* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Противомикробни средства
Orphan drug wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Discovery and development of non-nucleoside reverse-transcriptase inhibitors wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Drug design wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Neuropharmacology wikipedia , lookup
Discovery and development of cephalosporins wikipedia , lookup
Pharmacognosy wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Psychopharmacology wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
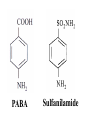
Medical University of Sofia, Faculty of Medicine Department of Pharmacology and Toxicology • SULFONAMIDES • ANTIMYCOBACTERIAL DRUGS • PRINCIPLES OF ANTIBACTERIAL CHEMOTHERAPY Assoc. Prof. Iv. Lambev E-mail: [email protected] SULFONAMIDES G. Domagk (1895-1964), bacteriologist and pathologist discovered the first sulphonamide in 1935. Nobel prize for Physiology and Medicine in 1939. Mechanism of action •Unlike man, the most bacteria cannot utilize external folic acid, a nutrient which is essential for growth, and have to synthesize it from para-aminobenzoic acid (PABA). Sulfonamides are structurally similar to PABA and inhibit the enzyme dihydrofolate synthetase in the biosynthetic pathway for folic acid. •High concentration of PABA antagonize the effectiveness of sulfonamides. PABA Sulfanilamide DHF synthetase PABA DHF reductase DHFA (-) Sulfonamides THFA Purines (-) Trimethoprim Dietary folate in man DNA Proteins Spectrum of activity •Sulfonamides have a bacteriostatic action on wide range of Gram-positive and Gramnegative microorganisms and also active against toxoplasma, nocardia species and chlamydia. •Sulfonamides alone are usually reserved for treatment of nocardiosis and toxоplasmosis. Resistance •Resistance is common and due to the production of dihydrofolate synthetase with reduced affinity for binding of sulfonamides, and is transmitted in Gram-negative bacteria by plasmids. •Resistant strains of Staphylococcus aureus can synthesize more PABA than normal. Pharmacokinetics •The most sulfonamides are well absorbed orally although parenteral preparations of some are available. They are widely distributed in the body and cross the BBB and placenta. •Sulfonamides are metabolized in the liver, initially by acetylation which shows genetic polymorphism. The acetylated product has no antimicrobial actions but retains toxic potential. Substantial amounts of parent drugs and N-acetyl metabolite are excreted by the kidney. Unwanted effects •Hypersensitivity reactions include rashes, vasculitis, Stevens-Johnson syndrome. •Haemolysis in patients with glucose-6phoshate-dehydrogenase deficiency. •Crystalluria is a potential problem with overdose of these drugs or with acid urine. •Sulfonamides compete for bilirubin binding sites on albumin and can cause kernicicterus in neonates. Stevens–Johnson syndrome after oral intake of Co-trimoxazole (Color Atlas and Synopsis of Clinical Dermatology, 1999) Lyell syndrome after oral intake of Co-trimoxazole Clcr Contraindications •Sulfonamides should not be used in the last trimester of pregnancy; in neonates; during the period of lactation; in patients with hypersensitivity reactions. DRUG PREPARATIONS t1/2 8–16 h: - sulfamethoxazolе - sulfametrolе t1/2 > 16 h: - sulfadimethoxinе - sulfalen Sulfacetamidе •collyrium 20% 10 ml Sulfadicramide For local treatment of bacterial conjunctivitis Low GI resorption (30%) - Sulfaguanidinе in GI infections Sulfasalazinе ® (Salazopyrin ) • colitis ulcerosa Sulfamethaxzole/Trimethopim Trimethoprim inhibits dihydrofolate reductase which converts dihydrofolate to tetrahydrofolate: DHF reductase DHF synthetase PABA DHFA (-) Sulfamethoxazole THFA (-) Trimethoprim Purines The bacterial enzyme is inhibited at 50 000 times lower concentrations than the mammalian equivalent. The combination of trimethoprim with the sulfonamide sulfamethoxazole (known as co-trimoxazole – BAN) acts synergistically to prevent folate synthesis by bacteria. However, resistance to the sulfamethoxazole component, and the incidence of unwanted