* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download soung_htn
Survey
Document related concepts
Adherence (medicine) wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Neuropharmacology wikipedia , lookup
Theralizumab wikipedia , lookup
Transcript
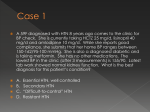
Hypertension: Case Studies Michael Soung, MD, FACP Virginia Mason Medical Center General Internal Medicine JNC 8? Current NHLBI guideline in development: JNC 8 (Hypertension) ATP IV (Cholesterol) Obesity 2 “Integrated Cardiovascular Risk Reduction Guideline” Why the delay? Intensified focus on evidence-based recommendations IOM 2011 reports on systematic reviews and guideline development http://www.nhlbi.nih.gov/guidelines/ -- Accessed Oct 2012 JNC 8? 3 clinical questions: When to initiate drug treatment? How low should BP be lowered? How do you get there? http://www.ahdbonline.com/node/1009 -- Accessed Oct 2012 Question #1 60 yo man w/ PMH HTN, hyperlipidemia, smoking. Meds include lisinopril 40mg qAM, HCTZ 25mg qAM, amlodipine 10mg qAM. Average bp 145/90. Which of the following is the next best step in management? A) Add losartan 25mg daily B) Increase HCTZ to 50mg daily C) Increase Lisinopril to 80mg daily D) Switch lisinopril dosing to bedtime E) No change in medications MAPEC study 2156 patients w/ untreated or resistant HTN (not well-controlled w/ ≥ 3 anti-HTsives) Intervention: Untreated: monotherapy -- morning vs. bedtime Resistant: (Replace 1 drug and take all BP meds in morning) vs. (Shift ≥ 1 BP med to bedtime dosing) Primary composite CV outcome at 5.6y: Bedtime dosing: RR 0.39 (0.29-0.51) 16 fewer CV events per 1000 patient-years 2 fewer deaths per 1000 patient-years Chronobiol Int 2010;27:1629-1651 MAPEC study Chronobiol Int 2010;27:1629-1651 MAPEC study Single-center (Spain), open-label, choice of meds left up to providers, use of ambulatory BP monitoring No difference in clinic BPs or awake ambulatory BP monitoring Lower sleep-time ambulatory BP monitoring Similar results in DM and CKD subgroup analyses Ann Intern Med 2012;156:JC6-8 Answer: D Chronobiol Int 2010;27:1629-1651 Diabetes Care 2011;34:1270-1276 J Am Soc Nephrol 2011;22:2313-21 J Fam Pract 2012;61:153-155 Question #2 52 yo man, initial clinic visit. Long history of inconsistently treated HTN. No current meds. Average BP over the last 6 months: 150/85. Trace LE edema on exam. Serum creatinine 3.1 (eGFR 21). Cr 3 months ago was 2.9. K 4.5 Urine albumin/creatinine ratio = 600 mg/g. Fasting glucose 98, HbA1c = 5.4%. Renal Ultrasound: medical renal disease, no hydronephrosis. Question #2 Which of the following is the most appropriate anti-hypertensive? A) Hydrochlorothiazide B) Benazepril C) Diltiazem D) Amlodipine E) Metoprolol HTN and Chronic Kidney Disease JNC 7: urinalysis in patients w/ HTN (consider urinary albumin) NKF K/DOQI guidelines: Assess for proteinuria in patients with CKD Proteinuria is strong predictor of both CKD progression and cardiovascular disease Proteinuria as a target of therapy JAMA 2003;289:2560-2572 Am J Kidney Dis 2004;43:S1-S290 HTN and Chronic Kidney Disease ACE inhibitors for nondiabetic CKD: Meta-analysis of 11 RCTs RR 0.70 (13.2% vs 20.5%) for renal outcomes (doubling of serum Cr or ESRD) Strongest benefit if proteinuria >0.5 g/ day No major differences between individual ACE-inhibitors and ARBs Ann Intern Med 2001;135:73-87 Am J Kidney Dis 2004;43:S1-S290 HTN and Chronic Kidney Disease What about advanced CKD? Largely excluded