Injury 2. Starvation Metabolic response is directed to restore: 1. Homeostasis 2. Repair Metabolic Response to Starvation ► ► HYPOGLYCEMIA – is primary stimulus Hormonal Changes: increase cortisol, catecholamines, glucagon, growth hormones Primary gluconeogenic precursors by the liver & kidney: a. lactate b. glycerol c. amino acid (alanine & glutamine) ► ► Proteolysis increase due to increase CORTISOL -----> inc. urinary nitrogen first 4 days of starvation (8-12g/day = 6.25g of muscle/g of nitrogen). ► Protein catabolism for gluconeogenesis primarily comes from SKELETAL muscle, but in pure starvation other organs are involved ► In liver. CHON loss is selective; spare enzymes for gluconeogenesis and lipolysis. In pancreas and GIT, enzymes for digestion and protein for regeneration of epithelium is involved -> PARADOXICAL ► FOOD INTOLERANCE ► Rapid proteolysis of body CHON cannot proceed at 75 g/day for long, or else patient will die immediately RANDLE EFFECT. decrease urinary excretion of nitrogen 2 – 4 gm/day due to keto-adaptation of the brain decrease protein degeneration and major source of energy is FAT (90%) Metabolism of Injured Patient PHASES: 1. Catabolic phase (Ebb, AdrenergicCorticoid): immediately following surgery or trauma characterized w/ hyperglycemia, increase secretion of urinary nitrogen beyond the level of starvation caused by increase glucagon, glucocorticoid, catecholamines and decrease insulin tries to restore circulatory volume and tissue perfusion Metabolism of Injured Patient PHASES: 2. Early anabolic phase (flow, corticoidwithdrawal): tissue perfusion has been restored, may last for days to months depending on: a. b. c. severity of injury previous health medical intervention sharp decline in nitrogen excretion nitrogen balance is positive (4g/day) indicating synthesis of CHON and there is a rapid and progressive gain in weight and muscular strength Metabolism of Injured Patient PHASES: 3. Late anabolic phase: several months after injury occurs once volume deficit have been restored slower re-accumulation of CHON re-accumulation of body fat Metabolism of Injured Patient Carbohydrate Metabolism in Injured Patient: Hyperglycemia = proportional to the severity of injury Importance: 1. Homeostatic significance 2. Ready source of energy to the brain 3. Adequate delivery Metabolism of Injured Patient Carbohydrate Metabolism: Hyperglycemia: Caused by: ►Increased catecholamine (primarily), cortisol, glucagon, GH, vasopressin, angiotensin II, somatostatin and decrease insulin. ►Gluconeogenesis in liver and kidney and impaired peripheral uptake of glucose Metabolism of Injured Patient Carbohydrate Metabolism: Hyperglycemia: Insulin resistance: ►During the Ebb phase there is reduction in beta cell sensitivity to glucose due to Catecholamine, somatostatin and reduced pancreatic blood flow ►Resistance to exogenous administration on insulin in both EBB and early FLOW phases ►In middle and late Flow phase, beta cell sensitivity return to normal and it’s level is higher, but hyperglycemia persist because of continuous gluconeogenesis Metabolism of Injured Patient Carbohydrate Metabolism: ► Glucose metabolism in wounded tissue: Increase glucose uptake and lactate production because of anaerobic glycolysis due to local tissue hypoxia (+) insulin insensitivity Metabolism of Injured Patient Lipid metabolism: primary source of energy Best stimulus for hormone-sensitive lipase is CATECHOLAMINE RANDLE EFFECT is not present Metabolism of Injured Patient Protein Metabolism: Nitrogen urine excretion 30-50g/day due to proteolysis; 20% utilized for energy (calories) the rest for gluconeogenesis by liver and kidney (cortisol, glucagon, catecholamine). Primary source of protein is the skeletal muscle and the visceral organs are spared. Metabolism of Injured Patient Protein Metabolism: Ketoadaptation is inhibited ----> gluconeogenesis