* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Slide 1
Drug discovery wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Discovery and development of neuraminidase inhibitors wikipedia , lookup
Psychopharmacology wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Prescription costs wikipedia , lookup
Discovery and development of non-nucleoside reverse-transcriptase inhibitors wikipedia , lookup
Pharmacognosy wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Neuropharmacology wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
Levofloxacin wikipedia , lookup
Ciprofloxacin wikipedia , lookup
Drug interaction wikipedia , lookup
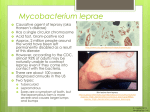
A. Characteristics I. Slowly growing organism; making them relatively resistant to antibiotics II. Mycobacterial cells can also be dormant and thus completely resistant to many drugs III. Lipid rich mycobacterial cell wall is impermeable to many agents IV. Substantial proportion of mycobacterial organism are intracellular, residing with macrophages and inaccessible to drugs V. Notorious for their ability to develop resistance to any single drug B. Agents Drugs used in Tuberculosis Drugs used in Atypical mycobacteria Drugs used in Leprosy Drugs used in Tuberculosis First line Anti TB Drugs 1)Isoniazid 2)Rifampin 3)Pyrazinamide 4)Ethambutol 5)Streptomycin Isoniazid The most active drug for the treatment of TB (1952), a small (MW 137) simple molecule freely soluble in water Bactericidal; active-intracellular and extracellular organisms Less effective in atypical mycobacteria MOA: inhibits synthesis of mycolic acid Availability: 50, 100, 300mg tab; 100-200mg/5ml susp. Resistance - due to mutations: a. inhA b. katG c. ahpC d. kasA - if used as a single drug, 10-20% prevalence Kinetics: readily absorbed in the GIT; serum conc. 35ug/ml in 1-2 hrs.; acetylation by liver N-acetyltransferase (rapid acetylators vs. slow acetylators); urine Dynamics: dose: 5mgkd (child) or 300mgd (adult) daily 15mgkd or 900mg in twice weekly dosing + rifampin 600mg - add Pyridoxine 25-50mgd if (+) neuropathy - as a single agent in cases of: a. recent converters b. immunocompromised individuals c. close contacts d. abnormal CXR but activity has been R/O 300mgd or 900mg twice weekly x 6 mos. Adverse effects: a. allergic reactions – fever, rashes, drug-induced SLE b. hepatitis – major toxic effect; age-dependent; 10-20% asymptomatic; if with clinical hepatitis, D/C INH; acetylhydrazide c. peripheral neuropathy – seen in 10-20% being given >5mgkd d. misc. reactions – hematologic abnormality, GI discomfort Drug interaction: phenytoin, AlOH Rifampin A large (MW 823) complex semisynthetic derivative of Rifamycin ( Streptomyces mediterranei) Active against gm (+), gm(-) cocci, some enteric bacteria, chlamydia Cross resistance with Rifabutin Bactericidal; penetrates intracellularly MOA: binds with the β-subunit of bacterial DNA dependent RNA polymerase → inhibit RNA synthesis Resistance: mutations in rpoβ Kinetics: well absorbed; highly protein-bound (↑ in CSF in meningeal inflammation); excreted in bile, feces, urine; undergoes enterohepatic recirculation Clinical uses: a. mycobacterial infection 600mgd (10mgkd) + INH, Ethambutol x 6 mos. atypical mycobacteria 600mgd or 2x weekly x 6 mos. leprosy 600mgd or 2x weekly x 6 mos. + sulfone b. other indications: meningococcal carriage 600mgd x 2 days H. influenzae typeB contact – 20mgkd x 4 days staph. - + another agent pneumococci (meningitis) - + ceftriaxone or vancomycin Adverse effect: a. orange color urine, sweat, tears, contact lens b. cholestatic jaundice c. flu-like syndrome – if given < 2x weekly d. hepatitis – occ. Drug interaction: microsomal enzyme inducer (methadone, anticoagulant, protease inhibitor, some anticonvulsant, ketoconazole, contraceptive, cyclosporine, chloramphenicol) Ethambutol Synthetic, water-soluble, heat stable compound MOA: inhibitor of mycobacterial