* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Lecture 8 - Mammography and tomosynthesis
Survey
Document related concepts
Transcript
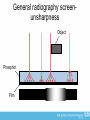
FRCR: Physics Lectures Diagnostic Radiology Lecture 8 Mammography and tomosynthesis Dr Tim Wood Clinical Scientist Overview • Introduction to mammography • The mammography X-ray set • The physics of mammography – X-ray spectra for mammo • Film/screen vs digital mammography • The NHS Breast Screening programme • Tomosynthesis An introduction to mammography • The aims of mammography are: – Demonstrate microcalcifications – features with high inherent contrast, but 100 μm or less in diameter – Demonstrate low contrast masses within the breast tissue – these may be relatively large, but are often very low contrast as glandular and adipose tissue have very similar atomic number (7.4 and 6.5, respectively) • Hence, require good spatial and contrast resolution • Also used for screening so must be lowest dose possible (more on this later) • Presents a different technical challenge compared with everything discussed so far An introduction to mammography The mammography X-ray set • Highly specialised X-ray systems required for mammography • Older sets based on a film-screen system • Modern sets utilise flat panels (typically direct conversion) • Sectra (now Philips) MicroDose uses a scanning fan beam geometry (see later) The mammo unit • Cathode-anode axis is perpendicular to chest wall (CW) – Cathode is positioned at the CW • Fall off in intensity due to anode-heel effect is at the nipple edge (NE) – More tissue at the CW, so requires more intense X-ray beam – NE tends to be thinner due to shape of anatomy (despite compression) so requires less Farr’s Physics for Medical Imaging 2nd Edition The mammo unit • Focal spot is located directly above the CW edge • Dual focus tubes are used – ~0.4 mm for general mammo – ~0.1-0.15 mm for magnification • Due to small focal spots, tube current tends to be limited to ~100 mA – Avoid melting the anode • kVp tends to be in the range 24-35 kV – Maximise radiographic contrast Farr’s Physics for Medical Imaging 2nd Edition The mammo unit • Breast is positioned on the support platform • Compression is applied to; – Hold the breast still during exposure (exposure times can be quite long due to low mA) – reduce motion unsharpness – Reduce the thickness of tissue so lower exposure factors can be used (lower dose) – Spread the anatomy out to minimise overlaying structures (improve contrast) Farr’s Physics for Medical Imaging 2nd Edition The mammo unit • Compression is applied to; – Equalise thickness to ensure homogenous density on the radiograph – Bring the structures closer to the detector to reduce geometric unshaprness Farr’s Physics for Medical Imaging 2nd Edition The mammo unit • A moving anti-scatter grid is incorporated in the support platform (bucky) to improve image contrast • AEC detectors on film-screen systems are positioned behind the film cassette (as opposed to in front, like in general radiography), as they will be seen on the resulting image due to the low kV used Farr’s Physics for Medical Imaging 2nd Edition Figure 1. Typical process of x-ray mammography. Mahesh M Radiographics 2004;24:1747-1760 ©2004 