* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download LOCAL ANESTHETICS,IV SEDATION AND PAIN MANAGEMENT
Survey
Document related concepts
Drug interaction wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Neuropharmacology wikipedia , lookup
Effects of long-term benzodiazepine use wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Toxicodynamics wikipedia , lookup
Theralizumab wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
History of general anesthesia wikipedia , lookup
Psychopharmacology wikipedia , lookup
Transcript
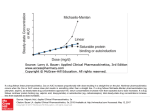
LOCAL ANESTHETICS,IV SEDATION AND PAIN MANAGEMENT MORAYA ALQAHTANI,MD Local Anesthetic history • • • • • • • • • Cocaine-1800 Niemann-1859 1884-1st use in clinical practice 1904-procaine 1925-dibucaine 1932-tetracaine 1942-Licocaine Mepivicaine,prilocaine,bupivicaine,etidocaine. ropivicaine neurophysiology Nerve structure pharmacokinetics • • • • Weak bases Lipid soluble Pka:8-9 at physiological pH Lipophilic portion-hydrophilic portion and intermediate link pharmacokinetics • • • • Degree of ionization. Both are involved in the blockage of the nerve They act by blocking Na channel Duration of esters are shorter pharmacokinetics • Vasoconstrictor activity at low doses • Vasodilatation at higher doses • Metabolism:Esters by plasma cholinesterase PAMA Amides metabolized in the liver pharmacokinetics • Vasoconstrictor activity at low doses • Vasodilatation at higher doses • Metabolism:Esters by plasma cholinesterase PAMA Amides metabolized in the liver pharmacokinetics • Clearance:amide mainly hepatic, • widely distributed compared to esters • More stable • Minimal allergic reaction Pharmacological factors • Lipid solubility • Absorption and distribution: • pharmacological factors • Physical factors:age,hepatic,renal,inflammation pharmacological factors *injection site *dosage *presence of epinephrine ,carbonation *protein binding *chemical properties Classification of LA Short acting Procaine 60-90 min Chloroprocaine 30-60 min Intermediate acting Mepivicaine Prilocaine 20-24 20-24 Long acting Lidocaine Tetracaine Bupivicaine 90-200 80-600 Etidocaine DRUG Maximum Plain(mg) Maximum Epinephrine(mg) Chloroprocaine 800 1000 Lidocaine 300 500 Mepivacaine 300 500 Prilocaine 500 600 Bupivacaine 175 225 Etidocaine 300 400 LA • Preparation: - topical :ointments,cream,lotion,spray -Injection • EMLA:Eutotic Mixture of Local Anesthetics 2.5% prilocaine 2.5% lidocaine TOXICITY Toxicity • Allergic reaction • Local toxicity • Systemic toxicity Allergic reaction • Rare condused with adverse effects • More with esters-PABA • Delayed type • No cross sensitivity • prevention: *proper Hx & PE *skin test- 20%-30% false positive Local toxicity • Direct trauma • Intraneuronal injection • Rare • preventable Systemic toxicity • CNS • CVS • Methemoglobinemia CVS • Conduction • Contractility • Peripheral effect • • • • CVS more resistant than CNS Bupivicaine more cardiac toxicity Ropivicaine less cardiac toxicity Lidocaine :anti arrhythmic drug CNS • • • • Concentration dependant Low concentration CNS:increases with hypoxia,acidosis ,pregnancy Adverse effect: drowsiness,light headiness slurred speech,restlessness, vertigo,tinnitus, muscle twitching, tremors,convulsion, coma, IV Sedation Practical consideration • Quite environment • Repeated cuff blood pressure measurement should be avoided • Monitors should be muted apart from alarm. Requirements of analgesia • 1.Continuous IV access. • 2.Continuous monitoring with both ECG and pulse oximeter. • 3.Both the practitioner and the assistant should have recently certified in CPR. • 4.Resuscitation equipments should be available (crash cart). • 5.Possibility to transfer for full critical care facilities e.g. Other hospital, ICU, OR. Steps to Sedoanalgesia • 1.Premedication with BDZ • 2.Adequate local or regional anesthesia • 3.IV sedation e.g. Midazolam • 4.Adjuvant analgesia with narcotics only if local/regional anesthetic is ineffective. IV Anesthetics • Neuroleptanesthesia • Neuroleptic drugs : Phenothiazines e.g. Chlorpromazine. • Butyrophenones e.g. Haloperidol, Droperidol. • Rarely used in anesthesia because of hypotension • droperidol –fentanyl (Innovar ) IV Anesthetics • Butyrophenones result in significant: • Sedation. • Tranquility. • Immobility • Antiemesis IV Anesthetics • Their side effects include: • An extrapyramidal syndrome with face and neck dyskinesia. • Oculogyric crises. • Torticollis. • Agitation • Hallucination IV Anesthetics • Droperidol (like other Butyrophenones) affect GABA receptors and alters the balance of dopamine and acetylcholine in certain brain sites. • Neuroleptanesthesia is contraindicated in patients receiving Mono Amine Oxidase Inhibitors, abusing drugs or alcohol and those with Parkinson’s disease. Benzodiazepines • Diazepam (valium) 1959 • Lorazepam (ativan) 1971 • Midazolam (versed) 1976 pharmacokinetics • Small molecule • Lipid soluble • Metabolized in the liver • Habitual