* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download MDR-TB
Survey
Document related concepts
Transcript
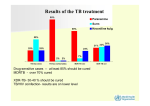
Epidemiology G.B. Migliori, Stefan Niemann WHO Collaborating Centre for Control of TB and Lung Diseases, Fondazione S. Maugeri, IRCCS, Tradate, Italy Research Center Borstel, Borsel, Germany Outline: • • • • Epidemiology of TB Epidemiology of MDR-TB Outcomes of MDR-TB Fingerprinting for TB and MDR-TB •Prevalence of infectious cases •Duration of illness •Intensity, frequency and duration of contact Largely exogenous •Particles/volume x exposure time •Production of infectious droplets •Clearance of air •Extent of exposure Largely endogenous Innate resistance Performance of cell-mediated immunity Re-infection Strain virulence RF RF RF RF Exposure Subclinical Infection TB epidemiological model Form and site of TB Age Patient’s susceptibility Delay in diagnosis Infectious TB/MDR-TB Death Non-infectious TB/MDR-TB •Prevalence of infectious cases •Duration of illness •Intensity, frequency and duration of contact Largely endogenous Largely exogenous •Particles/volume x exposure time •Production of infectious droplets •Clearance of air •Extent of exposure Innate resistance Performance of cell-mediated immunity Re-infection Strain virulence RF RF RF RF Exposure ? Subclinical Infection ? Form and site of TB Age Patient’s susceptibility Delay in diagnosis Infectious TB/MDR-TB Death Non-infectious TB/MDR-TB ? ? % PPD (+) reactors in 0-14 y.o. contacts Rotterdam (1967-1969): SS+ cases are infectious 50 45 40 35 30 25 SS+ C+ C- 20 15 10 5 0 Household contacts other contacts % of PPD+ children 0-14 yrs RR of TB by Risk Group compared to Gen. Popul. Risk Group Relative Risk AIDS HIV (+), PPD (+) HIV (+), PPD (-), ANERGIC HIV (+), PPD (-), NOT ANERGIC 170 40-50 30 3-25 SILICOSIS FIBROTIC LESION IMMUNOSUPPRESSIVE TREATMENT HEMODIALYSIS JEJUNOILEAL BYPASS CA OF HEAD OR NECK PPD CONVERSION <1 YEAR PPD CONVERSION > 7 YEARS 30 4-26 12 10-15 27-63 16 10 2 Risk of TB infection in European countries Age-specific prevalence of TB Infection, Switzerland 1920-1990 TB reported in Switzerland by age, 1990 TB reported incidence in African Countries, 1990-2002 1000 RATE PER 100 000 BOTSWANA MALAWI MOZAMBIQUE SOUTH AFRICA UGANDA TANZANIA ZIMBABWE 100 1990 91 92 93 94 95 96 97 98 99 2000 1 2 TB Case notifications, SS+ and all forms of TB, Kenya, 1990-2002 300 263 PTB+ 250 242 All types TB 218 202 n/100,000 pop. 200 171 144 150 130 108 100 50 89 84 32 62 54 53 31 33 42 95 44 98 104 110 83 53 63 68 0 '90 '91 '92 '93 '94 '95 '96 Year '97 '98 '99 '00 '01 '02 Latest global TB estimates Estimated number of cases All forms of TB Greatest number of cases in Asia; greatest rates per capita in Africa Estimated number of deaths 9.27 million 1.77 million (139 per 100,000) (27 per 100,000) Multidrug-resistant TB (MDR-TB) 511,000 ~150,000 Extensively drug-resistant TB (XDR-TB) ~50,000 ~30,000 HIV-associated TB 1.4 million (15%) 456,000 (2009) Estimated number of new TB cases, 2007 9.2 million new cases (~434,000 in Europe) 1.7 million death (~63,000 in Europe) Notified TB Incidence Rate 2007 Estimated TB Incidence Rate 2007 1.5-3 times higher than cases notified… Estimated TB burden, 2007 TB incidence rates stable or falling slowly 450 400 350 300 AFR AMR EMR EUR SEAR WPR 10 9 8 7 6 5 4 3 2 1 0 World 250 200 1990 9.27 Cases in million 1995 2000 150 100 50 0 1990 1995 2000 2005 2005 WHO European Region (EUR) 53 countries 18 high priority countries for TB 25 EU countries 1. 2. 3. 4. 5. 6. 7. 8. 