by Radiological Society of North America The mammo unit • The film/screen AEC chamber position can be moved to accommodate different sized women – Slides back and forth along the central axis • Digital systems use the signal incident on the detector as the AEC, and can use quite complex algorithms to determine the region of the image to use Farr’s Physics for Medical Imaging 2nd Edition The X-ray tube • In mammography, to maximise contrast use the lowest kV possible • Typical compressed breast thickness is 40-50 mm, and rarely greater than 80 mm • Ideal mono-energetic X-ray beam would be 1622 keV • Hence, the use of the full range of the Bremsstrahlung spectrum from a tungsten target with aluminium filters is not ideal for mammo • Use a range of different combinations of target and filter for different breast thicknesses and/or detectors The mammography X-ray spectrum • Traditional film-screen mammography relies on the spectrum from a Molybdenum (Mo) target with a Mo filter for small to average sized breast (up to about 50-60 mm) • Alternative filters such as Rhodium (Rh) can be used for thicker breasts, and some (but not many) systems use a Rh target as well • Tungsten targets are also used for thicker breasts, but in conjunction with the Rh filter (not Al like general radiography) • W/Rh is also primary target filter combination in digital systems (plus some other filters such as silver and very thin aluminium) The mammography X-ray spectrum • So why use these combinations for mammography?... • Mo – K-edge at 20 keV – Characteristic X-rays at 17.4 and 19.6 keV • Rh – K-edge at 23.2 keV – Characteristic X-rays at 20.2 and 22.8 keV K-edge (revision) 20 keV Mo/Mo Spectrum Intensity Mo target - unfiltered 2.15E+05 2.10E+05 2.05E+05 2.00E+05 1.95E+05 1.90E+05 1.85E+05 1.80E+05 1.75E+05 1.70E+05 1.65E+05 1.60E+05 1.55E+05 1.50E+05 1.45E+05 1.40E+05 1.35E+05 1.30E+05 1.25E+05 1.20E+05 1.15E+05 1.10E+05 1.05E+05 1.00E+05 9.50E+04 9.00E+04 8.50E+04 8.00E+04 7.50E+04 7.00E+04 6.50E+04 6.00E+04 5.50E+04 5.00E+04 4.50E+04 4.00E+04 3.50E+04 3.00E+04 2.50E+04 2.00E+04 1.50E+04 1.00E+04 5.00E+03 0.00E+00 Mo no filter 0 5 10 15 kV 20 25 30 Intensity Mo target – Mo filter 2.15E+05 2.10E+05 2.05E+05 2.00E+05 1.95E+05 1.90E+05 1.85E+05 1.80E+05 1.75E+05 1.70E+05 1.65E+05 1.60E+05 1.55E+05 1.50E+05 1.45E+05 1.40E+05 1.35E+05 1.30E+05 1.25E+05 1.20E+05 1.15E+05 1.10E+05 1.05E+05 1.00E+05 9.50E+04 9.00E+04 8.50E+04 8.00E+04 7.50E+04 7.00E+04 6.50E+04 6.00E+04 5.50E+04 5.00E+04 4.50E+04 4.00E+04 3.50E+04 3.00E+04 2.50E+04 2.00E+04 1.50E+04 1.00E+04 5.00E+03 0.00E+00 ‘Soft’ X-rays absorbed by filter (as for general X-ray set) Mo no filter Mo/Mo K-edge at 20 keV absorbs most of ‘hard’ Xrays 0 5 10 15 kV 20 25 30 Mo/Rh Spectrum Intensity Mo target - unfiltered 2.15E+05 2.10E+05 2.05E+05 2.00E+05 1.95E+05 1.90E+05 1.85E+05 1.80E+05 1.75E+05 1.70E+05 1.65E+05 1.60E+05 1.55E+05 1.50E+05 1.45E+05 1.40E+05 1.35E+05 1.30E+05 1.25E+05 1.20E+05 1.15E+05 1.10E+05 1.05E+05 1.00E+05 9.50E+04 9.00E+04 8.50E+04 8.00E+04 7.50E+04 7.00E+04 6.50E+04 6.00E+04 5.50E+04 5.00E+04 4.50E+04 4.00E+04 3.50E+04 3.00E+04 2.50E+04 2.00E+04 1.50E+04 1.00E+04 5.00E+03 0.00E+00 Mo no filter 0 5 10 15 kV 20 25 30 Intensity Mo target – Rh filter 2.15E+05 2.10E+05 2.05E+05 