from earlier ACE-I trials ACE-I in advanced, nondiabetic, proteinuric CKD 224 patients, serum Cr 3.1-5.0 mg/dL, Uprot > 0.3g/d Benazepril 20mg daily, 3.4 year f/u Primary outcome: doubling of Cr, ESRD, death RR 0.57 (41% vs 60%) for benazepril group ***Started low (10mg), checked weekly labs (Cr, K)*** ACE-I: check Cr and K in 1-2 wks Up to 30-35% increase in serum Cr is okay (beneficial), unless hyperkalemia (> 5.6) develops Answer: B NEJM 2006;354:131-140 Arch Intern Med 2000;160:685-693 Question #3 66yo woman w/ PMH HTN, CKD w/ proteinuria. Meds include lisinopril 40mg daily and amlodipine 10mg daily. Average BP 150/90. No S3, lungs clear, trace BLE edema on exam. Serum Cr 1.2, Urine alb/Cr ratio: 1400 mg/g. Which of the following is the most appropriate anti-hypertensive? A) Metoprolol B) Hydralazine C) Losartan D) Hydrochlorothiazide E) Doxazosin ACE-inhibitors plus ARBs ONTARGET (NEJM 2008;358:1547-59 / Lancet 2008;372:547-53.) Ramipril vs telmisartan vs dual-therapy 25,620 pts w/ CVD or high-risk DM No improvement in primary CV outcome Improved urinary albumin Worsened major renal outcomes (~1% ARI) VALIANT (NEJM 2003;349:1893-906) Captopril vs valsartan vs dual-therapy 14,808 pts w/ recent MI c/b CHF No difference in mortality or CV outcomes 1-3% ARI in drug discontinuation (hypotension, renal) ACE-inhibitors plus ARBs CHARM-Added (Lancet 2003;362:767-71) Candesartan vs placebo 2548 pts w/ CHF on ACE-inhibitors 4.8% ARR in CV death or CHF hospitalization 7% ARI in drug discontinuation Val-HeFT (NEJM 2001;345:167-75) Valsartan vs placebo 5010 pts w/ CHF (93% on ACE-inhibitors) 4.4% ARR in CHF hospitalization (mortality unchanged) 2.2% ARI in drug discontinuation Worse outcome if already on both ACE-I and β-blocker ACE-inhibitors plus ARBs Meta-analysis Worsened renal function: RR 2.17 Hyperkalemia: RR 4.87 Symptomatic Hypotension: RR 1.50 Meta-analysis of dual-therapy in CHF: of dual-therapy in proteinuria No difference in mortality or CV events Hypotension: RR 2.21 Arch Intern Med 2007;167:1930-1936 Nephrol Dial Transplant 2011;26:2827-2847 ACE-inhibitors plus ARBs Pros: Improves albuminuria and blood pressure Possible benefit in heart failure Cons: May worsen hard renal outcomes More hyperkalemia More symptomatic hypotension Generally avoid dual-therapy w/ ACE-I and ARB HTN and Chronic Kidney Disease Diuretics recommended in CKD and HTN NKF K/DOQI Grade A recommendation for most pts w/ CKD and HTN Thiazides if GFR ≥ 30 mL/min Loop diuretics if GFR < 30 mL/min Combination for volume overload / edema Non-dihydropyridine calcium-channel blockers also reduce proteinuria Answer: D Am J Kidney Dis 2004;43:S1-S290 Question #4 67 yo woman w/ PMH of DM II, HTN, and hyperlipidemia, on metformin 1000mg BID, lisinopril 10mg daily, and atorvastatin 20mg daily. Average BP:135/85. HbA1c 7.8%, Cr 0.9, Urine alb/cr ratio 16 mg/g. What of the following is the most appropriate next step in her blood pressure management? A) Add diltiazem B) Add amlodipine C) Add hydrochlorothiazide D) Increase the dose of lisinopril E) No change in blood pressure meds Blood pressure targets in diabetes JNC 7: Goal blood pressure < 140/90 Exceptions: Diabetes Mellitus Chronic Kidney Disease goal blood pressure < 130/80 JAMA 2003;289:2560-2572 Blood pressure targets in diabetes ACCORD BP trial 4733 pts w/ high-risk DM, HbA1c ≥ 7.5% SBP goals of <120 vs <140 mmHg SBPs achieved: 119 vs 133.5 mmHg No change in primary CV outcome at 4.7y • reduction in CVA: 0.32% vs 