use of alcohol • Lorazepam has higher affinity to receptors Benzodiazepines • • • • Action mediated through GABA Mainly on CNS ,minimal action on PNS Cells become hyperpolarized resistant to exitation Function is blood level dependant 20% :anxiolytic 30%-50% :sedation 60% :loss of consciousness • Tolerance Short acting Midazolam 6-11ml/kg/min Intermediate acting Lorazepam 0.8-1.8ml/kg/min Long acting Diazepam 0.2-0.5ml/kg/min Benzodiazepines • • • • • • Hypnotic Sedative Anxiolytic Amnestic Anticonvulsant:increases seizure threshold Muscle relaxant Benzodiazepines • Uses Sedation,Induction,maintainance • Contraindication: • Hypersensitivity, myasthenia gravis, COPD, acute narrow angle glaucoma. • Safety has not been established in children and pregnant females Benzodiazepines • Side effects *high safety margin *free allergic reaction *inactive non toxic metabolite *respiratory problem *venous irritation,thrombophlebitis *unpredictable interval of amnesia Rx: Flumazenil (Anexate) 0.2 mg IV over 15 sec. Then 0.1mg IV q60 sec. To effect (max. 1mg). Benzodiazepines • Dosage: midazolam: IM 0.07 mg/kg (5mg) 30 – 60 min.prior (50% of dose if >60 years) I.V. sedation: titrate with small doses (2mg initial followed by 1mg q2 min to effect) (max.dose 0.1mg/kg) (reduce dose by 30% if premedicated and by 50% if >60yo). • Diazepam (Valium ) : IM/PO premedication: 5-10 mg. 1 to 2 h prior (reduce dose by 50% if >60yo). • IV sedation: 5 - 10 mg IV q3h. (Reduce by 50% if >60yo). • Lorazepam (ativan): PO/SL premedication: 50mcg/kg (maximum 4mg) 1-2 hour prior (50% of dose if more than 60 yo) OPOIDS Classification • Natural • Semisynthetics • synthetics Natural opoids • Morphine • Codeine • Papaverine Semisynthetic • Heroin -dihydromorphone Synthetic opoids • Levorphenols: -Methadone -pentazocine • Phenypiperidine -meperidine -fentanyl opoids • Inhibit the action of opoid neurotransmitters • Analgesic effect differences: -access to the receptor -binding affinity -lipophility,ionization -distribution,clearance OPOIDS • In general most of them *respiratory depression *bradycardia except demerol *anti tussive *sleep *nausea,vomiting,constipation *hypersensitivity • Overdose :naloxone 0.4 mg IV q 2min opoids • Morphine: • Pharmacology: Onset of action 2 to 5 min. Duration of action 4-5 hrs. • Indication:Analgesia, induction of anesthesia. • Contraindication: • Hypersensitivity, MAO inhibitors within 14 days (hpertensive crises, tachyarrethmias). Dosage: 0.1-0.2 mg/kg IV/IM/SC q3h. opoids • Hydromorphone : -7-8 times stronger than morphine -rapid distribution -good in renal failure patient -dose:2-4 mg po Demerol • Pharmacology: Onset of action 2 to 5 min. via IV duration of action 2-4 hrs. • absorbed slowly • 7 to 10 times less potent than morphine • 60% bound to protien • Dosage:up to 1.8 mg/kg IM/SC/IV q2h. Fentanyl • Demorol family -100x morphine • High lipid solubility • Metabolized in the liver , excreted by bile or kidney • Poor hypnotic and sedative activity at low doses • No histamine release katamine • Cataleptic, analgesic, and dissociative anesthetic agent. • Onset of action 30 sec. For IV ,12-25 min for IM dosing. • Dosage:induction 2.0 mg/kg IV over 60 sec or 10 mg/kg IM (adults and children). • Maintenance of anesthesia: 50% of induction dose IV or IM, as anesthesia is lost. katamine • Contraindication:Hypersensitivity, pregnancy,uncontrolled HTN • Adverse effect:HR,BP,RR, pleasant dreams 5%, unpleasant dreams 2%, hallucinations 1%, confusion 3% (give BDZ with it to prevent bad trips). Other IV anesthetics propofol • • • • • Most resent 1977 High lipid solubility Alkylphenols Viscous milky white substance 1% of propofol *1%soy bean oil *2.25% glycerol *1.2% pure egg Propofol • • • • • Metabolized in the liver Iactive metabolite ,98% protein bound Hypnotic,analgesic,induction Titratable level of sedation Dose: sedation 10-50 micgm/kg/min induction 0.1-1 mg/kg over 3 min • Side effects:respiratory depression PAIN MANAGEMENT • Definition • Effect of pain -Neuroendocrine system -CVS -Resp -GIT -GUT -immunity NSAIDs • Limited use for acute PO pain • Mechanism of action • Prostaglandins -fever ,pain,vasodilatation Classification Mechanism of action pharmacokinetics • Rapidly absorped • Metabolized in the liver,inactive metabolites • High protein bound • Action dose dependent Side effects • Gastropathy • Hemostasis • nephrotoxocity Ketorolactromethaminne (Toradol) • Pyrolle acetic acid • High analgesic potency • 2mg of toradol = 1mg og morphine = 6-10mg of demerol • Dose 60mg IM followed by 30 mg IM q 6h • 50% in renal problem Toradol • Most sufficient for sever pain • 0.3% incidence of PU • Bleeding with long term use • Increases bleeding time Nausea and Vomiting • • • • • • • History of PO emesis Female Obesity Pain Type of surgery Anesthetic drugs Gastric distension Treatment • Prophylactic antiemetic droperidol 10 to 20 micgm/kg • Ondansetron 4 to 8 mg IV • Metoclopramide (10 to 20 mg IV) • Transdermal scopolamine