* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 01. Hepatitis(ABC)1432 - King Saud University Medical Student
Ebola virus disease wikipedia , lookup
Toxoplasmosis wikipedia , lookup
Onchocerciasis wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Herpes simplex wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Microbicides for sexually transmitted diseases wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Sarcocystis wikipedia , lookup
Chagas disease wikipedia , lookup
Trichinosis wikipedia , lookup
Antiviral drug wikipedia , lookup
Leptospirosis wikipedia , lookup
Henipavirus wikipedia , lookup
West Nile fever wikipedia , lookup
Marburg virus disease wikipedia , lookup
Schistosomiasis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Neonatal infection wikipedia , lookup
Lymphocytic choriomeningitis wikipedia , lookup
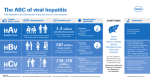
14/2/2011 Dr. Salwa Tayel 1 Viral Hepatitis Associate Professor Family and Community Medicine Department King Saud University 14/2/2011 21/2/2010 Dr. Salwa Tayel 2 Viral Hepatitis – Historical Perspective “Infectious” Viral hepatitis “Serum” A Enterically E transmitted “NANB” C Parenterally transmitted B D other 14/2/2011 Dr. Salwa Tayel 3 A, B, Cs of Viral Hepatitis • • • A – fecal-oral spread: hygiene, drug use, men having sex with men, travelers, day care, food – vaccine-preventable B – sexually transmitted – 100x more infectious than HIV – blood-borne (sex, injection drug use, motherchild, and health care) – vaccine-preventable C – blood borne (injection drug use primarily) – 4-5 times more common than HIV – NOT vaccine-preventable! 14/2/2011 Dr. Salwa Tayel 4 Acute Hepatitis – Clinical Symptoms Asymptomatic > Symptomatic > Fulminant Liver Failure > Death Symptoms (if present) are the same, regardless of cause (e.g., A, B, C, other viruses, toxins) • Nausea, vomiting • Abdominal pain • Loss of appetite • Fever • Diarrhea • Light (clay) colored stools • Dark urine • Jaundice (yellowing of eyes, skin) 14/2/2011 Dr. Salwa Tayel 5 Infectious hepatitis, epidemic hepatitis, epidemic jaundice. • Children are usually asymptomatic, adults symptomatic • Onset is usually sudden with fever followed within few days by jaundice. • Complete recovery is the rule (no chronicity). • The case-fatality rate among persons of all ages is approximately 0.3% • but is approximately 2% among persons > 40 years. Dr. Salwa Tayel 6 It is worldwide In developing countries, it occurs in endemic and epidemic forms due to: • Poor environmental sanitation • Overcrowding • Lack of personal hygiene. Dr. Salwa Tayel 7 Geographic Distribution of HAV Infection Dr. Salwa Tayel 8 Cycle of infection Agent Susceptible Host IP Reservoir PC Portal of Inlet Portal of Exit Mode of transmission Dr. Salwa Tayel 10 Hepatitis A Virus Picornavirus (RNA) Stable at low pH Inactivated by high temperature, formalin, chlorine Dr. Salwa Tayel 11 • Human clinical sub-clinical cases incubating carriers Through anal orifice with faeces. Dr. Salwa Tayel 12 1. Fecal-oral route. Close personal contact; house hold contact,, sex contact, day care centers. 2.Common vehicle; contaminated water and food; raw shellfish food handlers . 