0.53% SBP <120: ↑ serious adverse events (ARI 2%) No difference for microvascular outcomes NEJM 2010;362:1575-85 Kidney Int 2012;81:586-594 Blood pressure targets in diabetes 2011 meta-analysis (broad inclusion): 13 RCTs, 37,736 pts, BP <135 vs <140 No difference in overall macro/microvacular outcomes ↓ mortality by 10% (BP 130-135), ↓ CVA by 17% ↑ serious adverse effects by 20% 2012 meta-analysis (strict inclusion): 5 RCTs, 7312 pts, DBP <75-80 vs <90, + ACCORD No difference in mortality or MI ↓ CVA by 35% (1% ARI) Answer: E Circulation 2011;123:2799-2810 Arch Intern Med 2012;172:1296-1303 Blood pressure targets in CKD? JNC 7 & NKF K/DOQI: < 130/80 Extrapolated from recommendations for other high-risk groups (e.g. diabetes) Annals 2011 systematic review: 3 RCTs, 2272 patients No clear benefit from lower BP targets Possible benefit in proteinuric patients Await SPRINT (2018) and HALT-PKD (2013) Am J Kidney Dis 2004;43:S1-S290 Ann Intern Med 2011;154:541-548 Question #5 62 yo man w/ long history of HTN on max doses of lisinopril, hydrochlorothiazide, and amlodipine. Average bp: 155/95. No JVD, lungs clear, no LE edema. Serum electrolytes, glucose, creatinine, EKG normal. Negative secondary HTN workup. Which of the following is the most appropriate next step in management? A) Hydralazine B) Metoprolol C) Spironolactone D) Doxazosin E) Clonidine Resistant Hypertension = failure to reach goal BP w/ full doses of appropriate 3-drug regimen including a diuretic Multiple potential causes Secondary HTN (e.g. 1° hyperaldo, RAS) Improper measurement (e.g. cuff too small) Nonadherence, inadequate doses Drug-induced: NSAIDs, decongestants, OCPs, steroids, cocaine, amphetamines Excessive alcohol use, obesity JAMA 2003;289:2560-2572 Resistant Hypertension ASCOT-BPLA Uncontrolled, nonrandomized ASCOT cohort 1411 pts who received spironolactone as fourth-line anti-hypertensive Exclusions: hyperaldosteronism or receipt for another indication (CHF, liver failure) Median dose = 25mg Mean bp reduction: 22 / 10 mmHg Dosing: 12.5 - 50mg daily Side effects: gynecomastia (6%), hyperkalemia (monitor closely!) Answer: C Hypertension 2007;49:839-845 Question #6 85 yo woman w/ PMH HTN and chronic stable angina on ASA and metoprolol. No CP, SOB, edema, HAs, lightheadedness. Healthy diet, regular exercise. Average BP: 165/85. HR 60, nl CV exam, no edema. Cr 0.9, K 4.2, UA neg. Which of the following is the most appropriate next step in management? A) Add indapamide B) Add lisinopril C) Add amlodipine D) Increase metoprolol dose E) No change in blood pressure meds HTN in the very elderly Few patients >80yo included in previous HTN trials JNC 7 recommends same management for elderly (but w/ lower initial drug doses) Previous meta-analysis of HTN treatment in pts >80yo suggested reduced CVA risk but trend towards increase mortality JAMA 2003;289:2560-2572 NEJM 2008;358:1887-98 HTN in the very elderly HTN in the Very Elderly Trial (HYVET) 3845 healthy pts, age 80+, SBP ≥ 160 mmHg Indapamide +/- perindopril vs placebo Target blood pressure: 150/80 2y f/u: 48% of Rx group reached target (vs 20% placebo); mean difference 16/6 mmHg CVA: 5.3 fewer per 1000 pt-yrs Death (any cause): 12.4 fewer per 1000 pt-yrs Fewer serious adverse events in Rx group NEJM 2008;358:1887-98 HTN in the very elderly 2010 Cochrane review on anti-HTsive drug treatment in the very elderly: CV mortality / morbidity: RR 0.75 (0.65-0.87) Total mortality: RR 1.01 (0.90-1.13) Withdrawals due to