9. Armenia Azerbaijan Belarus Bulgaria Estonia Georgia Kazakhstan Kyrgyzstan Latvia 10. 11. 12. 13. 14. 15. 16. 17. 18. Lithuania Moldova Romania Russian Fed. Tajikistan Turkey Turkmenistan Ukraine Uzbekistan 19 TB case notification rate in EUR Annual TB cases per 100,000 pop. 90 80 295,240 70 East+ EUR (18 countries) 60 50 354,954 40 All EUR (53 countries) 30 373,497 20 54,231 10 European Union (25 countries) Year 0 80 81 82 83 84 85 86 87 88 89 90 91 92 93 94 95 96 97 98 99 00 01 02 03 04 Incidence of TB among TB-infected persons HIV (+) vs HIV (-) TB Infection HIV (-) 5% first 2 years <10% lifetime World Health Organization Incidence of TB among TB-infected persons HIV (+) vs HIV (-) TB Infection HIV (-) HIV (+) 3-13% every year >30% lifetime 5% first 2 years <10% lifetime World Health Organization Nairobi 600 0.15 500 400 6 yr 0.10 300 200 0.05 100 0 Williams B. 3rd Global TB/HIV Working Group Meeting; Montreux, 1980 4-6 June 2003 0.00 1990 2000 HIV prevalence TB notification/100k 700 (per 100K adults, 1999) Estimated annual TB incidence Estimated TB incidence vs. HIV prevalence in high burden countries 1600 1200 800 400 HIV prevalence increases by 1% TB incidence increases by 26/100k/yr 0 0.0 Williams B. 3rd Global TB/HIV Working Group Meeting; Montreux, 4-6 June 2003 0.1 0.2 0.3 HIV prevalence, adults 15-49 years 0.4 Pattern of the anti-TB resistance 100% 80% 60% 40% 20% 0% Estonia Patients resistant to HR only Latvia Orel Patients resistant to HRES Peru Philippines Tomsk Patients resistant to HRES and second-line drugs XDR-TB – extensively and 'extreme' drug resistant TB XDR = MDR-TB plus resistance to any fluoroquinolone, and to at least 1 of 3 injectable second-line anti-TB drugs (capreomycin, kanamicin, amikacin) Of 17,690 isolates during 2000-2004 20% were MDR and 2% were XDR XDR found in: USA: 4% of MDR Latvia: 19% of MDR S Korea: 15% of MDR XDR= HR + 1 FQ + 1 Injectable (KM or AMK or CM) 1st-line agents •INH Injectable agents •RIF •SM Fluoroquinolones •KM •Cipro 2nd-line Oral agents •AMK •Oflox •ETA/PTA •CM •Levo •PASA •Moxi •CYS •PZA •EMB •Gati "3rd-line" agents Not routinely recommended, efficacy unknown, e.g., amoxacillin/clavulanic acid, clarithromycin, clofazamine, Estimated MDR-TB incidence More than 50 000 cases From 10 000 to 50 000 cases From 1 000 to 9 999 cases From 100 to 999 cases Less than 100 cases Top 19 settings with MDR among new cases > 6% (1994-2007) Baku City, Azerbaijan Republic of Moldova Donetsk, Ukraine Tom sk Oblast, Russian Federation Tashkent, Uzbekistan Kazakhstan* Estonia Mary El Oblast, Russian Federation Ivanovo Oblast, Russian Federation* Latvia Liaoning Province, China Lithuania Arm enia Orel Oblast, Russian Federation Henan Province, China Inner Mongolia Autonom ous Region, China Indicates survey data reported in an earlier phase of the project Heilongjiang Province, China Georgia Dom inican Republic* 0.0 5.0 10.0 15.0 20.0 25.0 Countries with XDR-TB confirmed cases as of Dec 2008 Study 2: Italy, Germany, Estonia, Russia (Archangels Obl) 4,346 C+ 361 MDR 64 XDR Italy: MDR 4.2%; XDR 0.4% Germany: MDR 6.1%; XDR 0.4% Estonia: MDR 27.4%; XDR 5.9% Russia: MDR 7.3%; XDR 0% 3 Groups compared: • XDR: 64 (48 with definite outcome) • MDR “complicated” (res. to all 1st line drugs): 267 (187 with outcome) • “Other” MDR (suscept. to at least 1 first-line drug): 94 (53 with outcome) XDR: a death sentence? N° of previous TX periods > 30 days Hospital Admission (days) Smear conversion (days) Culture conversion (days) SRHEZ; FQ,AK,Cyc 220 Not achieved Not achieved Regular TX°, improved 73 SRHEZ; FQ,Eth,Ak,PAS,Cyc