2.00E+05 1.95E+05 1.90E+05 1.85E+05 1.80E+05 1.75E+05 1.70E+05 1.65E+05 1.60E+05 1.55E+05 1.50E+05 1.45E+05 1.40E+05 1.35E+05 1.30E+05 1.25E+05 1.20E+05 1.15E+05 1.10E+05 1.05E+05 1.00E+05 9.50E+04 9.00E+04 8.50E+04 8.00E+04 7.50E+04 7.00E+04 6.50E+04 6.00E+04 5.50E+04 5.00E+04 4.50E+04 4.00E+04 3.50E+04 3.00E+04 2.50E+04 2.00E+04 1.50E+04 1.00E+04 5.00E+03 0.00E+00 Mo no filter Mo/Rh K-edge at 23.2 keV absorbs less of the ‘hard X-rays’ than Mo filter – hence, higher mean energy 0 5 10 15 kV 20 25 30 Intensity Mo target – both filters 2.15E+05 2.10E+05 2.05E+05 2.00E+05 1.95E+05 1.90E+05 1.85E+05 1.80E+05 1.75E+05 1.70E+05 1.65E+05 1.60E+05 1.55E+05 1.50E+05 1.45E+05 1.40E+05 1.35E+05 1.30E+05 1.25E+05 1.20E+05 1.15E+05 1.10E+05 1.05E+05 1.00E+05 9.50E+04 9.00E+04 8.50E+04 8.00E+04 7.50E+04 7.00E+04 6.50E+04 6.00E+04 5.50E+04 5.00E+04 4.50E+04 4.00E+04 3.50E+04 3.00E+04 2.50E+04 2.00E+04 1.50E+04 1.00E+04 5.00E+03 0.00E+00 Mo no filter Mo/Mo Mo/Rh 0 5 10 15 kV 20 25 30 Mammography X-ray spectra • Traditionally, mammography relies on the characteristic X-rays and K-edges of target/filter materials to produce a low energy spectrum around the ideal 16-22 keV • Thicker breasts, however, require more penetrating beams, so W or Rh target may be used • Result in higher mean energy of X-ray beam • For thinner to thicker breasts, systems tend to use: – Mo/Mo then Mo/Rh then Rh/Rh or W/Rh Rh/Rh Spectrum Rh target – unfiltered Intensity 8.50E+04 8.00E+04 7.50E+04 Rh no filter 7.00E+04 6.50E+04 6.00E+04 5.50E+04 5.00E+04 4.50E+04 4.00E+04 3.50E+04 3.00E+04 2.50E+04 2.00E+04 1.50E+04 1.00E+04 5.00E+03 0.00E+00 0 5 10 15 kV 20 25 30 Rh target – Rh filter 5.00E+04 4.50E+04 Rh/Rh 4.00E+04 Intensity 3.50E+04 3.00E+04 2.50E+04 2.00E+04 1.50E+04 1.00E+04 5.00E+03 0.00E+00 0 5 10 15 kV 20 25 30 Rh target – Rh filter 8.50E+04 8.00E+04 Rh no filter Rh/Rh 7.50E+04 7.00E+04 Intensity 6.50E+04 6.00E+04 5.50E+04 5.00E+04 4.50E+04 4.00E+04 3.50E+04 3.00E+04 2.50E+04 2.00E+04 1.50E+04 1.00E+04 5.00E+03 0.00E+00 0 5 10 15 kV 20 25 30 Intensity W target 1.08E+06 1.07E+06 1.06E+06 1.05E+06 1.04E+06 1.03E+06 1.02E+06 1.01E+06 1.00E+06 9.95E+05 9.90E+05 9.85E+05 9.80E+05 9.75E+05 9.70E+05 9.65E+05 9.60E+05 9.55E+05 9.50E+05 9.45E+05 9.40E+05 9.35E+05 9.30E+05 9.25E+05 9.20E+05 9.15E+05 9.10E+05 9.05E+05 9.00E+05 8.95E+05 8.90E+05 8.85E+05 8.80E+05 8.75E+05 8.70E+05 8.65E+05 8.60E+05 8.55E+05 8.50E+05 8.45E+05 8.40E+05 8.35E+05 8.30E+05 8.25E+05 8.20E+05 8.15E+05 8.10E+05 8.05E+05 8.00E+05 7.95E+05 7.90E+05 7.85E+05 7.80E+05 7.75E+05 7.70E+05 7.65E+05 7.60E+05 7.55E+05 7.50E+05 7.45E+05 7.40E+05 7.35E+05 7.30E+05 7.25E+05 7.20E+05 7.15E+05 7.10E+05 7.05E+05 7.00E+05 6.95E+05 6.90E+05 6.85E+05 6.80E+05 6.75E+05 6.70E+05 6.65E+05 6.60E+05 6.55E+05 6.50E+05 6.45E+05 6.40E+05 6.35E+05 6.30E+05 6.25E+05 6.20E+05 6.15E+05 6.10E+05 6.05E+05 6.00E+05 5.95E+05 5.90E+05 5.85E+05 5.80E+05 5.75E+05 5.70E+05 5.65E+05 5.60E+05 5.55E+05 5.50E+05 5.45E+05 5.40E+05 5.35E+05 5.30E+05 5.25E+05 5.20E+05 5.15E+05 5.10E+05 5.05E+05 5.00E+05 4.95E+05 4.90E+05 4.85E+05 4.80E+05 4.75E+05 4.70E+05 4.65E+05 4.60E+05 4.55E+05 4.50E+05 4.45E+05 4.40E+05 4.35E+05 4.30E+05 4.25E+05 4.20E+05 4.15E+05 4.10E+05 4.05E+05 4.00E+05 3.95E+05 3.90E+05 3.85E+05 3.80E+05 3.75E+05 3.70E+05 3.65E+05 