adverse effects: RR 1.71 (1.45-2.00) Answer: A Cochrane Database of Systematic Reviews 2010 Question #7 63 yo man w/ PMH of HTN, CHF, asthma, gout. Meds include lisinopril, fluticasone / salmeterol INH, allopurinol. Average BP 145/90, HR 68, lungs are clear, no S3, trace BLE edema, a few gouty tophi. Which of the following is the most appropriate anti-hypertensive? A) Diltiazem B) Amlodipine C) Doxazosin D) Hydrochlorothiazide E) Metoprolol Βeta-blockers and lung disease Cochrane reviews on cardioselective beta-blockers in: COPD: 22 RCTs in pts w/ COPD No change in FEV1 or symptoms No change in response to β2-agonists Reversible airway disease (asthma/COPD): 29 RCTs in pts w/ reversible airway disease No change in FEV1 or symptoms No change in response to β2-agonists Cochrane Database of Systematic Reviews 2008 Anti-HTsives in systolic heart failure Drugs Who? ACE-I/ARB All ↓ mortality? ↓ morbidity? Carvedilol / All metoprolol ER Aldosterone Class III or antagonists IV Diuretics Class II - IV Hydralazine / Nitrates ACE-I/ARB intolerant Answer: E Ann Intern Med 2010;152:ITC61-15 Question #8 37 yo woman w/ 5-year history of HTN comes for pre-pregnancy counseling. Stopped her OCP and lisinopril 3 weeks ago. Average BP since: 160/90. No edema on exam, serum electrolytes, Cr, UA all normal. Which of the following is the most appropriate next step in management? A) Hydrochlorothiazide B) Losartan C) Labetalol D) Atenolol E) No medication Chronic Hypertension in Pregnancy Prevalence in U.S.: 3% and rising ↑ risk for preeclampsia, placental abruption, fetal growth restriction, preterm birth, C-section Treatment reduces risk for severe HTN (but not the above outcomes) BP typically falls late 1st trimester, rises to prepregnacy values during 3rd trimester Cochrane: insufficient evidence to determine appropriate BP targets in pregnancy Recommendations for starting therapy range from >150-180/100-110, variable targets NEJM 2011;365:439-46 Cochrane Database of Systematic Reviews 2011 Chronic Hypertension in Pregnancy First-line: Second-line: Methyldopa: longest safety record, somnolence limits tolerability Labetalol: better tolerated, good safety data • (Atenolol: fetal-growth restriction) Long-acting CCBs: less safety data but appears safe Diuretics: previously considered unsafe but review of 9 RCTs no difference in pregnancy outcomes Contraindicated: ACE-I / ARBs: teratogenic, oligohydramnios Answer: C NEJM 2011;365:439-46 Question #9 72 yo woman w/ PMH of HTN, atrial fibrillation (EF 60%), and hyperlipidemia. Medications include HCTZ 25mg daily, digoxin 0.125mg daily, warfarin 5mg daily, and simvastatin 40mg daily. Average BP 135/85, HR 90-110. Which of the following is the most appropriate next step in management? A) Start metoprolol B) Start diltiazem C) Start amiodarone D) Start amlodipine E) Increase digoxin dose Atrial Fibrillation management 2006 ACC/AHA/ESC Guidelines: Recommended equally for rate control: Beta-blockers Nondihydropyridine calcium channel blockers Digoxin: Slows HR at rest, but not w/ exercise, in Afib Not generally recommended for monotherapy Circulation 2006; 114:700-752 Drug interactions SEARCH trial Simvastatin 20mg vs 80mg w/ hx of MI Non-significant 6% RRR in CV events 80mg dose: ↑↑ myopathy • Excess rate: 4/1000 in 1st year, 1/1000 thereafter Increased risk in women and elderly Risk doubled w/ calcium channel blocker (particularly diltiazem) Lancet 2010;376:1658–1669 www.fda.gov/Drugs/DrugSafety/ucm256581.htm