arabinosyl transferase (involved in the polymeration of arabinoglycan, an essential component of mycobacterial cell wall barrier) by embCAB operon Resistance: mutations within the embB structural gene or overexpression of emb gene products Kinetics: well wbsorbed; CSF conc. –variable (469% in inflammed meninges); excreted 20% feces, 50% urine (reduced dose by half if with renal failure) Dose: 15-25 mgkd + INH + Rifampin 50mgkg twice weekly dosing Adverse effect: retrobulbar neuritis – most common; loss of visual acuity and red-green color blindness); dose-related (25mgkd) hyperuricemia C/I: very young children because visual acuity assessment is difficult Pyrazinamide A relative of nicotinamide, stable, inexpensive Inhibits intracellular organism MOA: inhibits mycobacterial fatty acid synthase I involved in mycolic acid synthesis Resistance: mutations in pncA Kinetics: well absorbed; distributed widely, in inflammed meninges; t1/2 8-11 hrs. Clinical use: a. 25mgkd + INH + Rifampin x 6 mos. or 50-70mgkg 2x-3x weekly dosing b. multi-drug resistant cases PZA + Ciprofloxacin or Ofloxacin -prevention of active disease in close contacts and recent converters Adverse effects: a. hepatotoxicity (1-5%) b. nausea, vomiting c. drug fever d. hyperuricemia (gouty arthritis) Streptomycin Resistant to some non-tuberculous species Extracellular tubercle bacilli; inflammed meninges MOA: interfere with protein synthesis (30s subunit) Resistance: point mutation in rpsL gene or rrs that alters the ribosomal binding site Clinical use: a. severe, life threatening forms of TB b. drug resistance Dose: 15mgkd IM or IV x several weeks ffed. by 1-1.5gm. 2-3x weekly x 6 mos. Adverse reaction: ototoxicity, nephrotoxicity Alternative or Second Line Drugs •Uses: a. resistance b. failure of clinical response to conventional tx. c. toxic effects Ethionamide Related to INH; poorly soluble in water; liver MOA: blocks mycolic acid synthesis Dose: 1 gm/d – to achieve serum concentration of 20 ug/ml; CSF conc.; causes gastric irritation and neurologic symptom Adverse effect: hepatotoxic; neurotoxicity Dose: 250 mg OD → 500-750 mg OD Resistance: when used as single agent Capreomycin MOA: peptide protein synthesis inhibitor from Streptomyces capreolus Used for multidrug resistant cases (streptomycin, amikacin) Dose: 1 gm/d IM Resistance: rrs mutation Adverse effect: nephrotoxic, ototoxic - reduced if 1 gm is given 2-3x weekly after initial response is observed Cycloserine MOA: inhibitor of cell wall synthesis Dose: 0.5-1gm/d in 2 divided doses Renal excretion (dose is reduced if creatinine clearance is <50ml/min Adverse effect: a. peripheral neuropathy (seen in 1st 2 weeks of therapy) b. CNS dysfunction – depression, psychotic reactions (pyridoxine 150mg/d is given to ameliorate neurologic toxicity) Aminosalicylic Acid (PAS) MOA: folate synthesis antagonist Structure – similar to PABA and sulfonamides Widely distributed in tissues and body fluids except in CSF; excreted in urine Adverse effect: a. anorexia, nausea, lbm, epigastric pain b. peptic ulceration, hgge c. hypersensitivity reaction – fever, jt. pains, skin rashes, hepatosplenomegaly, hepatitis, adenopathy, granulocytopenia →seen 3-8 weeks of PAS Kanamycin and Amikacin MOA: inhibits 30s ribosomal subunit For streptomycin resistant cases, multidrug resistant TB, atypical mycobacterium Dose: 15 mgkd IV, IM + 1,2 or 3 other drugs x 2 mos. then 1-1.5 gm 2-3x weekly x 4 mos. Ciprofloxacin and Levofloxacin MOA: inhibits gyrase mediated DNA-supercoiling M. tuberculosis: levofloxacin > ciprofloxacin Atypical mycobacterium: levofloxacin < ciprofloxacin Dose: ciprofloxacin – 750 mg po BID/ levofloxacin – 500 mg po OD + 2 or more active drugs Prophylaxis: fluoroquinolone + PZA (multidrug resistant cases) Resistance: mutations in gyrase A subunit Rifabutin Derived from rifamycin, related to rifampin Uses: a. M. tb, M. avium intracellulare, M. foruitum