effects limit the value of this combination. Thrimethoprim has a wide spectrum of activity against Gram-positive and Gramnegative bacteria. The combination with sulfamethoxazole is also effective against Proteus and Pneumocystis carinii (this is now its major indication). Trimethoprim and sufamethoxazole are well absorbed from the gut. Their t1/2 is about 11 h. Trimethoprim is excreted unchanged by the kidney. Co-trimoxazole is availble for p.o. and i.v. use. Co-trimoxazolе (BAN) - tab. 480 mg ® •Trimezol - tab. 480 mg ® •Biseptol Adverse effects Sulfamethoxazole/Trimethopim •Nausea, vomiting and diarrhoea, which are usually mild. •Skin rashes. •Folate deficiency leading to megaloblastic changes in the bone marrow is rare except in patients with depleted folate stores. •Marrow depression with agranulocytoses. ANTIMYCOBACTERIAL DRUGS Antitubercolous drugs •Synthetic drugs (p.o.): Isoniazid, Ethambutol, Pyrazinamide, Ethionamide •Antibiotics: Rifampicin (p.o.), Rifamycin (i.v. infusion), Rifabutin; Streptomycin Drugs for treatment of leprosy p.o.: Rifampicin, Clofazimine, Dapsone ANTITUBERCOLOUS DRUGS Isoniazid (5 mg/kg/24 h p.o. ) inhibits production of long-chain mycolic acids which are unique to the cell wall of mycobacteria species. It is bacteriocidal against dividing microorganisms. Resistance is due to random mutation. It can be troublesome in developing countries. Oral absorption of isoniazid is good, but reduced by food. It diffuses well into the body tissues, including the CSF, and penetrates into macrophages so that it is effective against intracellular tubercle bacilli. Isoniazid undergoes genetically controlled polymorphic acetylation in the liver. A high percentage of fast acetylators being found in Japanese and Eskimo populations. In European populations 40–50% are rapid acetylators. Unwanted effects of isoniazid •Nausea and vomiting. •Peripheral neuropathy in high doses. This can be prevented by prophylactic oral use of pyridoxine (vitamin B6). High risk patients are with diabetes, alcoholism, chronic renal failure, malnutrition. •Hepatotoxicity. •Systemic lupus erythematosus like syndrome. (B6) Ethambutol impairs synthesis of the cell wall of mycobacteria. It is primarily bacteriostatic. Its oral bioavailability is 77%. Only a small amount is metabolized and most is eliminated unchanged by the kidney. Unwanted effects •Headache, dizziness •Optic neuritis (dose-related, but usually reversible). Pyrzinamide has bactericidal effect. Adverse effects •Hyperuricemia (it may precipitate gout) •Hepatotoxicity •Rashes and photosensitivity •Sideroblastic anaemia Rifampicin (Rifampin) acts by inhibition of DNA-dependent RNA polymerase and has bactericidal effect. It has a broad spectrum of activity which in addition to mycobacteria species includes brucella, legionella and staphylococci. •Resistance develops rapidly. It is a one step process of mutation. Absorption from gut is almost complete, but is delayed by food. Peak plasma levels reach 3 h after a single oral dose of 600 mg. The t1/2 is 3 h. About 85-90% of the drug is protein bound in plasma but rifampicin penetrates well into most tissues, cavities and exudates. It is metabolized by deacetylation and is excreted mainly in the bile. The drug and its metabolite undergo prolonged enterohepatic circulation. Unwanted effects of rifampicin •Sometimes influenza-like symtoms, flushing and rashes. •Hepatotoxicity, usually only producing a transient rise in plasma of transaminases. •Induction of drug-metabolizing enzymes in the liver. Important interactions include those with oral contraceptives, phenytoin, warfarin and sulphonylureas. •Urine and tears become pink/red which may be a useful guide to compliance. Streptomycin is an aminoglycoside antibiotic. Its antibacterial activity is due to it binding to the 30S subunit of the bacterial ribosome and inhibiting of protein synthesis. It has a wide spectrum of antibacterial activity but is primarily use to treat mycobacterial infections (i.m.). •The main problems are eighth nerve toxicity (vestibulotoxicity more than deafness), nephrotoxicity, allergic reactions. DRUG TREATMENT OF TUBERCULOSIS •Mycobacterium tuberculosis readily develops resistance to monotherapy. Three or four drugs are used for the first 2 months, and than the treatment is continued with 2 drugs for a further 6-9 months. A standard regimen in the UK includes rifampicin and isoniazid for 6 months with ethambutol and pyrazinamide for the first 2 months only. PRINCIPLES OF ANTIBACTERIAL CHEMOTHERAPY (Adapted from Laurence et al., 1997) The following principles, many of which apply to drug therapy in general, are a guide to good clinical practice with antimicrobial agents. •Make a diagnosis as precisely as possible: - defining the site of action; - defining the microorganism(s) responsible and their sensitivity to drugs; - biological samples for laboratory must be taken before treatment is begun. •Remove barriers to cure (e.g. lack of free drainage of abscesses, obstruction in the urinary or respiratory tracts). •Decide whether chemotherapy is necessary. As a general rule, acute infections require chemotherapy whilst chronic infections may not. Chronic abscess or empyema respond poorly. Even some acute infections such as gastroenteritis are better managed symptomatically than by antimicrobials. •Select the best drugs. This involves consideration of: - specificity (the antimicrobial activity of drug must cover the infecting organisms; - pharmacokinetic factors (the chosen drug must be reach the site of infection (e.g. by crossing BBB); - the patients (who may previously have allergic reactions to antimicrobials or whose routes of drug elimination my be impaired e.g. by renal disease). In some infections the choice of antimicrobails follows automatically from the cliniccal diagnosis because the causative organknish is always the same, and is virtually always sensitive to the same drug, e.g. segmental pneumonia in a young person which is almost always caused by S. pneumonia (benzylpenicillin), some haemolytic streptococcal infections, e.g. scarlet fever and erysipelas (benzylpenicillin), typhus (tetracycline), leprosy, lues. In the other cases the infecting organism is identified by the clinical diagnosis, but no assumption can be made as to its sensitivity to any one antimicrobial, e.g. tuberculosis. In the most cases the infecting organism is not identified by the clinical diagnosis, e.g. in urinary tract infections, meningitis etc. In the last two categories the choice of antimicrobial drug may be guided by: - knowledge of the like pathogens - simple staining and sensitivity tests. •Indications for combination therapy: -To avoid the development of resistance in chronic infections (tuberculosis). - To broaden the antibacterial spectrum: a) in a known mixed infection; b) if the microorganism cannot be predicted (septicemia complicating neutropenia). - To obtain potentation (e.g. penicillin plus genatmicin for enterococcal endocarditis) •Antimicrobial therapy and pregnancy PRC B have: •Azithromycine •Erythromycine •Penicillins •The most of cefalosporines •Administer the drug in optimum dose and frequency and by the most appropriate route. - Inadequate dose may encourage the development of microbial resistance. - Intermittent dosing is proffered to continual infusion. - Plasma concentration monitoring can be applied to optimize therapy with aminosides, fluoroquinolones, cephalosporins etc. in patients with kidney disease. •Continued therapy enough until apparent cure has been achieved. - Most acute infections are treated for 5 to 10 days. There are many exceptions to this, such as typhoid fever, tubercularsis and infective endocarditic, in which relapse is possible long after apparent clinical cure and so the drugs are continued for a long time, determined by experience. •Test for cure. In some infections, microbiological proof of cure is desirable because disappearance of symptoms and signs occurs before the microorganisms are eradicated, e.g. urinary tract infections (examinations must be done after withdrawal of chemotherapy). •Prophylactic chemotherapy for surgical and dental procedures should be of very limited duration. It should be start at the time of surgery to reduce the risk of producing resistant microorganisms.