SRHEZ; FQ,AK,Cyc 83 Not achieved Not achieved Died 16 3 SRHEZ; FQ,Eth,AK,PAS,K, Cyc,Clof SRHZ; FQ,Eth,K 406 300 300 Regular TX°, improved 10 Bilateral cavities 4 SRHEZ; FQ,PAS,Cyc SRHZ; FQ,Eth,AK,PAS 69 49 35 Regular TX°, improved 6 Italy Bilateral cavities 3 SRHEZ; FQ,Eth,AK,PAS,C, K,Cyc,Rb,Clof,Dap, Cl,Th SRHEZ; FQ,Eth,AK,PAS,C, K,Cyc,Rb,Clof 422 Not achieved Not achieved Died 94 38/F Italy Bilateral cavities 3 SRHEZ; FQ,Eth,PAS,C,Cyc SRHEZ; FQ,AK,PAS,Cyc 80 Not achieved Not achieved Died 12 7) It 49/F Italy Bilateral cavities 3 SRHEZ; FQ,Eth,AK,PAS,C, K,Cyc,Rb,Clof, Dap,Cl,Th SRHEZ; FQ,Eth,AK,PAS,C, K,Cyc,Rb,Clof, Dap,Cl,Th 625 Not achieved Not achieved Died 60 8) G 33/M Uzbekistan Monolateral cavity 2 SRHEZ; SRHEZ; FQ,Eth,AK,C,Rb 120 Not achieved Not achieved Regular TX°, improved 4 9) G 29/M Uzbekistan Bilateral cavities 2 SRHEZ; Rb SRHEZ; FQ,C 240 180 160 Regular TX°, improved 12 10)G 52/M Azerbaijan Monolateral cavity Not available SRHEZ; FQ,AK,PAS,C,Cyc, Rb 140 7 35 Regular TX°, improved 6 11) It 36/F Romania Bilateral cavities SRHEZ; FQ,Eth,PAS,Cyc,Rb RHZ; FQ,AK,Rb 248 110 Not achieved Regular TX° 28 Country of birth Radiology at XDR diagnosis Drug received during previous TX periods Country Age/sex 1) It 40/M Italy Bilateral cavities 3 SRHEZ; Rb 2) It 61/F Peru Monolateral cavity 1 3) It 27/F Moldova Monolateral cavity 4) It 46/M Senegal 5) It 43/F 6) It >1 4 Drug resistance at XDR diagnosis Outcome TX duration (months) MDR-TB, susceptible at least one 1st drug MDR-TB, resistant to all 1st line drugs XDR-TB Eur Respir J 2007 Prisons… Migration Poverty, malnutrition…. Congregate settings: homeless shelter The goals of TB control: To reduce mortality, morbidity and transmission of the disease, while prevention drug resistance, until it no longer poses a threat to public health An Expanded DOTS Framework for Effective TB control. WHO/CDS/TB/2002.297 World Health Organization Regional Office for Europe TB control & elimination strategies Control: to reduce the incidence of new TB infection through rapid identification and effective treatment of infectious cases (sources of infection) Elimination: additional strategy aimed at reducing the prevalence of latent TB infection by provision of preventive therapy to persons at increased risk of progression from latent infection to TB disease World Health Organization Regional Office for Europe Principles of TB control: 1. Contagious persons must be detected and their TB diagnosed, treated, and rendered noncontagious 2. Non-contagious persons must be prevented from becoming contagious 3. Persons not infected must be prevented from becoming infected World Health Organization Regional Office for Europe R TB elimination Less than 1 smear positive case per 1 million population emerges annually and /or the prevalence of TB infection is below 1% and continues to decrease (K. Styblo, 1990) World Health Organization Regional Office for Europe Full implementation of Global Plan: 2015 MDG target reached but TB not eliminated by 2050 Propects for TB elimination by 2050 Incidence/100,000/yr 10000 1000 Projected incidence 100x bigger than elimination target in 2050 100 10 Elimination 16%/yr Elimination target: 1 / million / year by 2050 Global Plan 6%/yr Current trajectory 1%/yr 1 2000 2010 2020 2030 Year 2040 2050 Interventions over time: old weapons might be useful again to manage XDR First sanatorium Germany, 1857 First Dispensary, Scotland, 1897 BCG vaccination Pneumotorax, Italy, 1907 Drugs, 1945-1962 Koch, Mtb, 1882 MMR,1950-1980 Fox:Ambulatory treatment, 1968 Styblo model, 1978 