3. Rarely through blood transfusion and contaminated syringes. Dr. Salwa Tayel 13 Through the mouth. • Susceptibility is general. • Post infection immunity probably lasts for life. Dr. Salwa Tayel after the attack 14 • Incubation period 28 days (range 15-50 days) • The maximum infectivity is during the latter half of the incubation period (2 weeks before and 1 week after onset of jaundice). Dr. Salwa Tayel 15 Prevention of Hepatitis A Vaccination Immune globulin Good hygiene (hand washing) Clean water systems; avoidance of food contamination Food sanitation especially shell fish and raw eaten food. Dr. Salwa Tayel 16 Hepatitis A Prevention – Immune Globulin Pre-exposure – travelers to intermediate and high HAV-endemic regions Post-exposure (within 14 days) Routine – household and other intimate contacts Selected situations – institutions (e.g., day care centers) – common source exposure (e.g., food prepared by infected food handler) Dr. Salwa Tayel 17 Hepatitis A Vaccine Inactivated whole virus vaccine. Licensed for persons 1 year of age and older. Schedule 2 doses First dose then booster dose 6-18 months after first. Gives protection after 4 weeks of the fist dose. The vaccine should be administered intramuscularly. Site: deltoid muscle. Dr. Salwa Tayel 18 Indications of Hepatitis A Vaccine Persons at increased risk for infection: – travelers to intermediate and high HAV-endemic countries (Individuals who will travel to high-risk areas <4 weeks after the initial dose of vaccine should also be given IG) – MSM (Men who have sex with men) – illegal drug users – Persons who have clotting factor disorders – persons with chronic liver disease For communities with historically high rates of hepatitis A: -routine childhood vaccination Dr. Salwa Tayel 19 Dr. Salwa Tayel 20 Viral Hepatitis B (HBV) 14/2/2011 21/2/2010 Dr. Salwa Tayel 21 Serum hepatitis, serum jaundice. Clinical signs & symptoms occur more in adults. At least 50% of infections are asymptomatic Onset is usually gradual with anorexia, nausea and vomiting, often progressing to jaundice. 14/2/2011 Dr. Salwa Tayel 22 Hepatitis B – Clinical Features • Incubation period: Average 60-90 days Range 45-180 days • Clinical illness (jaundice): age <5 yrs, <10% • Acute case-fatality rate: 0.5%-1% • Chronic infection: <5 yrs, 30%-90% >5 yrs, 2%-10% >5 yrs, 30%-50% • Premature mortality from chronic liver disease: 14/2/2011 Dr. Salwa Tayel 15%-25% 23 Symptomatic Infection of Hepatitis B Virus by Age at Infection Symptomatic Infection (%) 100 80 60 40 20 Symptomatic Infection 0 14/2/2011 Dr. Salwa Tayel 24 Risk of Chronic HBV Carriage by Age of Infection 100 Carrier risk (%) 90 80 70 60 50 40 30 20 10 0 Birth 14/2/2011 1-6 mo 7-12 mo Age infection Dr. of Salwa Tayel 1-4 yrs 5+ yrs 25 Outcome of Hepatitis B Virus Infection by Age at Infection Chronic Infection (%) 100 100 80 80 60 60 Chronic Infection 40 40 20 20 Symptomatic Infection 0 14/2/2011 0 Dr. Salwa Tayel 26 CHRONIC Hepatitis B Virus Infection •Overall risk: 10% of all acute infections. •About 15%-25% of persons with chronic HBV infection might die from either cirrhosis or liver cancer •Chronic infection occurs in: ~ 90% of infants infected with HBV at birth ~ 30% of children infected at age 1- 5 years 2- 6% of people infected after age 5 years 14/2/2011 Dr. Salwa Tayel 28 Geographic Distribution of Chronic HBV Infection HBsAg Prevalence 8% - High 2-7% - Intermediate <2% - Low 14/2/2011 Dr. Salwa Tayel 29 Global Patterns of Chronic HBV Infection High (>8%): – 45% of global population – early childhood infections common Intermediate (2%-7%): – 43% of global population – infections occur in all age groups Low (<2%): – 12% of global population – most infections occur in adult risk groups 14/2/2011 Dr. Salwa Tayel 30 Cycle of infection Agent Susceptible Host IP Reservoir PC Portal of Inlet Portal of Exit Mode of transmission 14/2/2011 Dr. Salwa Tayel 31 Hepatitis B Virus HBsAg Double-Stranded DNA HBsAg HBcAg HBeAg The presence of HBsAg indicates active infection or chronic carrier. Antibody to HBsAg, from either disease or vaccine, indicates immunity. 