3.60E+05 3.55E+05 3.50E+05 3.45E+05 3.40E+05 3.35E+05 3.30E+05 3.25E+05 3.20E+05 3.15E+05 3.10E+05 3.05E+05 3.00E+05 2.95E+05 2.90E+05 2.85E+05 2.80E+05 2.75E+05 2.70E+05 2.65E+05 2.60E+05 2.55E+05 2.50E+05 2.45E+05 2.40E+05 2.35E+05 2.30E+05 2.25E+05 2.20E+05 2.15E+05 2.10E+05 2.05E+05 2.00E+05 1.95E+05 1.90E+05 1.85E+05 1.80E+05 1.75E+05 1.70E+05 1.65E+05 1.60E+05 1.55E+05 1.50E+05 1.45E+05 1.40E+05 1.35E+05 1.30E+05 1.25E+05 1.20E+05 1.15E+05 1.10E+05 1.05E+05 1.00E+05 9.50E+04 9.00E+04 8.50E+04 8.00E+04 7.50E+04 7.00E+04 6.50E+04 6.00E+04 5.50E+04 5.00E+04 4.50E+04 4.00E+04 3.50E+04 3.00E+04 2.50E+04 2.00E+04 1.50E+04 1.00E+04 5.00E+03 0.00E+00 W no filter 0 5 10 15 kV 20 25 30 W target – Rh filter 1.50E+04 Intensity W/Rh 1.00E+04 5.00E+03 0.00E+00 0 5 10 15 kV 20 25 30 Intensity W target – Rh filter 1.08E+06 1.07E+06 1.06E+06 1.05E+06 1.04E+06 1.03E+06 1.02E+06 1.01E+06 1.00E+06 9.95E+05 9.90E+05 9.85E+05 9.80E+05 9.75E+05 9.70E+05 9.65E+05 9.60E+05 9.55E+05 9.50E+05 9.45E+05 9.40E+05 9.35E+05 9.30E+05 9.25E+05 9.20E+05 9.15E+05 9.10E+05 9.05E+05 9.00E+05 8.95E+05 8.90E+05 8.85E+05 8.80E+05 8.75E+05 8.70E+05 8.65E+05 8.60E+05 8.55E+05 8.50E+05 8.45E+05 8.40E+05 8.35E+05 8.30E+05 8.25E+05 8.20E+05 8.15E+05 8.10E+05 8.05E+05 8.00E+05 7.95E+05 7.90E+05 7.85E+05 7.80E+05 7.75E+05 7.70E+05 7.65E+05 7.60E+05 7.55E+05 7.50E+05 7.45E+05 7.40E+05 7.35E+05 7.30E+05 7.25E+05 7.20E+05 7.15E+05 7.10E+05 7.05E+05 7.00E+05 6.95E+05 6.90E+05 6.85E+05 6.80E+05 6.75E+05 6.70E+05 6.65E+05 6.60E+05 6.55E+05 6.50E+05 6.45E+05 6.40E+05 6.35E+05 6.30E+05 6.25E+05 6.20E+05 6.15E+05 6.10E+05 6.05E+05 6.00E+05 5.95E+05 5.90E+05 5.85E+05 5.80E+05 5.75E+05 5.70E+05 5.65E+05 5.60E+05 5.55E+05 5.50E+05 5.45E+05 5.40E+05 5.35E+05 5.30E+05 5.25E+05 5.20E+05 5.15E+05 5.10E+05 5.05E+05 5.00E+05 4.95E+05 4.90E+05 4.85E+05 4.80E+05 4.75E+05 4.70E+05 4.65E+05 4.60E+05 4.55E+05 4.50E+05 4.45E+05 4.40E+05 4.35E+05 4.30E+05 4.25E+05 4.20E+05 4.15E+05 4.10E+05 4.05E+05 4.00E+05 3.95E+05 3.90E+05 3.85E+05 3.80E+05 3.75E+05 3.70E+05 3.65E+05 3.60E+05 3.55E+05 3.50E+05 3.45E+05 3.40E+05 3.35E+05 3.30E+05 3.25E+05 3.20E+05 3.15E+05 3.10E+05 3.05E+05 3.00E+05 2.95E+05 2.90E+05 2.85E+05 2.80E+05 2.75E+05 2.70E+05 2.65E+05 2.60E+05 2.55E+05 2.50E+05 2.45E+05 2.40E+05 2.35E+05 2.30E+05 2.25E+05 2.20E+05 2.15E+05 2.10E+05 2.05E+05 2.00E+05 1.95E+05 1.90E+05 1.85E+05 1.80E+05 1.75E+05 1.70E+05 1.65E+05 1.60E+05 1.55E+05 1.50E+05 1.45E+05 1.40E+05 1.35E+05 1.30E+05 1.25E+05 1.20E+05 1.15E+05 1.10E+05 1.05E+05 1.00E+05 9.50E+04 9.00E+04 8.50E+04 8.00E+04 7.50E+04 7.00E+04 6.50E+04 6.00E+04 5.50E+04 5.00E+04 4.50E+04 4.00E+04 3.50E+04 3.00E+04 2.50E+04 2.00E+04 1.50E+04 1.00E+04 5.00E+03 0.00E+00 W no filter W/Rh 0 5 10 15 kV 20 25 30 Mammography X-ray spectra • Digital mammography tends to use W/Rh combination as digital gives much better contrast than the fixed dynamic range of film – Hence, the poorer contrast due to the harder X-ray beam is less significant than the gain due to the use of digital (window and level, image processing, etc) – Allows lower doses to be used for the same image quality – In practice, contrast resolution in digital is much better than film Film-screen • Film-screen mammography requires high spatial resolution – As using lower kV, thinner