DOTS, 1991 Outbreak Management, sanatoria Risk Group Management screening drug therapy Socio-economic improvement Carlo Forlanini, first notes on Pneumotorax January 7th, 1907 The STOP TB Strategy – 2009 1. Pursue high-quality DOTS expansion and enhancement 2. Address TB-HIV, MDR-TB, and the needs of poor and vulnerable populations 3. Contribute to health system strengthening based on primary health care a. b. c. d. e. a. b. c. a. b. c. d. 4. Help improve health policies, human resource development, financing, supplies, service delivery and information Strengthen infection control in health services, other congregate settings and households Upgrade laboratory networks, and implement the Practical Approach to Lung Health (PAL) Adapt successful approaches from other fields and sectors, and foster action on the social determinants of health Involve all public, voluntary, corporate and private providers through Public-Private Mix (PPM) approaches Promote use of the International Standards for TB Care (ISTC) Empower people with TB, and communities through partnership a. b. c. 6. Scale-up collaborative TB/HIV activities Scale-up prevention and management of multidrug-resistant TB (MDR-TB) Address the needs of TB contacts, and of poor and vulnerable populations, including women, children, prisoners, refugees, migrants and ethnic minorities Engage all care providers a. b. 5. Secure political commitment, with adequate and sustained financing Ensure early case detection, and diagnosis through quality-assured bacteriology Provide standardized treatment with supervision, and patient support Ensure effective drug supply and management Monitor and evaluate performance and impact Pursue advocacy, communication and social mobilization Foster community participation in TB care Promote use of the Patients' Charter for TB Care Enable and promote research a. b. Conduct programme-based operational research, and introduce new tools into practice Advocate for and participate in research to develop new diagnostics, drugs and vaccines 2006/rev. 2009 “Nobody wants me around..” TB Control Extensively drug resistant (XDR) - TB MDR = Multi Drug Resistance Resistance against at least INH and RMP XDR = Extensively Drug Resistance Resistance against at least INH and RMP (MDR-TB) + Fluoroquinolone (e.g. ofloxcin) + injectible drugs (e.g. capreomycin, amikacin) Epidemiology Complex Interactions: Treatment failure, Transmission Relative Fitness of MDR strains,... Efficient methods for strain typing MDR TB in Germany Beijing Genotype MDR TB in Germany Hospital transmission of MDR tuberculosis patient A A B IS6110 fingerprint pattern resistanc e susceptible MDR MDR Patient A was reinfected with the MDR strain of patient B during their stay at hospital Niemann et al., JCM 1997 MDR TB in Germany o Transmission of drug-resistant strains could be shown and seem to contribute to the problem of drug-resistant TB Germany o In most cases, drug-resistant M. tuberculosis strains seem to be as infectious as drug-susceptible strains o Regular tuberculosis therapy is not sufficient to protect patients against infection with a multidrug-resistant M. tuberculosis strain o Drug-resistant M. tuberculosis strains are presumably carried over from the former SU to Germany o M. tuberculosis strains of the "Beijing Family" could be found in Germany too, representing a rising proportion of all drug-resistant TB cases in Germany TSRU Meeting 1998, ESM Meeting 1998 MDR TB in Germany 1995-2005: 806 strains 1995 Beijing genotype 12 % 2005 Beijing genotype 68 % Origin of Patients with