14/2/2011 Dr. Salwa Tayel 32 Human (cases and carriers). Human blood and blood products can transmit infection if not screened for HBs Ag. Other body Fluids have the virus with varying concentrations. 14/2/2011 Dr. Salwa Tayel 33 Concentration of HBV in Various Body Fluids High blood serum wound exudates 14/2/2011 Moderate semen vaginal fluid saliva Dr. Salwa Tayel Low/Not Detectable urine feces sweat tears breast milk 34 1.Parenteral: Unsafe injections and transfusions, organ transplants, sharing needles, haemodialysis, needle sticks, tattooing , razors and toothbrushes. 2.Perinatal exposure, especially when HBs Ag carrier mothers are also HBe Ag positive. 3.Sexual exposure. 14/2/2011 Dr. Salwa Tayel 35 From 45-180 days, average 60-90 days. • 1-2 months before the onset of symptoms • during acute clinical course • during the chronic carrier state which may persist for life. 14/2/2011 Dr. Salwa Tayel 36 Elimination of HBV Transmission Strategy Prevent perinatal HBV transmission Routine vaccination of all infants Vaccination of children in high-risk groups Vaccination of adolescents & all children up through age 18 Vaccination of adults in high-risk groups 14/2/2011 Dr. Salwa Tayel 37 Hepatitis B Vaccine Currently, subunit recombinant HBs Ag • given IM in the deltoid region. • 3 dose series, typical schedule 0, 1-2, 4-6 months - no maximum time between doses (no need to repeat missed doses or restart) • Protection • ~30-50% dose 1 • 75% - dose 2 • 96% - dose 3 • lower protection in older, immunosuppressive illnesses (e.g., HIV, chronic liver diseases, diabetes), obese, smokers 14/2/2011 Dr. Salwa Tayel 38 Indication of Hepatitis B Vaccination Routine for infants. Ages 11-15 “catch up”, and through age 18 years Over 18 – high risk – Occupational risk health care workers (HCWs) – Hemodialysis patients – All clinic clients of sexually transmitted diseases (STD) – Multiple sex partners or prior STD – MSM (Men having sex with men) – IDU (injecting drug users) – Institution for developmental disability (Staff & clients) 14/2/2011 Dr. Salwa Tayel 39 14/2/2011 Dr. Salwa Tayel 40 Prevention of perinatal HBV transmission Prevent perinatal HBV transmission by: • screening all pregnant women for hepatitis B surface antigen (HBsAg) & • providing hepatitis B immune globulin (HBIG) in combination with hepatitis B vaccine to infants of HBsAg-positive mothers 14/2/2011 Dr. Salwa Tayel 41 Immunoglobulins (HBIG): (HBIG) is indicated in combination with the vaccine in: accidental needle stick injury sure sexual exposure perinatal exposure In blood banks: screening of blood donors And avoid donors from risky group. 14/2/2011 Dr. Salwa Tayel 42 Use of adequately sterilized syringes and needles or preferably use disposal equipment. Discourage risky behaviors e.g. tattooing, drug abuse and extramarital relations. Avoid transmission from persons with (e antigen), especially medical and dental personnel who routinely perform invasive procedures. Health care personnel should follow the universal precautions. 14/2/2011 Dr. Salwa Tayel 43 14/2/2011 Dr. Salwa Tayel 44 Hepatitis D (Delta) Virus d antigen HBsAg RNA HDV is a defective single-stranded RNA virus (delta Ag) 14/2/2011 Dr. Salwa Tayel It requires HBV for synthesis of envelope protein composed of HBsAg. 