Drug interactions 2011 FDA simvastatin warning: Do not exceed 10mg simvastatin daily with: Diltiazem, Verapamil Do not exceed 20mg simvastatin daily with: Amlodipine, Amiodarone 2012 FDA lovastatin warning: Do not exceed 20mg lovastatin daily with: Diltiazem, Verapamil Answer: A www.fda.gov/Drugs/DrugSafety/ucm256581.htm www.fda.gov/Drugs/DrugSafety/ucm283137.htm www.fda.gov/Drugs/DrugSafety/ucm293101.htm Question #10 50 yo man w/ hx of difficult-to-control HTN and recurrent headaches. Average BP 165/95 on HCTZ 25mg daily, felodipine 10mg daily, metoprolol 100mg BID, and lisinopril 40mg daily. Taking all meds as prescribed, no supplements, checking BPs appropriately. On exam, he is obese, HR 80, funduscopic exam shows AV nicking, trace leg edema. Labs show K 3.0 and Cr 1.0 prior to starting lisinopril. Since then, stable K 3.2 and Cr 1.3. UA trace protein. Question #10 Which of the following is the most appropriate test? A) Sleep study B) Serum aldosterone / renin ratio C) Plasma free metanephrines D) MRA of renal arteries E) 24-hour urinary cortisol Secondary Hypertension Consider workup if: Severe or resistant hypertension New-onset HTN at age <25 Malignant HTN Signs / symptoms of a specific secondary cause Rule out other causes of resistant HTN (see previous slide; e.g. med nonadherence , other meds, improper measurement, etc) Ann Intern Med 2008;149:ITC61-16 JAMA 2003;289:2560-2572 UpToDate 2011 Secondary Hypertension (By ascending age:) Coarctation of the aorta: Children, young adults >20mmHg difference between arm & leg SBP Diminished / delayed femoral pulses Initial test: Echocardiogram Fibromuscular dysplasia (Renal artery stenosis): Young adults, typically women Acute, >30-35% increase in serum Cr w/ ACE-I / ARB Renal bruits Initial test: CTA, MRA, Duplex U/S of renal arteries Am Fam Physician 2010;82:1471-1478 UpToDate 2011 Secondary Hypertension Pheochromocytoma: Rare. Middle-aged adults Paroxysms of elevated BPs, esp w/ HA, palpitations, sweats, flushing Initial test: plasma free metanephrines Cushing’s Syndrome: Middle-aged adults (depending on cause) Moon facies, buffalo hump, central obesity, dark abdominal striae Initial test: 24-hour urine cortisol, late-night salivary cortisol, low-dose dexamethasone suppresion test Am Fam Physician 2010;82:1471-1478 UpToDate 2011 Secondary Hypertension Primary hyperaldosteronism: Middle-aged adults Hypokalemia (though >1/2 are normokalemic) Common: 6% of pts w/ HTN Initial test: serum aldosterone / renin ratio Obstructive Sleep Apnea: Middle-aged (and younger) adults Snoring, apneic events, daytime somnolence Initial test: sleep study Am Fam Physician 2010;82:1471-1478 UpToDate 2011 Secondary Hypertension Renal artery stenosis (atherosclerotic) Older, vascular disease Acute, >30-35% increase in serum Cr w/ ACE-I / ARB Renal bruits Initial test: CTA, MRA, Duplex U/S of renal arteries Medical management as effective as revascularization without clear indications Other causes: Thyroid dysfunction 1° hyperPTH Renal parenchymal disease Answer: B Am Fam Physician 2010;82:1471-1478 UpToDate 2011 Question #11 42 yo man w/ new diagnosis of HTN, average BP 145/90 after intensive lifestyle improvements. Normal serum electrolytes and creatinine, UA negative, EKG wnl. Otherwise healthy. Which of the following is the most appropriate next step in management? A) Lisinopril B) Chlorthalidone C) Amlodipine D) Hydrochlorothiazide E) Atenolol F) No medication, continued monitoring Initial Therapy