Beijing strains >70% of the patients with Beijing strains had an indication of foreign birth These patients were mainly coming from the former SU (Kazakhstan, Georgia, Ukraine, etc.) Resistant TB in Abkhazia • “Chronic Conflict” – War 1991-94 – Independent since 1994 – Blockade since 1994 • 150,000 citizens • Prospective study 2003 – 2006 326 patients Pardini et al. Tuberculosis 2009 Resistant TB in Abkhazia Total tested Fully sensitive Any resistance - Any H resistance - Any R resistance - Any E resistance - Any S resistance H and R resistance - MDR - H+R only - H+R+S only - H+R+E+S only Number of resistant drugs - 1 drug - 2 drugs - 3 drugs - 4 drugs New cases No. % 196 90 45.9 106 54.1 59 30.1 17 8.7 36 18.4 75 38.3 Previously treated cases No. % 127 40 31.5 87 68.5 74 58.3 51 40.2 50 39.4 67 52.8 Total No. % 326* 131 40.6 195 60.4 135 41.8 69 21.4 88 27.2 144 44.6 17 1 5 11 8.7 0.5 2.6 5.6 49 2 12 35 38.6 1.6 9.5 27.6 68 3 17 48 21.0 0.9 5.3 14.9 55 32 8 11 28.1 16.3 4.1 5.6 21 12 19 35 16.5 9.5 15.0 27.6 76 44 27 48 23.3 13.5 8.3 14.7 Resistant TB in Abkhazia Second line resistance among MDR strains No resistance to 2nd line drugs Any resistance to 2nd line drugs - Ethionamide - Kanamycin - Capreomycine - Ofloxacin > three 2nd line drugs XDR strains** New cases N=17* No. % 11 64.7 6 35.3 5 7.1 3 4.3 0 0 0 0 0 0 0 0 Previously treated cases N=49* No. % 16 32.6 33 67.3 20 60.6 18 54.5 3 9.1 3 9.1 2 6.1 3 9.1 Total N=68 No. 29 39 25 21 3 3 2 3 % 42.6 57.3 36.8 30.9 4.4 4.4 2.9 4.4 Resistant TB in Abkhazia Beijing genotype and MDR-TB: OR 20.9 (95% CI 10.5-41.7 ), p<0.001 Resistant TB in Abkhazia MDR - strains Cluster 5 variants 23 % of all MDR cases Caused by one clone (Cluster 5) Highly resistant – Super virulent phenotype Resistant TB in the Aral Sea region TB – incidence of more than 100/100.000 High resistance rate supposed 416 patients recruited between July 2001 and March 2002 76% of eligible patients in Dashoguz and 68% in Karakalpakstan 2005 Resistant TB in the Aral Sea region Karakalpakstan 50% Dashoguz 40% MDR-TB 40% 27% 30% 20% 10% 19% 13% 11% 4% 0% New Re-treatment Total Cox et al., EID, 2004 Resistant TB in the Aral Sea region 40% of all isolates in clusters 50% of all isolates belong to the Beijing genotype 55% of Beijing genotype isolates in clusters Cox et al. & Niemann, Resp Res, 2005 Resistant TB in the Aral Sea region New (n=198) Previously treated (n=184) 80 73 76 % of Beijing type strains 70 58 60 50 40 46 39 59 55 46 45 38 30 20 10 0 fully susceptible resistant to 1 drug poly resistance (not MDR-TB) MDR-TB Total Cox et al. & Niemann, Resp Res, 2005 Treatment failure Patient 1 Isolat e1 Resistance H, R 2 H, R, E, Z, P Patient 2 Isolat e1 Resistance susc. 2 H, S 3 H, R, E, S Cox H, et al. CID, 2007 Treatment failure 382 patients analyzed with DNA fingerprint 72 patients with follow up culture 10 had a different strain 62 had the same strain Cox H, et al. CID, 2007 Treatment failure 11 (39%) of 28 polyresistant Beijing genotype strains amplified resistance compared with none of the 27 non-Beijing polyresistant strains Cox H, et al. CID, 2007 Resistant TB in the Aral Sea region Cox et al. & Niemann NEJM 2008 Resistant TB in the Aral Sea region Cox et al. & Niemann NEJM 2008 Summary TB is back MDR- and XDR-TB are a new challenge Major driving force for the spread of MDR is transmission Exogenous reinfection even with XDR-TB Beijing genotype strongly associated with drug resistance/transmission Clonal expansion of particular MDR strains with super transmissible phenotype Molecular mechanisms mainly unclear