* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download L3_protein synthesis..
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Discovery and development of neuraminidase inhibitors wikipedia , lookup
Environmental impact of pharmaceuticals and personal care products wikipedia , lookup
Neuropharmacology wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Ciprofloxacin wikipedia , lookup
Psychopharmacology wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmacognosy wikipedia , lookup
Levofloxacin wikipedia , lookup
Drug interaction wikipedia , lookup
Discovery and development of cephalosporins wikipedia , lookup
Dydrogesterone wikipedia , lookup
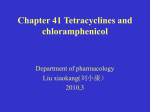
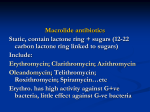
Inhibitors of bacterial protein synthesis The five general mechanisms comprise (1) inhibition of synthesis of cell wall, (2) damage to cell membrane, (3) modification of nucleic acid/DNA synthesis, (4) modification of protein synthesis (at ribosomes), and (5) modification of energy metabolism within the cytoplasm (at folate cycle). Inhibitors of bacterial protein synthesis Drugs that inhibit protein synthesis vary considerably in terms of chemical structures and their spectrum of antimicrobial activity. Chloramphenicol, tetracyclines, and the aminoglycosides were the first inhibitors of bacterial protein synthesis to be discovered with broad spectrum of antimicrobial activity. Erythromycin, an older macrolide antibiotic has a narrow spectrum of action. Azithromycin and clarithromycin (semisynthetic macrolides), clindamycin and newer inhibitors developed lately as streptogramins, linozolid, telithromycin, and tigecycline have activity against certain bacteria that have developed resistance to older antibiotics. Lists of drugs act as protein synthesis inhibitors I : Chloramphenicol Chloramphenicol is a bacteriostatic antimicrobial that became available in 1949. it was isolated from cultures of streptomyces bacteria. It inhibits bacterial protein by binding to the 50S ribosomal subunit. Chloramphenicol is considered a prototypical broad spectrum antibiotic, is effective against a wide range of gram-positive and gram-negative bacteria, including most anaerobic organisms. Because of its toxicity, its use is restricted to lifethreatening infections for which no alternative exist. Due to resistance and safety concerns, it is no longer a first-line agent for any infection. Mechanism of action of chloramphenicol Antibacterial spectrum It is a bacteriostatic broad-spectrum antibiotic that is active against both aerobic and anaerobic gram positive and gram negative organisms It is active not only against bacteria, but also against other microorganisms, such as Rickettsia. (A genus of gram-negative bacteria that are carried as parasites by many ticks, fleas, and lice and cause diseases such as typhus, scrub typhus, and Rocky Mountain spotted fever.) It is bacteriostatic for most organisms but kills (bacterocidal) for Haemophilus influenzae, Neisseria meningitidis and Bordetella pertussis (Bacteroids). • • • It is not active against Klamedia species. P. aeruginosa is resistant to even very high concentrations of the drug. Chlamydia is a genus of bacteria that are obligate intracellular parasites. Chlamydia infections are the most common bacterial sexually transmitted infections in humans and are the leading cause of infectious blindness worldwide.[The three Chlamydia species include Chlamydia trachomatis (a human pathogen), Chlamydia suis (affects only swine), and Chlamydia muridarum (affects only mice and hamsters).[ Classification and Pharmacokinetics Chloramphenicol has a simple and distinctive structure, and no other antimicrobials have been discovered in this chemical class. Chloramphenicol is extremely lipid soluble; it remains relatively unbound to protein and is a small molecule. It has a large apparent volume of distribution, and penetrates effectively into all tissues of the body, including the brain. The concentration achieved in brain and cerebrospinal fluid (CSF) is around 30 to 50%, even when the meninges are not inflamed; this increases to as high as 89% when the meninges are inflamed. Pharmacokinetics Chloramphenicol is effective orally as well as parenterally and is widely distributed readily crossing the placental and blood brain barriers. Chloramphenicol undergoes enterohepatic cycling, and a small fraction of the dose (10%) is excreted in the urine unchanged. Most of the drug is inactivated by a hepatic glucuronosyltransferase. Chloramphenicol inhibits the hepatic mixed-function oxidases. Chloramphenicol increases the absorption of iron Administration and fate of chloramphenicol Clinical uses Because of its toxicity, chloramphenicol has very few uses as a systemic drug. Chloramphenicol should be reserved for serious infections in which benefit of the drug outweighs