persist ---> proteolysis persist (INTERLEUKIN I). The degree and duration (-) nitrogen balance is related to severity of injury. The net CHON catabolism depends on the age, sex and physical condition of the patient (> in young, healthy and male) (-) nitrogen balance can be reduced by high caloric nitrogen supplement Traumatized Man Injury of any type is associated with: 1. Immobilization 2. Starvation 3. Repair the first two are associated with reduction in energy requirement. While the third is associated w/ increase energy requirement The amount of energy produced in injured pt. is not optimum, to supply necessary energy for the repair due to: 1. reduced or absent nutritional intake 2. significant reduction of energy charge and ATP content during shock, hypoxia, sepsis, ischemia and wound - anaerobic metabolism REE (Resting energy expenditure) by Harris and Benedict: (MEN) 66.47 + 13.75 (W) + 5.0 (H) – 6.76 (A) = Kcal/day (Female) 65.51 + 9.56 (W) + 1.85 (H) – 4.68 (A) = Kcal/day Fever: increase resting energy expenditure of approximately 7% for each degree of F of fever. Nutritional Support Fundamental goal of nutritional support: 1. To meet the energy requirement for metabolic processes 2. To maintain a normal core body temperature 3. For tissue repair Nutritional Support Indication of nutritional support: 1. Pre-morbid state 2. Age of the patient 3. Duration of starvation 4. Degree of the insult 5. Likelihood of resuming normal intake within finite period Nutritional Support Determination of Lean Body Mass: 5. Displacement Exchange of labeled ions (radioactive K+) Neutron activation analysis Total body counter Nuclear magnetic resonance 6. Clinical history and physical examination 1. 2. 3. 4. History of weight loss, anorexia and disease process that interfered with intake Anthropometric data (skin fold thickness , arm circumference measurement, thenar eminence) Biochemical determination (TP, albumin, globulin, liver profile, kidney function test) Route of Administration: 1. ENTERAL ROUTE 2. PARENTERAL ROUTE (TPN) 3. COMBINATION ENTERAL ► Advantages: 1. 2. 3. 4. 5. more physiological (liver not bypassed) lesser cardiac work safer and more efficient better tolerated by the patient more economical ENTERAL Route: 1. Naso-enteric tube feeding (blended food – Casseinates and whole protein formulas) Naso-esophageal or NGT / NJT. 2. Gastrostomy tube (blended food) Stamm (sero-lined) – temporary Glassman (mucous-lined) – permanent Percutaneous endoscopic gastrostomy 3. Jejunostomy tube (elemental diet) Roue-en-y - permanent Witzel - permanent Endoscopic ENTERAL Hyperosmolar solution are better tolerated by the stomach: Gastric feeding – increase osmolality first then the volume Small bowel – volume first is increase then osmolality Precautions to be observe to prevent reflux/aspiration: 1. 30 degree angle 2. Conscious 3. Stop feeding at 11 pm Use French 10 and after administration of food clean the tube Prolonged used render the cardia incompetent and sometimes caused stricture Complication of Enteral Feeding 1. Malposition of the catheter (pharynx/trachea): Inadvertently moved Reinsert ideally w/ fluoroscopic guidance 2. Aspiration due to: Overloading Supine position / unconscious Change in gastric motility 3. Solute overloading --> diarrhea, dehydration, electrolyte imbalance (hypokalemia, hypomagnesemia), hyperglycemia (hyperosmolar, nonketotic coma) Avoided by gradual increase in the osmolality of the fluid 4. Perforation (rare) Parenteral Nutrition Components: 1. CHON: Mixture of single amino acid of synthetic origin, largely produced from “intelligent bacteria” cultures 2. CHO: Provides calories; hypertonic dextrose 3. Fat emulsion: 10 or 20% emulsion of soy or safflower oil emulsions, usually emulsified and stabilized with egg phosphatides and lecithin Parenteral Nutrition Indications: Principal indication is found in seriously ill patients suffering from Malnutrition, Sepsis, severe surgical or accidental trauma when the use of the Gastrointestinal tract for feeding is not possible. Can be supplemental in patients with inadequate oral intake Parenteral Nutrition As Primary Therapy: 1. 