screens may be used to improve resolution – Single screen and emulsion layer to minimise crossover and parallax Film-screen • The screen is positioned on the distal side of the film – Hence, highest proportion of photon interactions will be on the side of the screen in contact with the film – This minimises the spread of light from the screen to the film • Film-screen mammo system is capable of ~15 lp mm-1 or better – Compared with ~7 lp mm-1 for general radiography General radiography screenunsharpness Object Phosphor Film Mammography screenunsharpness Object Film Phosphor Film-screen • Film-screen system is still limited by the fixed dynamic range of film • High contrast (gamma) films are used • Critical to ensure exposure factors are matched to the film – AEC setup and QA very important Figure 3. Limitations of SFM in imaging a breast composed of a wide range of tissues. Mahesh M Radiographics 2004;24:1747-1760 ©2004 by Radiological Society of North America The automatic exposure control • AECs are implemented in different ways by different manufacturers – Manual selection of kV and T/F based on exposure chart – Automatic select everything based on breast thickness and/or pre-pulse of X-rays Film-screen versus digital • The advantaged and limitations of the filmscreen system: Figure 2. Typical response curves for SFM and digital mammography. Mahesh M Radiographics 2004;24:1747-1760 ©2004 by Radiological Society of North America Film-screen versus digital • Digital mammography tends to use direct conversion flat panel detectors – Better spatial resolution than indirect detectors, but still limited to ~7-10 lp mm-1 – Hence, limiting spatial resolution is poorer c.f. film • BUT, image processing and window/level controls result in better contrast resolution • Lower dose as more efficient (better DQE) and higher beam qualities used • Higher throughput as instant image on screen – Particularly valuable on ‘vans’ • Plus all the other advantages of digital (and disadvantages, such as cost!) Digital Mammography • Directly acquire the data in digital format • Main technologies: HKD2 (Room 2) HKD1 (Centenary) – Phosphor coupled to a read out device – Indirect conversion flat panels – a-Se/TFT array – Direct conversion flat panels – Photon counting scanning detector HSU (Health Central), HKD3 (Room 3), HKD4 (Cromwell Road), HMU1-3, HGA1 & 2 (Grimsby) Direct conversion flat panels • Amorphous Selenium (a-Se) is a photoconductor – Converts X-rays directly to electrons • Deposited directly onto amorphous silicon TFT array • No phosphor, hence no light spread • Resolution governed by effective pixel pitch • Every mammography set manufacturer (except GE) use this technology MicroDose ‘photon counting’ • Photon counting detector = no electronic noise or analogue-to-digital conversion • Uses a scanning fan beam rather than a full field digital flat panel • Hence, much less scatter is generated in the breast – Do not need a moving anti-scatter grid, – Improves image quality, and/or – Reduces patient dose • Doses tend to be lower for this type of system than flat panel sets (~50%!) • BUT, the tubes are worked much harder The MicroDose system The output from ‘Collimator 1’ Photon counting • Detector counts photons as they hit the