b. disseminated atypical disease in AIDS pts. with CD4 count of <50/ml. c. prophylaxis: TB x 6 mos. alone or with PZA x 2 mos. Resistance: rpo mutation Less potent inducer – for HIV infected patients receiving other meds Dose: 300 mg/d if with protease inhibitor – 150 mg/d if with efavirenz – 450 mg/d Rifapentine Analog of rifampin; against M. tb, M. avium MOA: bacterial RNA polymerase inhibitor Potent inducer of cytochrome p450 Toxicity: Dose: 600 mg once or 2x weekly Clofazimine Last resort for multidrug resistant TB Effective against leprosy MOA: unknown ( involved in DNA binding) Adverse effect: skin discoloration, GIT intolerance Dose: 200 mg po as single or divided doses (t1/2 2 mos.- slowly released) Atypical Mycobacteria Not communicable from person to person Disease produced are less severe than TB MAC – disseminated disease in late stages of AIDS; incurable - 1st line tx: azithromycin 500 mg OD or clarithromycin 500 mg BID + ethambutol 15 mgkd or Clofazimine or Ciprofloxacin 750mg BID or Amikacin - 2nd line tx: Rifabutin 300 mg OD; Rifampicin; Ethionamide; Cycloserine; Imipenem - prophylaxis in AIDS pts.: Rifabutin 300 mg OD Mycobacterium marinarum - skin infections - 1st line tx: Rifampicin + Ethambutol - 2nd line tx: TMP-SMX; Clarithromycin; Amikacin; Kanamycin; Minocycline; Doxycycline Mycobacterium scrofulaceum - cervical lymphadenitis - tx: surgical excision Mycobacterium fortuitum - chronic lung disease and skin/soft tissue infection - 1st line tx: Amikacin + Doxycycline - 2nd line tx: Cefoxitin; Rifampicin; TMP-SMX; Ciprofloxacin; Ofloxacin; Imipenem; Clarithromycin Mycobacterium kansasii - similar to TB but milder - 1st line tx: INH + Rifampicin + Ethambutol - 2nd line tx: Ethionamide; Cycloserine; Clarithromycin; Amikacin; Streptomycin Leprosy Caused by M. leprae Tropical, warm temperate regions Skin and nerve predilection Depends upon cell-mediated immunity Dx: biopsy; slit skin smears Mode of transmission: nasal secretions Clinical types of Leprosy: 1. Tuberculoid leprosy – skin macules with clear centers and well defined margins; anesthetic; no Virchow cells; (+) lepromin test 2. Borderline tuberculoid 3. Borderline disease 4. Borderline lepromatous 5. Lepromatous – impaired cell immunity; atrophy of skin, muscles; amputations; spontaneous ulcerations Leprosy Dapsone (diaminodiphenylsulfone) MOA: inhibits folate synthesis Uses: a. leprosy b. prevent and treat P. carinii in AIDS Mgt: dapsone + rifampin + clofazimine (100mg OD) (600mg monthly) (100mg/d po) Adverse effect: hemolysis, GIT intolerance, erythema nodosum leprosum (steroids/thalidomide) Jarisch-Herxheimer reaction: - exacerbation of lepromatous leprosy - is induced 5-6 wks. after initiation of treatment - fever, malaise, exfoliative dermatitis, jaundice with hepatic necrosis, lymphadenopathy, methemoglobinemia, anemia Leprosy (cont.) Rifampicin – 600mg OD or once a month Clofazimine (Lamprene) MOA: inhibit the template function of DNA by binding to it -prevents the development of erythema nodosum leprosum - oral; 100mg OD - SE: discoloration of the skin, eosinophilic enteritis Miscellaneous agents for leprosy Thalidomide – treatment of erythema nodosum leprosum -dose: 100 – 300mg/day; teratogenic Ethionamide – a substitute for clofazimine -dose: 250 -375mg/day Management of Leprosy Tuberculoid, borderline tuberculoid and indeterminate disease: Dapsone 100 mg daily + Rifampicin 600 mg daily/monthly X 6 mos. Lepromatous, borderline lepromatous, borderline disease: Dapsone 100 mg daily + Rifampicin 60 mg daily/monthly +/Clofazimine 100 mg daily X 1–5 yrs. Leprosy-Classic Facial Appearance: Patient with chronic M Leprae infection that has led to collapse of nasal structure and subsequent development of classic "Leonine Facies.“ Skin discoloration is due to medication used to treat this infection. Patient has lost digits of hand secondary to leprosy as well. Thank you Ma. Victoria M. Villarica, M.D.