2. 3. 4. 5. 6. 7. TPN influence the disease process: GIT fistula Renal failure (ATN) Short Bowel Syndrome Acute Burn (severe trauma) Hepatic failure With normal bowel length but with malabsorption syndrome due to SPRUE, enzymatic or pancreatic insufficiency, Ulcerative colitis, regional enteritis Anorexia nervosa Parenteral Nutrition As Supportive Therapy: 1. 2. 3. 4. 5. 6. 7. Nutritional support can be achieved but alteration in the disease process have not been established. New born GIT anomalies (TIF, gastrochisis, omphalocele) Alimentary tract obstruction (achalasia, stricture, carcinoma, pyloric obstruction) Acute radiation enteritis Acute chemotherapy toxicity Prolonged ileus Prolonged respiratory support Large wound losses Parenteral Nutrition Contraindication of TPN: 1. Lack of specific goal for severe metabolic management (inevitable dying). 2. Cardiovascular instability / severe metabolic derangement. 3. Feasible GIT feeding 4. Patient with good nutritional status 5. Infants with less than 3cm of small bowel 6. Irreversible decerebrate (dehumanized) Parenteral Nutrition Route of TPN: Central hyperalimentation Subclavian vein Internal jugular vein Femoral vein Gauge 16, 8-12 inches radio-opaque catheter end at SVC Checked position w/ x-ray Parenteral Nutrition Complication of TPN: I. Technical complication: A. Early: - related to catheter insertion 1. 2. 3. 4. 5. 6. 7. 8. Pneumothorax Arterial laceration Hemothorax Mediastinal hematoma Nerve injury to the brachial plexus Hydrothorax Air embolism Catheter embolism Parenteral Nutrition Complication of TPN: I. Technical complication: A. Late: 1. 2. 3. Erosion of the catheter to the bronchus or right atrium Thrombosis: Upper arm swelling and pain at the base of the neck Streptokinase / heparin ---> coumadin Septic thrombosis: Antibiotic therapy Fogarty catheter embolectomy Excision of the subclavian vein and superior venacava Parenteral Nutrition Complication of TPN: II. Metabolic complication: A. Inadequate administration of certain nutrient 1. Trace metal deficiency: a) Zinc deficiency: perioral pustular rash darkening of the skin creases neuritis b) Copper deficiency: microcytic anemia Parenteral Nutrition Complication of TPN: II. Metabolic complication: A. Inadequate administration of certain nutrient: 2. B. Essential Fatty Acid deficiency: Dry flaky skin w/ small reddish papules and alopecia Disorder of Glucose metabolism: 1. Hypoglycemia – unexpected slowing of the glucose infusion / excessive insulin administration Parenteral Nutrition Complication of TPN: II. Metabolic complication: B. Disorder of Glucose metabolism: 2. Hyperglycemia – most dangerous metabolism complication in TPN Due to rapid infusion (60 ml/hr the increase of 20ml/hr every 24-48 hrs) DM (Hyperosmolar nonketotic coma) due to osmotic diuresis ---> dehydration, fever, obtundation and coma ---> death. Tx: insulin 200 units/day and administration of large dextrose free hypo=osmolar solution (0.45% NSS w/ K+). Parenteral Nutrition Complication of TPN: II. Metabolic complication: C. Liver function derangement: Adnormalities in SGOT / SGPT / Alk. PO4 Fatty infiltrate of liver ----> fat emulsion Parenteral Nutrition Complication of TPN: III. Septic complication: A. Catheter infection: most lethal complication of TPN Bacterial / fungal (candida) Site of entry of the organism ---> site of catheter Symptom: - sudden spike of fever Management: − Change TPN bottle, tubes and filter – culture / investigate for presence of pneumonia, UTI, wound infection, etc. − If fever persist after 8 hrs. ---> removed catheter and culture the tip of the tube. THANK YOU