its uncommon but serious hematological toxicity, such uses may include: Infections caused by H. influnzae resistant to other drugs. Meningitis in patients whom penicillin cannot be used. Chloramphenicol is active against the three main bacterial causes of meningitis: Neisseria meningitidis, Streptococcus pneumoniae and Haemophilus influenzae. Chloramphenicol is sometimes used for rickettsial diseases. The drug is commonly used as a topical antimicrobial agents in bacterial conjunctivitis. It is effective in typhoid fever, but ciprofloxacin or amoxicillin and co-trimoxazole are similarly effective and less toxic. Clinical use in special populations Chloramphenicol is metabolized by the liver to chloramphenicol glucuronate (which is inactive). In liver impairment, the dose of chloramphenicol must therefore be reduced. The majority of the chloramphenicol dose is excreted by the kidneys as the inactive metabolite, chloramphenicol glucuronate. Only a tiny fraction of the chloramphenicol is excreted by the kidneys unchanged. Plasma levels should be monitored in patients with renal impairment, but this is not mandatory. Chloramphenicol succinate ester (the inactive intravenous form of the drug) is readily excreted unchanged by the kidneys, more so than chloramphenicol base, and this is the major reason why levels of chloramphenicol in the blood are much lower when given intravenously than orally. Chloramphenicol passes into breast milk, so should therefore be avoided during breast feeding, if possible. Adverse effects Aplastic anemia: The most serious side effect of chloramphenicol treatment is aplastic anemia. This effect is rare and is generally fatal: there is no treatment and it is unpredictable. Aplastic anemia is severe idiosyncratic depression of the bone marrow resulting in pancytopenia (a decreased in all blood cell elements) and independent of dose and may occur after therapy ceased. Bone marrow suppression: Chloramphenicol commonly causes bone marrow suppression during treatment; this is a direct toxic effect of the drug on human mitochondria. This effect manifests first as a fall in hemoglobin levels. The anemia is dose-dependent and fully reversible once the drug is stopped. Leukemia There is an increased risk of childhood leukemia, and the risk increases with length of treatment. Adverse effects Gray baby syndrome Intravenous chloramphenicol use has been associated with the so-called gray baby syndrome. This phenomenon occurs in newborn infants because they do not yet have fully functional liver enzymes (i.e. UDPglucuronyl transferase), so chloramphenicol remains unmetabolized in the body. This causes several adverse effects, including hypotension and cyanosis. The condition can be prevented by using the drug at the recommended doses, and monitoring blood levels. Gastrointestinal disturbances: These conditions may occur from direct irritation and from superinfections, especially candidiasis (secondary to alteration of the intestinal microbial flora). Drug interactions Administration of chloramphenicol concomitantly with bone marrow depressant drugs is contraindicated. Chloramphenicol is able to inhibit some of the hepatic mixed-function oxidases and, thus, blocks the metabolism of such drugs as: warfarin, phenytoin, tolbutamide, and chlorpropamide, thereby increasing their elimination halflife, elevating their concentrations and potentiating their effects. Conversely, other drugs may alter the drug elimination. Concurrent administration of phenobarbital or rifampin, which potently induce CYPs, shortens its t1/2 and may result in subtherapeutic drug concentrations. Inhibition of the cytochrome P450 system by chloramphenicol II : Macrolides The macrolide antibiotics are large cyclic lactone ring structures with attached sugars. The main macrolide and related antibiotics are erythromycin, clarithromycin and azithromycin. Erythromycin was the first of these drugs to be used clinically as drug of choice and as alternative to penicillin in individuals who are allergic to penicillin (mainly active against grampositive organisms). Clarithromycin and azithromycin are semisynthetic derivatives of erythromycin have greater gram-negative activity than erythromycin. Telithromycin a semisynthetic derivative of erythromycin, is the first “ketolide” antimicrobial agent that has been approved. The Ketolides are active against macrolide-resistant grampositive strains. Macrolide antibiotics structure Mechanism of action of macrolide antibiotics Antimicrobial spectrum 1. Erythromycin: This drug is effective against many of the same organisms as penicillin G, and is slightly wider than that of penicillin, it may be used in patients who are allergic to the penicillins. Erythromycin is used to treat infections caused by Grampositive bacteria (e.g. Streptococcus pneumoniae) and spirochaetes, but not against most gram-negative organisms, exceptions being N gonorrhoeae and, to a lesser extent, H influenzae. Erythromycin has activity against many species of Campylobacter, Chlamydia, Mycoplasma, Legionella. Erythromycin is not active against penicillin-resistant Streptococcus pneumoniae strains (PRSP) and MRSA strains. 