detector • Large number of crystalline Si strips in edge-on geometry (ensure long enough to absorb X-rays) • X-ray interactions excite electron-hole pairs (several thousand) • Bias voltage applied to induce current • Fast read-out electronics to count the pulses (2 ms) Photon counting Photon counting • Flat panels = integrating systems – Sum the electrical charge from all X-ray photon interactions – High energy photon = more electrical signal = greater weighting in the image = poorer contrast • Photon counting – – – – – High energy = larger pulse Low energy = smaller pulse Can separate ‘high’ and ‘low’ energy photons Can apply equal weighting to improve contrast Opens up the possibility of dual energy mammography (next version of MicroDose has this functionality, with glandularity calculation as standard) Patient dose • Patient dose optimisation particularly important in mammography (see later) • Systems designed to only expose the breast • Hence, effective dose is not a particularly useful quantity • The mean glandular dose (in mGy) is used instead – Typical values fall in the range 1.5-3 mGy per film – In the UK, the dose to the standard breast (4.5 cm Perspex, equivalent to 5.3 cm breast) must be less than 2.5 mGy – Doses in digital will be much lower than this – 2 mGy ~ 1 in 50,000 risk of fatal cancer (age 50-65) Magnification • Sometimes referred to as macroradiography • Mammo only modality that routinely uses magnification views • Use a raised platform to support the breast about half way between focus and film i.e. not in close(ish) contact anymore • Magnification is the result of the diverging X-ray beams travelling in straight lines Magnification imaging • Magnifies image by a factor of between 1.5-1.8 • Magnification increases geometric unsharpness so small focal spot is used Focal spot – Increases exposure times due to lower mA Object • Can remove grid to lower exposure factors (and patient dose) as scatter is reduced by the air gap • Overall patient dose is higher – Magnification requires individual justification Film/ detector Penumbra The NHS Breast Screening Programme • Based on the Forrest Report (1986), the first breast screening programme in the world was setup in England in 1988 • All women in the age range 50-70 invited every 3 years for mammogram – Two views of each breast – Age range recently extend to between late 40s-73 • However, the fundamental principle of screening programme means that healthy women are exposed to radiation – What about justification? Justification of the NHSBSP • The vast majority of women X-rayed in the NHSBSP show no signs of cancer, and have no symptoms prior to attending – Women who display symptoms should go to their GP and be referred to the symptomatic unit at their local hospital (outside the scope of the NHSBSP, but in Hull these are the same) • On an individual basis, justification is difficult • Justification for the NHSBSP is based on the net benefit to the population, not the individual • However, this makes patient dose optmisation and quality assurance (QA) critical to effectiveness of the programme – QA also important due to the basic principles of mammography e.g. low kV, high spatial resolution, etc QA and the NHSBSP • QA is a fundamental principle of the