* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Chapter 21 Antimicrobial Medications
Peptide synthesis wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Clinical neurochemistry wikipedia , lookup
Oligonucleotide synthesis wikipedia , lookup
Vectors in gene therapy wikipedia , lookup
Amino acid synthesis wikipedia , lookup
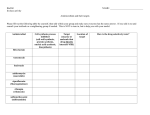
Drug discovery wikipedia , lookup
Chapter 10 Antimicrobial Medications • Chemotherapy • Antibiotic • Synthetic drugs • Semi-synthetic drugs • In 1910, Paul Ehrlich discovered Salvarsan – Arsenic derivative used to treat syphilis • In 1935, Gerhard Domagk discovered a red dye that inhibited G+ bacteria – Prontosil • In 1936, Ernest Fourneau discovered it was the sulfur portion of the dye that was active – stimulated the development of sulfa drugs • In 1928, Alexander Flemming -1st true antibiotic – Penicillium mold secretes compound that inhibits bacterial growth • Selman Waksman isolated streptomycin from the soil bacteria Streptomyces • In 1940s, Howard Florey and Ernst Chain performed first clinical trials of penicillin – Developed a method for mass production – Penicillin G • More than ½ of antibiotics in use come from bacteria – Primarily species of Streptomyces – Some are isolated from species of Bacillus • Some are isolated from various molds – Penicillium and Cephalosporium • Most antibiotic producers are spore formers • Selective Toxicity • Magic bullet – causes damage to the microorganism without causing significant harm to the host – Easier with prokaryotic pathogens – Why? • Chemotherapeutic index – maximum tolerable dose (per kg body weight) / minimum effective dose (per kg body weight) – Higher the index the safer for host • Spectrum of activity – range of different microorganisms against which the drug is effective – Narrow-spectrum • Example – anti-mycobacterials – Broad-spectrum • May disturb normal microbiota • May lead to superinfection • Synergism – increased effect of two drugs when used together – clavulanic acid and amoxicillin • Antagonism – reduction of a drug’s desirable effect when administered with another • penicillin and tetracycline • Adverse effects of antimicrobials – Allergic reactions – Toxic effects – Suppression of normal flora Primary Modes of Action Inhibition of Cell Wall Synthesis – Bacterial cell walls are composed of the polysaccharide peptidoglycan • Some antibiotics prevent the synthesis of intact peptidoglycan • Human cells are unaffected Disruption of Cell Membrane • changes permeability of the plasma membrane – Results in the loss of important metabolites – May target specific membrane components – Ex. particular sterols in fungi cell membranes Inhibition of Protein Synthesis • Common feature of all cells – May target the ribosomes • • • • – Change ribosome shape Block binding sites for tRNA/rRNA Inhibit peptide bond formation Prevent shift of reading frame Use is limited Inhibition of Nucleic Acid Synthesis • Interfere with DNA or RNA synthesis – May act as nucleoside/nucleotide analogs – Some have an extremely limited usefulness – Others are widely used because they are more selectively toxic • May act only on bacterial or viral enzymes Metabolic Antagonists • Inhibition of the synthesis of essential metabolites – enzymatic activity of microbes can be inhibited by a substance that closely resembles the normal substrate for the enzyme – Competitive inhibition Inhibition of Host Recognition or Attachment • Depends on chemical reaction between pathogen and host – Pathogen proteins and specific host receptors – Modification of either attachment or receptor proteins can inhibit attachment and entry Mechanisms for Administration of Drugs • • • • Topical Orally Intramuscularly (IM) Intravenously (IV) Tests to Guide Chemotherapy • Disk-diffusion method (Kirby-Bauer test) • Minimum Inhibitory Concentration tests (MIC) • E-test • Minimum Bactericidal Concentration tests (MBC) Kirby-Bauer Test MIC Test E Test MBC Test