2. Clarithromycin: Clarithromycin is slightly more potent than erythromycin against sensitive strains of streptococci and staphylococci. Clarithromycin is as active, and its metabolite is twice as active, against H. influnzae as erythromycin. Its activity against intracellular pathogens, such as Chlamydia, Legionella, Moraxella, and Ureaplasma species and Helicobacter pylori, is higher than that of erythromycin. 3. Azithromycin: Azithromycin is far more active against respiratory infections due to H. influnzae and Moraxella cattarhalis. Azithromycin is now the preferred therapy for urithritis caused by Chlamydia trachomatis, and for Mycobacterium infections. It is also effective in gonorrhea, as an alternative to ceftriaxone and in syphilis, as an alternative to penicillin G. 4. Telithromycin: This ketolide drug has an antibacterial spectrum similar of that of azithromycin. The structural modification within ketolides neutralizes the most common resistance mechanisms (methylase-mediated and efflux-mediated) that make macrolides ineffective. The drug can be used in community-acquired pneumonia including infections caused by multidrug-resistant organisms. Pharmacokinetics Erythromycin: The erythromycin base is destroyed by gastric acid. Thus, enteric coated tablets or esterified forms of the antibiotic are administered. All are adequately absorbed upon oral administration. Intravenous administration of erythromycin is associated with a high incidence of thrombophlebitis. It distributes well to all body fluids except the CSF. it is extensively metabolized by the liver and is known to inhibit the oxidation with cytochrome P450 of several drugs for example: theophylline. It is primarily concentrated and excreted in an active form in the bile. Partial reabsorption occurs through the enterohepatic circulation. Inactive metabolites are excreted into the urine (15%). Pharmacokinetics Clarithromycin, azithromycin, and telithromycin are stable to stomach acid and readily absorbed. Food interferes with the absorption of erythromycin and azithromycin, but can increase that of clarithromycin. All these drugs are concentrate in the liver and are widely distributed in the tissues. Inflammation allows for greater tissue penetration. Azithromycin has the longest half-life and largest distribution. Telithromycin inhibit cytochrome P450 system, and all are converted to active metabolites. Clarithromycin and its metabolites (the active 14-hydroxy derivative metabolite) are eliminated by the kidneys as well as the liver. Administration an fate of the macrolide antibiotics Some properties of the macrolide antibiotics Clinical uses Erythromycin is effective in the treatment of infections caused by M pneumoniae, Corynebacterium, Bordetella pertussis, Ureaplasma urealyticum, and treponema pallidum. Erythromycin is useful as a penicillin substitute in penicillinallergic individuals with infections caused by streptococci or pneumococci. Erythromycin or tetracycline is the drug of choice for Mycoplasmal pneumonia. Erythromycin is an effective alternative for individuals who are allergic to penicillin for the prophylaxis of recurrences of rheumatic fever. Clinical uses Azithromycin has a similar spectrum of activity but is more active against Moraxella catarrhalis, Neisseria, H influnzae, and Legionella pneumophila. Because of its long half-life, a single dose of azithromycin is effective in the treatment of urogenital infections caused by Chlamydia trachomatis. Clarithromycin has almost the same spectrum of antimicrobial activity and clinical uses as erythromycin. Clarithromycin 500 mg, in combination with omeprazole, 20 mg, and amoxicillin, 1 g, each administered twice daily for 10 to 14 days, is effective for treatment of peptic ulcer disease caused by H. pylori . Adverse effects Gastrointestinal disturbance: GIT disturbances are common and unpleasant but not serious. Anorexia, nausea, vomiting, and diarrhea occasionally accompany oral administration (due to a direct stimulation of gut motility). Cholestatic jaundice: Cholestatic hepatitis is the most striking side effect (fever, jaundice, impaired liver function), probably as the result of a hypersensitivity reaction to the estolate form of erythromycin. Ototoxicity: Transient deafness has been associated with erythromycin, especially at high dosages. Allergic reactions: Among the allergic reactions observed are fever, eosinophilia and skin eruptions, which may occur alone or in combination; each disappears shortly after therapy is stopped. Inhibition of the cytochrome P450 system by erythromycin, clarithromycin, and