* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Coagulation
Neuropsychopharmacology wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Psychopharmacology wikipedia , lookup
Plateau principle wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
Metalloprotease inhibitor wikipedia , lookup
Drug-eluting stent wikipedia , lookup
Discovery and development of direct Xa inhibitors wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Dydrogesterone wikipedia , lookup
Discovery and development of direct thrombin inhibitors wikipedia , lookup
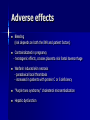
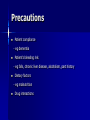
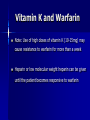
Blood coagulation and fibrinolysis March 2006 Haemostasis adhesion shape change activation and secretion aggregation interaction with coagulation factors Drug classes 1. Anticoagulants 2. Antiplatelet drugs 3. Thrombolytic Agents Anticoagulants Heparin Glycosaminoglycan containing a mixture of sulfated mucopolysaccharides of various sizes - Unfractionated (5000-30000 Da) - Low molecular weight (LMWH) (1000-10000 Da) Mechanism of Action Heparin : - enhances the action of Antithrombin III (AT-III) (plasma protease inhibitor) 1000 fold ↑ activity - antithrombin III inhibits clotting factor proteases, Thrombin (IIa), IXa, Xa, XIa and XIIa, by forming stable complexes - heparin binds to AT-III and causes a conformational change thereby activating AT-III LMWH: - predominantly inhibit factor Xa Heparins do not affect thrombin bound to fibrin or Xa bound to platelets Monitoring Therapy APTT (APTTR) (Activated Partial Thromboplastin Time) Intrinsic pathway (heparin) PT (INR) (Prothrombin Time) Extrinsic pathway (warfarin) Heparin - indications Rapid onset of action & short half life When immediate anticoagulation required When quick reversal may be required Prevention and treatment of venous thrombosis Pulmonary embolism Acute Coronary syndromes Given intravenously or subcutaneously Can be used in pregnant women Adverse effects Increased bleeding 3% - antidote (protamine sulfate) Heparin induced thrombocytopaenia - HITs 1% up to 3 days 5% >5 days - Can precipitate thrombosis Osteoporosis with long term high-dose administration 3-6mths Inhibit aldosterone synthesis – rarely causes ↑K+ Unfractionated heparin Unpredictable pharmacokinetics Requires regular monitoring Infusion Higher incidence of HITs Rebound ischaemia Low Mol Weight Heparins Eg Enoxaparin; Tinzaparin More predictable pharmacokinetics Lower incidence of heparin-associated thrombocytopenia Ease of administration s/c injection No need for monitoring Possible improvement in outcomes of acute coronary syndromes (Such a benefit was suggested with enoxaparin in TIMI 11B, ESSENCE, and EVET) Oral Anticoagulants Sweet Clover Coumarins Warfarin, Dicumarol Mechanism of action: Block the Vitamin K-dependent glutamate carboxylation of precursor clotting factors II, VII, IX and X Also inhibits Proteins C & S 8-12 hour delay in action because of T1/2 of clotting factors in plasma recovery needs synthesis of new clotting factors action is reversed with vitamin K Monitoring Therapy PT (INR) (Prothrombin Time) Extrinsic pathway (warfarin) APTT (APTTR) (Activated Partial Thromboplastin Time) Intrinsic pathway (heparin) Warfarin Highly plasma protein bound Metabolised by liver Substrate of CYP450 enzymes CYP1A2 (minor), 2C8/9 (major), 2C19 (minor), 3A4 (minor); Inhibits CYP2C8/9 (moderate), 2C19 (weak) Excreted in urine and stool Indications Prophylaxis and treatment of 1. venous thrombosis 2. pulmonary embolism 3. thromboembolic disorders 4. atrial fibrillation with risk of embolism 5. prophylaxis of systemic embolism post MI (LV thrombus) Adverse effects Bleeding (risk depends on both the INR and patient factors) Contraindicated in pregnancy - teratogenic effects, crosses placenta risk foetal haemorrhage Warfarin induced skin necrosis - paradoxical local thrombosis - increased in patients with protein C or S deficiency "Purple toes syndrome," cholesterol microembolization Hepatic dysfunction Precautions Patient compliance - eg dementia Patient’s bleeding risk - eg falls, chronic liver disease, alcoholism, past history Dietary factors - eg malnutrition Drug interactions Interactions Pharmacokinetic - changes in the absorption, protein binding, and/or metabolism - metabolism/elimination via cytochrome P450 system (common) - displacement of warfarin from plasma protein-binding sites eg NSAIDs (less important) Pharmacodynamic - alter the risk of bleeding or clotting by either effect on platelet aggregation or vitamin K