Breast Screening Programme • You are X-raying ‘healthy’ women, with no symptoms, so the JUSTIFICATION for the exposure (under IR(ME)R) is based on the net benefit to the population (rather than each individual), versus the risk of irradiating a large number of healthy women – This is a very current issue, given the recent publications about risk-benefit and overdiagnosis in the NHSBSP… • OPTIMISATION (under IR(ME)R) to ensure doses are ALARP is therefore incredibly important, so must make sure the X-ray equipment is fit for use! The NHSBSP and QA • The national NHSBSP is split into localities (e.g. Humberside BSP) that then belong to regions (e.g. North East, Yorkshire and Humberside) • Quality Assurance Reference Centres (QARCs) are regional bodies that ensure the local BSP is fulfilling their obligations under national guidance for the NHSBSP • Inspect whole of local BSP (including surgery, etc) • For mammography, there are national guidance documents outlining the QA required, split into daily, weekly and monthly Radiographer tests and 6 monthly Physics QA Physics QA • Test/measure (6 monthly): – – – – – – – – – – – kV accuracy X-ray tube output for all T/F and range of kV/mAs Half-value layers AEC performance Mean glandular dose to the standard breast Image quality with phantoms Beam alignments Uniformity Focal spot sizes Compression force Etc… Radiographer QA… • Daily – AEC consistency (B1) – Visual check of acquisition and reporting monitors (B2) – Inspection of breast support table and associated equipment (B3) • Weekly – Contrast-to-noise ratio (CNR) (B5) – Image quality (B6) – Artefacts and uniformity (B7) • Monthly – – – – Image quality (B6) AEC consistency with varying thickness including CNR (B10) Mechanical safety and beam function (B11) Compression force (B12) • Other (weekly/before use) – Stereo-tactic localising device (B8) The QARC website Tomosynthesis • Digital tomosynthesis can be considered a halfway house between tomography and CT • There are applications (and systems available) in general radiography, but most common implementation is in digital mammography • The basic principle is that a number of projections are acquired over a narrow range of angles, and the images are processed to give a series of ‘planes’ through the breast (strictly speaking they are not slices like in CT) Tomosynthesis equipment Tomosynthesis • Wider angle of projections = better 3D resolution • More projections = slower to acquire • Data processing is manufacturer specific; – Back projection/shift and add for Hologic (see Ben Johnson slides from UKMPG 2011) – Filtered back projection (like CT) for Siemens – Iterative reconstruction for IMS (like new CTs) Ben Johnson, Barts and the London NHS Trust, UKMPG 2011 Ben Johnson, Barts and the London NHS Trust, UKMPG 2011 Ben Johnson, Barts and the London NHS Trust, UKMPG 2011 Ben Johnson, Barts and the London NHS Trust, UKMPG 2011 Ben Johnson, Barts and the London NHS Trust, UKMPG 2011 Ben Johnson, Barts and the London NHS Trust, UKMPG 2011 Tomosynthesis • Like tomography, the basic idea is that in plane structures are in focus, out of plane structures blurred • Unlike tomography, reconstruct a number of different projections to get a series of images through the volume (like CT)