telithromycin. “Chancroid is a bacterial infection that is spread only through sexual contact III : Aminoglycosides Aminoglycoside antibiotics had been used for treatment of serious infections due to aerobic gram-negative bacilli. Because their use is associated with serious toxicities, they have been replaced to some extent by safer antibiotics, such as the third- and fourth-generation cephalosporins, the fluoroquinolones, and the carbapenems. Aminoglycosides that are derived from Streptomyces have mycin suffixes, whereas those derived from micromonospora end in –micin. The polycationic nature precludes their easy passage across tissue membranes. All members of this family are believed to inhibit protein synthesis. Aminoglycosides structure The aminoglycoside are a group antibiotics of complex chemical structure composed of amino-modified sugars, resembling each other in antimicrobial activity, pharmacokinetic characteristics and toxicity. The main agents are gentamicin, streptomycin, amikacin, tobramycin, and neomycin. Mechanism of action of the aminoglycosides Antibacterial spectrum The aminoglycosides are effective against many aerobic gramnegative bacilli (including Peudomonas aeruginosa) and some gram-positive organisms. They most widely used against gram-negative enteric organisms and sepsis.(Sepsis is an illness in which the body has a severe response to bacteria or other germs) To achieve an additive or synergistic effect, aminoglycosides are often combined with a beta-lactam antibiotic, vancomycin, or a drug active against anaerobic bacteria. They may be given together with a penicillin in streptococcal infections and those caused by Listeria spp. and P. aeruginosa. Gentamicin and tobramycin commonly used for P. aeruginosa. Amikacin has the widest antimicrobial spectrum and can be effective in infections with organisms resistant to gentamicin and tobramycin. Pharmacokinetics Aminoglycosides are polar compounds, not absorbed after oral administration and must be given intramuscularly, or intravenously for systemic effect. Because aminoglycosides are concentration- and timedependent and also have post antibiotic effect, once-daily dosing with the aminoglycosides can be employed. This results in less toxicity and less expensive to administer. They have limited tissue penetration and do not pass the BBB. Glomerular filtration is the major mode of excretion, 50-60% of a dose being excreted unchanged within 24 hr. The plasma half-life (2-3 hr) of these drugs are greatly affected by changes in renal function. If renal function is impaired, accumulation occurs rapidly, with resultant increase the dose related toxic effects (such as ototoxicity and nephrotoxicity). Administration and fate of aminoglycosides Clinical uses Gentamicin, tobramycin, and amikacin are important drugs for the treatment of serious infections caused by aerobic gram-negative bacteria, including E. coli and Enterobacter, Klebsiella, Proteus, Providencia, Pseudomonas, and Serratia species. In most cases, aminoglycosides are used in combination with a betalactam antibiotic. Examples include their combined use with penicillins in the treatment of pseudomonal, listerial, and entercoccal infections. Pseudomonal aeruginosa infections could be treated with tobramycin alone or in combination with piperacillin or ticarcillin. Enterococci infections could be treated with gentamicin or streptomycin plus vancomycin or ampicillin. Gentamicin is the drug of choice for the treatment of tularemia. (Tularemia is usually a disease of animals. Humans can acquire tularemia when they come in contact with infected animals or are bitten by insects that have fed on an infected animal.) Clinical uses Streptomycin in combination with penicillins is used in the treatment of enterococcal carditis, tuberculosis, and plague. Because of the risk of ototoxicity, streptomycin should not be used when other drugs well serve. Owing to their toxic potential, neomycin and kanamycin are usually restricted to topical (for the conjunctiva or external ear) or oral use (e.g., eliminate bowel flora). Gentamicin is also available for topical use. Because of their toxicity with prolonged administration, aminoglycosides should not be used for more than a few days unless deemed essential for a successful or improved outcome. Once the microorganism is isolated and its sensitivities to antibiotics are determined, the aminoglycoside should be discontinued if the infecting microorganism is sensitive to less toxic antibiotics. Side effects Serious, dose-related toxic effects, which may increase as treatment proceeds, can occur with the aminoglycosides. The main hazards being ototoxicity and nephrotoxicity. 