in HTN JNC 7: Thiazide diuretics for most patients Hydrochlorothiazide = most common But not widely used in studies at current doses HCTZ 12.5-25mg: weaker reduction in BP vs all other drug classes No CV morbidity or mortality outcomes data at low doses (except in combo w/ triamterene or amiloride) JAMA 2003;289:2560-2572 J Am Coll Cardiol 2011;57:590-600 Hypertension 2009;54:951-953 Cochrane Database of Systematic Reviews 2009 Initial Therapy in HTN Some recommend chlorthalidone: Longer half life, 1.5-2x as potent (vs HCTZ) (12.5mg chlorthalidone ≈ 25mg HCTZ) Used in ALLHAT, SHEP 2012 network meta-analysis of CTD vs HCTZ: greater CV benefit w/ similar BP reduction Caveats: Less available (few combo pills, higher cost) No 12.5mg dose (need to halve a 25mg pill) More hypokalemia Hypertension 2009;54:951-953 Hypertension 2011;57:689;694 Hypertension 2012;59:1110-1117 Initial Therapy in HTN BMJ 2009 meta-analysis: All classes similar efficacy for reducing CHD events and CVA Beta-blockers extra protection first few years post-MI CCBs slight advantage for CVA prevention Cochrane 2009 meta-analysis: Low-dose thiazides (HCTZ <50mg/day, chlorthalidone <50mg/day): strongest evidence ACE-I: similar benefit, less evidence CCBs: insufficient evidence β-blockers (atenolol) and high-dose thiazides: inferior BMJ 2009;338:b1665 Cochrane Database of Systematic Reviews 2009 Initial Therapy in HTN ACCOMPLISH trial: 11,506 pt w/ high-risk HTN Benazepril plus (amlodipine or HCTZ) Target BP <140/90 (<130/80 for DM or CKD) Similar BPs achieved Primary composite CV outcome at 3y: • Benazepril-amlodipine: 9.6% • Benazepril-hydrochlorothiazide: 11.8% NEJM 2008;359:2417-2428 Initial Therapy(?) in HTN Cochrane 2012: mild hypertension BP 140-159 / 90-99, primary prevention 4 RCTs, 8912 patients, 4-5y f/u No change in mortality, CHD, CVA, CV events 9% ARI of withdrawals due to adverse effects Caveats: Low event rates, mostly driven by a single trial (MRC), half on propranolol-based Rx Wide confidence intervals Long enough follow-up? Cochrane Database Syst Rev 2012;8 :CD006742 Anti-HTsives in normotension JAMA Anti-HTsives in normotensive patients w/ CVD 25 RCTs, 64,000 patients ↓ mortality, CVA, MI, CHF, total CVD events Eur 2011 meta-analysis: Heart J 2012 meta-analysis: ACE-I or ARB in normotensive patients w/ CVD or CVD risk factors 13 RCTs, 80,000 patients ↓ composite CV endpoint, CV mortality JAMA 2011;305:913-922 Eur Heart J 2012;33:505-514 Initial Therapy in HTN Sigh… Consider overall CV risk when managing mild HTN Really push lifestyle changes My current approach to meds: 1st line: Lisinopril, HCTZ/triam, or chlorthalidone (depending on potassium level), or no med if low risk Still using lisinopril-HCTZ due to low cost and convenience -- dosing qhs or BID Amlodipine before beta-blockers JNC 8?? Answer: A, B, C, D, F? Take home points Dose ≥1 BP med at bedtime Use ACE-inhibitors for proteinuric CKD (even with very high Cr) Avoid combining ACE-I & ARB No benefit from tight BP control in DM (or CKD?) Add spironolactone for resistant HTN Treat systolic HTN in octogenarians (with caution) Take home points Beta-blockers okay with chronic asthma & COPD Use labetolol in pregnancy Avoid CCBs with ≥10-20mg of simvastatin or lovastatin (or switch statins) Watch for clues suggesting secondary causes of HTN (hypoK & hyperaldo) First-line Rx: variety of reasonable options Not atenolol Consider chlorthalidone over HCTZ No clear benefit from meds in low-risk mild HTN