* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Goal BP
Survey
Document related concepts
Transcript
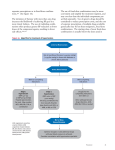
HYPERTENSION Dr Akram Saleh ASS professor Consultant Invasive Cardiologist Jordan University Hospital 22-NOV-2010 HYPERTENSION HTN prevalence ~ age > 18 years 25-30% age > 65 years 50% Only 30-35% of hypertensive patients are well control The BP relationship to risk of CVD is continuous, consistent, and independent of other risk factors. Blood pressure is a continuous variable which fluctuates widely during the day • physical stress • mental stress • High during the day ( early morning) • Low during sleep The definition of hypertension has been arbitrarily set as: abnormal elevation of blood pressure: Control of blood pressure Blood pressure is controlled by an integrated system Prime contributors to blood pressure are: • Cardiac output • Stroke volume • Heart rate • Peripheral vascular resistance Each of these factors can be manipulated by drug therapy BP= C.O.P× Peripheral Resistant Sympathetic Nervous System Sympathetic system activation produces • vasoconstriction • reflex tachycardia • increased cardiac output In this way blood pressure is increased The actions of the sympathetic system are rapid and account for second to second blood pressure control The renin-angiotensin-aldosterone system The RAAS is pivotal in long-term BP control The RAAS is responsible for: • maintenance of sodium balance • control of blood volume • control of blood pressure The RAAS is stimulated by: • fall in BP • fall in circulating volume • sodium depletion Any of the above stimulate renin release from the juxtaglomerular apparatus Renin converts angiotensinogen to angiotensin I Angiotensin I is converted to angiotensin II by angiotensin converting enzyme (ACE) Angiotensin II is a potent • vasoconstrictor • anti-natriuretic peptide • stimulator of aldosterone release from the adrenal glands Aldosterone is also a potent antinatriuretic and antidiuretic peptide Angiotensin II is also a potent hypertrophic agent which stimulates myocyte and smooth muscle hypertrophy in the arterioles Myocyte and smooth muscle hypertrophy: • are both poor prognostic indicators in patients with hypertension • partially explain why hypertension and the risks of hypertension persist in some patients despite treatment Both the sympathetic and RAAS are key targets in the treatment of hypertension Pathophysiology Mechanism Neurogenic: sympathetic activation– high catecholamin– high arteriolar tone– high resistent Abnormal Na balance: Na excretion----Salt and Water retention----increase volume----increase COP---Increase tone At cellular level----Inhibition of Na pump –Increase Na intracellular---Activate Na-Ca pump ---increase intracellular Ca --Vasoconstriction Pathophysiology Multifactorial in origin and caused by a breakdown of the control mechanisms which regulates: Cardiac Out Put Blood volume Na balance Systemic vascular resistant Aetiology of Hypertension Primary – 90-95% of cases – also termed “essential” or “idiopathic” Secondary – about 5% -10% of cases Essential HTN Usually occurs in the fourth or fifth decade Risk factors • Obesity • Excessive salt intake • Excessive alcohol intake • Lack of exercise • Stress • Family history of essential HTN • Others: fetal weight, humoral factors, metabolic syndrome X Caffeine and smoking increase the BP acutely but are not risk factors for the development of chronic essential HTN Secondary – about 5% -10% of cases • Renal : 1- Paranchymal: GN, Pylonephritis, Polycystic kidney,… • 2- Renal artery stenosis: atherosclerosis, fibromuscular dysplasia • Endocrine disease • • • • Phaeochomocytoma Cusings syndrome Conn’s syndrome Acromegaly and hypothyroidism, hyperparathyroidism • Iatrogenic • Hormonal / oral contraceptive • NSAIDs • Steroid, sympathomimetic, carbenoxolone, • Coarctation of the aorta • Sleep apnea syndrome Pregnency: pre-eclampsia, eclampsia SECONDARY HYPERTENSION Drug-induced or related causes • NSAIDs • oral contraceptives, steroids • Cocaine, amphetamines, other illicit drugs • Sympathomimetics • Cyclosporine and tacrolimus • Erythropoietin CLASSIFICATION JNCVII Category • • • Normal PREHTN Hypertension -Stage 1 -Stage 2 Systolic BP Diastolic BP <120 120-139 and or <80 80-90 140-159 >160 or or 90-99 >100 Clinical manifestation Asymptomatic Non-specific symptoms: headache, epistaxis, nocturia,.. Target organ damage: CVS, CNS, Kidney, Eye, Periphral vascular disease Symptoms of secondary causes: Muscle weakness, palpitation, sweating, tremors, flank pain, hematuria,.. Patient Evaluation Evaluation of patients with documented HTN has three objectives: 1. Assess lifestyle and identify other CV risk factors or concomitant disorders that affects prognosis and guides treatment. 