1. Ototoxicity: Its directly related to high peak plasma levels and the duration of treatment. Auditory or vestibular damage (or both) may occur with any aminoglycoside and may be irreversible. Auditory impairment or deafness is more likely with neomycin, amikacin and kanamycin while vestibular dysfunction manifested as vertigo, ataxia, and loss of balance is more likely with streptomycin, gentamicin and tobramycin. Ototoxicity may be increased by the use of other ototoxic drugs (e,g., loop diuretics, cisplatin, etc.). In the case of the auditory part of CN VIII, the symptoms are deafness or tinnitus (ringing in the ears). In the case of the vestibular part of CN VIII, the symptoms are vertigo or imbalance. Side effects 2. Nephrotoxicity: Renal toxicity usually takes the form of acute tubular necrosis. Its reversible and more common in elderly patients and in those taking nephrotoxic agents (e.g., 1st generation cephalosporins, vancomycin). Gentamicin and tobramycin are the most nephrotoxic. 3. Neuromuscular blockade: Paralysis caused by neuromuscular blockade may occur at high doses of aminoglycoside. It results from inhibition of calcium uptake. Patients with myasthenia gravis are at risk. 4. Skin reactions: Allergic skin reactions may occur in patients, and contact dermatitis may occur in personnel handling the drug. Neomycin is the agent most likely to cause this adverse effect. Tetracycline antibiotics Tetracyclines are a group of broad-spectrum bacteriostatic antibiotics that inhibit protein synthesis. The group includes tetracycline, doxycycline and minocycline. They have only minor differences in their activities against specific organisms. Their general usefulness has been reduced with the onset of bacterial resistance. Despite this, they remain the treatment of choice for some specific indications. They are so named for their four (“tetra-”) hydrocarbon rings (“-cycl-”). Classification All of the tetracycline have the basic structure shown below: Mechanism of action Tetracycline bind to the 30S ribosomal subunits, thus preventing the binding of aminoacyl-tRNA to the ribosome. Antibacterial spectrum As broad spectrum bacteriostatic antibiotics, the tetracyclines are effective against gram-positive and gram-negative bacteria, as well as organisms other than bacteria such as: Mycoplasma, Rickettsia, Chlamydia spp., spirochetes, and some protozoa (e.g., amoebae). Minocycline is also effective against N. meningitidis. The antibacterial activities of most tetracyclines are similar except that tetracycline-resistant strains may remain susceptible to doxycycline or minocycline. Pharmacokinetics The tetracyclines are generally given orally but can also be administered parenterally. Minocycline and doxycycline are lipid soluble and virtually completely absorbed. The absorption of most other tetracyclines is irregular and incomplete but is improved in the absence of food. Because tetracyclines chelate metal ions (calcium, magnesium, iron, aluminum), forming non-absorbable complexes, absorption is decreased in the presence of milk, certain antacids and iron preparations. A portion of an orally administered dose of tetracycline remains in the gut lumen, modifies intestinal flora, and is excreted in the feces. Minocycline and doxycycline are long acting tetracycline while tetracycline is short acting. Pharmacokinetics Tetracyclines are distributed widely to tissues and they bind to tissues undergoing calcification (e.g., teeth and bones). All tetracyclines enter the CSF, but levels are insufficient for therapeutic efficacy, except for minocycline. and can cross the placental barrier and concentrate in fetal bones and dentition. All the tetracyclines undergo enterohepatic cycling. Obstruction of the bile duct and hepatic or renal dysfunction can increase their half-lives. Doxycycline is excreted mainly in feces; does not accumulate significantly in renal failure, and requires no dosage adjustment, making it the tetracycline of choice for use in the setting of renal insufficiency Tigecycline, formulated only for IV use, is eliminated in the bile and has a half-life of 30-36 hours. Administration and fate of tetracyclines Effects of antacids and milk on the absorption of tetracyclines Clinical uses Primary uses: Tetracyclines are recommended in the treatment of infections caused by Mycoplasma pneumoniae (in adults), chlamydiea, rickettsiae, vibrios, and some spirochetes. Doxycycline is currently an alternative to macrolides in the initial treatment of community-acquired pneumonia caused by Mycoplasma pneumoniae. Secondary uses: Tetracyclines are alternative drugs in the treatment of syphilis. They are also used in the treatment of respiratory infections caused by susceptible organisms, for prophylaxis against infection in chronic bronchitis, in the treatment of leptospirosis, and in the treatment of acne. Leptospirosis is a bacterial disease that affects both humans and animals. Humans become infected through direct contact with the urine of infected animals or with a urine-contaminated