45 Geographic Distribution of HDV Infection Taiwan Pacific Islands HDV Prevalence High Intermediate Low 14/2/2011 Very Low No Data Dr. Salwa Tayel 46 Hepatitis D - Clinical Features • Coinfection with HBV – – severe acute disease low risk of chronic infection • Superinfection on top of chronic HBV – usually develop chronic HDV infection – high risk of severe chronic liver disease 14/2/2011 Dr. Salwa Tayel 47 Hepatitis D Virus Modes of Transmission • Percutanous exposures injecting drug use • Permucosal exposures sex 14/2/2011 contact Dr. Salwa Tayel 48 Prevention of Hepatitis D • HBV-HDV Coinfection – Pre or postexposure prophylaxis to prevent HBV infection (HBIG and/or Hepatitis B vaccine) • HBV-HDV Superinfection – Education to reduce risk behaviors among persons with chronic HBV infection 14/2/2011 Dr. Salwa Tayel 49 14/2/2011 Dr. Salwa Tayel 50 Prevalence of HCV Infection Among Blood Donors 14/2/2011 Dr. Salwa Tayel 51 Hepatitis C – Clinical Features Incubation period: Average 6 - 7 wks Range 2 – 26 wks Acute illness (jaundice) Mild (≤20%) Case fatality rate Low Chronic infection 60%-85% Chronic hepatitis 70% Cirrhosis 5%-20% Mortality from CLD : 3% 14/2/2011 Dr. Salwa Tayel 52 Natural History of HCV Infection 100 People Time 15% Resolve (15) 85% Chronic (85) 80% Stable (68) 20% Cirrhosis (17) 75% Stable (13) 25% Mortality (4) Leading Indication for Liver Transplant 14/2/2011 Dr. Salwa Tayel 53 Chronic Hepatitis C Factors Promoting Progression or Severity • Increased alcohol intake • Age > 40 years at time of infection • HIV co-infection • Others: • Male gender • Chronic HBV co-infection 14/2/2011 Dr. Salwa Tayel 54 Risk Factors Associated with Transmission of HCV • Illegal injection drug use • Transfusion or transplant from infected donor • Occupational exposure to blood – Mostly needle sticks • Iatrogenic (unsafe injections) • Birth to HCV-infected mother • Sexual/household exposure to anti-HCV positive contact • Multiple sex partners 14/2/2011 Dr. Salwa Tayel 55 Sources of Infection for Persons With Hepatitis C Injecting drug use 60% Sexual 15% Transfusion 10% (before screening) Occupational 4% Other 1%* Unknown 10% * Nosocomial; iatrogenic; perinatal 14/2/2011 Dr. Salwa Tayel Source: Centers for Disease Control and Prevention 56 Other modes of transmission: percutaneous procedures using inadequately sterilized equipment (e.g. ear and body piercing, circumcision, tattooing) HCV do not spread by sneezing, hugging, coughing, food or water, sharing eating utensils, or casual contact 14/2/2011 Dr. Salwa Tayel 57 Prevention of HCV transmission - Reduce or Eliminate Risks for Acquiring HCV Infection - Preventing HCV Transmission from patients to Others - HCV testing/ screening 14/2/2011 Dr. Salwa Tayel 58 Prevention of HCV transmission Screening and testing donors of blood, organs, and tissues Virus inactivation of plasma-derived products Risk-reduction counseling and services – Obtain history of high-risk drug and sex behaviors – Provide information on minimizing risky behavior, including referral to other services Infection control practices Blood and body fluid precautions 14/2/2011 Dr. Salwa Tayel 59 Public Health Service Guidelines for Anti-HCV-Positive Persons Anti-HCV-positive persons should: • Be considered potentially infectious • Keep cuts and skin lesions covered • Be informed of the potential for sexual transmission • Be informed of the potential for perinatal transmission – no evidence to advise against pregnancy or breastfeeding Anti-HCV-positive persons should not: • Donate blood, organs, tissue, or semen • Share household articles (e.g., toothbrushes, razors) 14/2/2011 Dr. Salwa Tayel 60 The End Thank You Website http://faculty.ksu.edu.sa/73234/default.aspx [email protected] 14/2/2011 Dr. Salwa Tayel 61