2. Reveal identifiable causes of high BP. 3. Assess the presence or absence of target organ damage. Evaluation History Examination Investigation Evaluation- History Duration, Coarse, Treatment Dietary: Salt, Fat, Alcohol Family history Symptoms of secondary causes: muscle weakness, palpitation, anxiety, sweating, tremors, flank pain,.. Symptoms of target organ damage: CVS, CNS,.. Other risk factors: DM, Smoking, Hyperlipidemias,.. Drug history Features of sleep apnea syndrome Examination Detection and Confirmation of hypertension: Patient position Cuff size, inflation, deflation Stethoscope position phase 1 and phase IV SIGNS OF SECONDARY CAUSES SIGNS OF ORGAN DAMAGE BP MEASUREMENT Measurement of BP should be obtained: • In all adults (age >18) at each visit • > 30 minutes after use of nicotine or caffeine • After 5 minutes of rest with arm supported at heart level • With appropriate sized cuff • bladder should encircle 80% of the arm BP MEASUREMENT Measurement of BP should be obtained: • Twice, at least two minutes apart • repeat if >5 mm pressure difference • With patient seated with feet flat on floor, back and arm supported, and arm at heart level • Use manual mercury sphygmomanometer or recently calibrated aneroid manometer or validated automated device (JNCVI and VII) BP MEASUREMENT Self measurement of BP • An avg BP more than 135/85 mmHg measured at home is generally considered to be hypertensive • Wrist and finger manometers are not recommended http://www.familymedshop.com/prod_img/pc0007.jpg General appearance, Azotemia,cushinoid acromegaly Xanthelesma, arcus, fundoscopy Abex beat, A2, S4, syst bruite Carotid pulse, bruit, goiter Upper body hypertrophy Renal bruite, polycystic Kidney, aortic aneurysm Radial pulse, R-F delay xanthoma, A-V fistula Prox muscle weakness Dist sens loss( DM, Alcohol) Pulses: dorsalis ped, post tibia edema Target Organ Damage Heart: Increase 3 folds of cardiac death • Left ventricular hypertrophy • Coronary Atherosclerosis: Angina or prior myocardial infarction •Heart failure Brain: Increase 6 folds of stroke • Stroke or transient ischemic attack •Subarachnoid HG, Intracerebral HG Chronic kidney disease: Nephropathy, Renal failure Peripheral arterial disease: atherosclerosis, aneurysm, dissection Retinopathy Retinopathy Grade 1: Narrowing and tortousity Grade2 : 1+ A/V Nipping Grade 3: 2+ flame shaped HG and soft exudate Grade 4: 3+ papilloedema Laboratory Tests Routine Tests • Electrocardiogram • Urinalysis • Blood glucose, and hematocrit • Serum potassium, creatinin, or the corresponding estimated GFR, and calcium • Lipid profile, after 9- to 12-hour fast, that includes high-density and low-density lipoprotein cholesterol, and triglycerides •Echocardiography •CXR (no more routine) More extensive testing for identifiable causes is not generally indicated unless BP control is not achieved Secondary HTN – who to evaluate Young patients 20<Age > 50 with no family history Createnin >1.2 mg/dl Patients resistant to treatment • Uncontrolled HTN on adequate doses of three medicines one of which is a diuretic Patients who have • Physical findings (abdominal bruits) sensitivity 40%, specificity 90% • Biochemical abnormalities (unprovoked hypokalemia) An acute rise in BP over previously stable baseline Flash pulmonary edema Unexplained raise in createnin after ACE inhibitor Moderate-sever hypertension in patient with diffuse atherosclerosis Treatment Goals of Therapy Reduce morbidity and mortality Treat to BP <140/90 mmHg or BP <130/80 mmHg in patients with diabetes or chronic kidney disease. Benefits of Lowering BP Average Percent Reduction Stroke incidence 35–40% Myocardial infarction 20–25% Heart failure 50% GOALS OF THERAPY JNCVI Goal BP: • HTN: <140/90 • Diabetics: <130/85 • Renal failure: <130/85 • Proteinuria (>1 gm/24 hrs): <125/75 JNCVII • Goal BP: – HTN: <140/90 – Diabetics: <130/80 – Renal failure: <130/80 GOALS OF THERAPY Base medication decisions on: • compelling indications • comorbid conditions • side effect profile • drug interactions • cost Always favor the long-acting formulations Lifestyle Modification Modification Weight reduction Approximate SBP reduction (range) 5–20 mmHg/10 kg weight loss Adopt DASH eating plan 8–14 mmHg Dietary sodium reduction 2–8 mmHg Physical activity 4–9 mmHg Moderation of alcohol consumption 2–4 mmHg Classification and Management of BP for adults BP classification Normal SBP* mmHg DBP* mmHg Lifestyle modification <120 and <80 Encourage Initial drug therapy Without compelling indication Prehypertension 120–139 or 80–89 Yes No antihypertensive drug indicated. Stage 1 Hypertension Yes Thiazide-type diuretics for most. May consider ACEI, ARB, BB, CCB, or combination. Yes Two-drug combination for most† (usually thiazide-type diuretic and ACEI or ARB or BB or CCB). Stage 2 Hypertension 140–159 or 90–99 >160 or >100 *Treatment determined by highest BP category. Initial combined therapy should be used cautiously in those at risk for orthostatic hypotension. Treat patients with chronic kidney disease or diabetes to BP goal of <130/80 mmHg. With compelling indications Drug(s) for compelling indications. ‡ Drug(s) for the compelling indications.‡ Other antihypertensive drugs (diuretics, ACEI, ARB, BB, CCB) as needed. ANTIHYPERTENSIVE MEDICATIONS JNCVII Compelling Indications • Diabetes mellitus (type 1) with proteinuria ACE-I, ARB, CCB • Heart failure Diuretic, -blocker, ACE-I, ARB, and aldo antagonist • High coronary disease risk (stable angina/silent ischemia) Diuretic, -blocker, -blocker, ACE-I, CCB , Diuretic ANTIHYPERTENSIVE MEDICATIONS JNCVII Compelling Indications • Post Myocardial infarction -blockers, ACE-I, aldo antagonist (w/ HF) • Chronic kidney disease ACE-I, ARB • Recurrent stroke prevention Diuretic, ACE-I Logical Combinations Diuretic bDiureti c blocker - ACE inhibitor CCB ablocker b-blocker - * - CCB - * - ACE inhibitor a-blocker * Verapamil + beta-blocker = absolute contra-indication Thank you Renal Angiogram Angioplasty Right Stent in-situ Coronary Stents Bilateral Stents In-Situ