environment ACNE Clinical uses Selective uses: Specific tetracyclines are used in the treatment gastrointestinal ulcers caused by Helicobacter pylori (tetracycline), in Lyme disease (doxycycline), and in the meningococcal carrier state (minocycline). Doxycycline is also used for the prevention of malaria and in the treatment of amebiasis. Tigecycline: It has a broad spectrum action that includes organisms resistant to standard tetracyclines. Its antimicrobial activity includes gram-positive cocci resistant to methicillin (MRSA strains) and vancomycin-resistant enterococci (VRE strains). Beta-lactamase-producing gramnegative bacteria, anaerobes, chlamydiae, and mycobacteria. The drug is formulated only for IV use. Lyme disease is a bacterial infection you get from the bite of an infected tick. Typical therapeutic applications for tetracyclines CHOLERA LIME DISEASE MYCOPLASMA PNEUMONIAE ROCKY MOUNTAIN SPOTTED FEVER CHLAMEDIAL INFECTIONS Side effects Gastrointestinal disturbances: Nausea, vomiting, and diarrhea are the most common reasons for discontinuing tetracycline medication. These effects are due to direct local irritation of the GIT. Superinfections: disturbance in the normal flora may lead to candidiasis (oral and vaginal) and more rarely to bacterial superinfections with S aureus or Clostridium difficile. Bony structure and teeth: because they chelate calcium, tetracyclines are deposited in growing bones and teeth, causing staining and sometimes dental hypoplasia and bone deformity. Fatal hepatotoxicity: high doses of tetracyclines, especially in pregnant patients and those with preexisting hepatic disease, may impair liver function and lead to liver necrosis. Side effects Phototoxicity (sensitization to sunlight): tetracyclines, especially demeclocycline, may cause enhanced skin sensitivity to ultraviolet light. Vestibular disturbances: dose-dependent reversible dizziness and vertigo have been reported with doxycycline and minocycline. Tetracyclines other than doxycycline may accumulate to toxic levels in patients with impaired kidney function. High doses of tetracyclines can decrease protein synthesis in host cells, an anti anabolic effect that may result in renal damage. The tetracyclines should not be employed in pregnant or breast-feeding woman or in children less than 8 years of age. Phototoxicity Important information about tetracycline( summary) Do not use tetracycline if you are pregnant. It could cause harm to the unborn baby, including permanent discoloration of the teeth later in life. Tetracycline can make birth control pills less effective. Use a second method of birth control while you are taking this medicine to keep from getting pregnant. Tetracycline passes into breast milk and may affect bone and tooth development in a nursing baby. Do not give this medicine to a child younger than 8 years old. Tetracycline can cause permanent yellowing or graying of the teeth, and it can affect a child's growth. Avoid exposure to sunlight or artificial UV rays (sunlamps or tanning beds). Tetracycline can make your skin more sensitive to sunlight and sunburn may result. Use a sunscreen (minimum SPF 15) and wear protective clothing if you must be out in the sun. Do not take iron supplements, multivitamins, calcium supplements, antacids, or laxatives within 2 hours before or after taking tetracycline. These products can make this medicine less effective. Throw away any unused tetracycline when it expires or when it is no longer needed. Do not take this medicine after the expiration date on the label has passed. Expired tetracycline can cause a dangerous syndrome resulting in damage to the kidneys. Inhibitors of metabolism (antifolate drugs) Antimicrobial agents that interfere with folate synthesis or action (antifolate drugs) The antifolate drugs used in the treatment of infectious diseases are the sulfonamides, which inhibit microbial enzymes involved in folic acid synthesis, and trimethoprim, a selective inhibitor of dihydrofolate reductase. The importance of sulfonamides has declined due to increasing resistance. The only drugs still commonly used are sulfamethoxazole (usually in combination with trimethoprim as cotrimoxazole), sulfasalazine (poorly absorbed in the gastrointestinal tract, used to treat ulcerative colitis) and occasionally sulfadiazine. Structures of two representative sulfonamides and trimethoprim Mechanisms of action Sulfonamide is a structural analogue of p-aminobenzoic acid (PABA), which is an essential precursor in the synthesis of folic acid, required for the synthesis of DNA and RNA in bacteria. Sulfonamides as antimetabolites of PABA, they are competitive inhibitors of the enzyme dihydropteroate synthetase . They can also act as substrates for this enzyme, resulting in the synthesis of nonfunctional forms of folic acid. The selective toxicity of sulfonamides results from the inability of mammalian cells to synthesize folic acid; they must use preformed folic acid that is present in the diet. The action of sulfonamide is to inhibit growth of the bacteria, not to kill them; thus it is bacteriostatic rather than bactericidal. Mechanisms of action Trimethoprim is structurally similar to folic acid, and is a selective inhibitor of bacterial dihydrofolate reductase that prevents formation of the active tetrahydro form of folic acid (tetrahydrofolate coenzymes required for purine, pyrimidine, and amino acid synthesis). Trimethoprim plus sulfamethoxazole: When the two drugs are used in combination, antimicrobial synergy results from the sequential blockade of folate synthesis. The drug combination is bactericidal against susceptible organisms. Inhibitory effects of sulfonamides and trimethoprim on folic acid synthesis Inhibition of tetrahydrofolate synthesis by sulfonamides and trimethoprim Pharmacokinetics Sulfonamides are weakly acidic compounds, given orally and are well absorbed (except, sulfasalazine), and widely distributed in the body. The drug pass into inflammatory exudates and cross both placental and blood brain barriers. They are metabolized mainly in the liver, the major product being an acetylated derivative that lacks antibacterial action and eliminated by the kidney. Trimethoprim is well absorbed orally, and widely distributed throughout the tissues and body fluids. It reaches high concentrations in the lungs and kidneys, and fairly high concentrations in the cerebrospinal fluid (CSF). When given with sulfamethoxazole, about half the dose of each is excreted within 24 hr. Because trimethoprim is a weak base, its elimination by the kidney increases with decreasing urinary pH. Administration and fate of the sulfonamides Administration and fate of co-trimoxazole Antibacterial spectrum Sulfonamides are active against selected Enterobacteria in the urinary tract and Nocardia. In addition, sulfadiazine, in combination with the dihydrofolate reductase inhibitor pyrimethamine, is preferred form of treatment for toxoplasmosis. The antibacterial spectrum of trimethoprim is similar to that of sulfamethoxaole. However, trimethoprim is 20- to 50-fold more potent than the sulfonamide. Trimethoprim may be used alone in the treatment of acute urinary tract infections and in the treatment of bacterial prostatitis (although fluoroquinolones are preferred) and vaginitis. Antibacterial spectrum Trimethoprim is more lipid soluble than sulfamethoxazole and has a greater volume of distribution. Administration of one part trimethoprim to five parts of the sulfa drugs produces a ratio which is optimal for the antibiotic effect. Co-trimoxazole shows greater antimicrobial activity than equivalent quantities of either drug used alone. It is effective in treating urinary tract infections and respiratory tract infections as well as in pneumonia and ampicillin- or chloramphenicol-resistant systemic salmonella infections. Synergism between trimethoprim and sulfamethoxazole inhibits growth of Escherichia coli Clinical use I. Sulfonamides: The sulfonamides are active against gram-positive and gramnegative organisms, Chlamydia, and Nocardia. - Simple urinary tract infections- Oral (triple sulfa, sulfisoxazole). -Ocular infections – Topical (sulfacetamide). -Burn infections – Topical (mafenide, silver sulfadiazine) -Ulcerative colitis, rheumatoid arthritis – Oral (sulfasalazine). -Toxoplasmosis – Oral (sulfadiazine plus pyrimethamine). II. Co-trimoxazole: This drug combination is effective orally in the treatment of urinary tract infections and respiratory, ear, and sinus infections caused by Haemophilus influnzae and Moraxella catarhalis. It is used for treatment of severe Pneumocystits pneumonia and for gram-negative sepsis Adverse effects Sulfonamides may have the following adverse effects: Hypersensitivity: allergic reactions, including skin rashes and fever, occur commonly. Gastrointestinal: nausea, vomiting, and diarrhea and mild hepatic dysfunction may occur. Hematotoxicity: granlocytopenia, thrombocytopenia, and aplastic anemia. Nephrotoxicity: sulfonamides may precipitate in the urine at acidic pH, causing crystalluria and hematuria. Sulfonamides can displace bilirubin from plasma proteins, with the risk of kernicterus (bilirubin-induced brain dysfunction) in the neonate if used in the third trimester of pregnancy. Adverse effects Trimethroprim can produce the effects of folic acid deficiency (blood disorders), including megaloblastic anemia, leukopenia and granulocytopenia. These blood disorders can be reversed by the simultaneous administration of folinic acid, which does not enter bacteria. Co-trimoxazole: may cause any of the adverse effects associated with the sulfonamides. AIDS patients given co-trimoxazole have a high incidence of adverse effects, including fever, rashes, leukopenia, and diarrhea.