catabolism CYP450 and Warfarin CYP2C8/9 inducers ↓ warfarin effect eg Carbamazepine, phenobarbital, phenytoin, rifampin CYP2C8/9 inhibitors ↑ warfarin effect eg fluconazole, gemfibrozil, ibuprofen, ketoconazole, mefenamic acid, miconazole, nicardipine, pioglitazone, amiodarone, isoniazid, losartan, omeprazole, pantoprazole CYP2C8/9 gene polymorphism Alcohol and Warfarin Acute ethanol ingestion (binge drinking) decreases the metabolism of warfarin and increases PT/INR Chronic daily ethanol use increases the metabolism of warfarin and decreases PT/INR Food and Warfarin The anticoagulant effects of warfarin may be decreased if taken with foods rich in vitamin K eg liver, green tea and leafy green vegetables Vitamin E may increase warfarin effect Cranberry juice may increase warfarin effect Herbal/Nutraceuticals Cranberry, fenugreek, ginkgo biloba, glucosamine, may enhance bleeding or increase warfarin's effect Ginseng (American), coenzyme Q10, and St John's wort may decrease warfarin levels and effects Antibiotics and Warfarin Cytochrome P450 High risk >75% - eg Erythromycin, Clarithromycin, Ciprofloxacin, Cotrimoxazole, Metronidazole, Ketoconazole, Fluconazole Any broad-spectrum antibiotics can suppress production of vitamin K by the gut flora Management of elevated INR INR <6 No significant bleeding - Reduce dose or hold the next dose until INR <5 INR >6 and <8 No significant bleeding - Hold the next 1or 2 doses until INR <5 then resume lower dose INR >8: No significant bleeding - Hold warfarin until INR <5 - Vitamin K orally 5-10 mg or 0.5mg iv if high risk for bleeding Any INR elevation + Serious bleeding - Hold warfarin, give vitamin K (10 mg by slow I.V. infusion), and supplement with fresh plasma transfusion or prothrombin complex concentrate (factor X complex) Vitamin K and Warfarin Note: Use of high doses of vitamin K (10-15mg) may cause resistance to warfarin for more than a week Heparin or low molecular weight heparin can be given until the patient becomes responsive to warfarin Newer Anticoagulants Direct Thrombin Inhibitors Eg Hirudin, a naturally occurring anticoagulant Bind directly to thrombin's catalytic site rather than to antithrombin III Inhibit clot-bound thrombin Increased risk of major hemorrhage with hirudin Possible role in HITs Ximelegatran Oral direct thrombin inhibitor Concerns re: hepatotoxicity No antidote Antiplatelet agents Antiplatelet agents Predominantly prevent arterial thrombosis In acute setting of MI & ischaemic stroke Secondary prevention of vascular events Primary prevention when 10 yr risk >15% and BP controlled Antiplatelet drug targets Prostaglandin synthesis ADP binding GPIIb/IIIa receptor Cyclic AMP Antiplatelet agents Aspirin inhibits cyclo-oxygenase thromboxane A2 synthesis inhibits both COX 1 and COX 2 irreversibly COX-1 vs COX-2 inhibitors Aspirin Pros Inexpensive Proven efficacy Cons – Intolerance Limited potency Adverse effects GI ulceration 6-31% Haemorrhage Bronchospasm Interstitial nephritis, papillary necrosis, proteinuria, renal failure Reye’s syndrome in children CI <16yrs Dangerous in overdose Antiplatelet agents Theinopyridines eg Clopidogrel, Ticlopidine Block activation of platelets by reducing ADP activation of Gp IIb / IIIa receptor complex Clopidogrel Alternative to aspirin First choice for aspirin intolerance In addition to aspirin in context of Primary PCI Acute coronary syndromes Secondary prevention of MI but NOT stroke Adverse effects GI upset Bleeding Blood dyscrasias Aspirin + Clopidogrel significant increase in major (3.7 versus 2.7 percent for aspirin alone) and minor bleeding (5.1 versus 2.4 percent) bleeding risk with clopidogrel plus aspirin in patients who require coronary artery bypass graft surgery (CABG) Antiplatelet agents Glycoprotein IIb/IIIa inhibitors (eg abciximab, eptifibatide) – inhibit cross-bridging of platelets by fibrinogen – Fab fragment of monoclonal antibody GP IIb/IIIa inhibitors for ACS Among patients undergoing PCI with stenting Periprocedural administration of GP IIb/IIIa inhibitors improves outcomes in patients with a non-ST elevation ACS No evidence for benefit in context of thrombolysis Glycoprotein IIb/IIIa inhibitors Adverse effects Drug-induced thrombocytopaenia Bleeding Emergency CABG (abciximab-treated patients were more likely to require surgical reexploration for bleeding (12 versus 3 percent)) Antiplatelet agents Dipyridamole Inhibits platelet activation : by inhibiting platelet phospho-diesterase activity, stimulating prostacyclin synthesis, and blocking adensoine uptake Dipyridamole pyrimido-pyrimidine derivative vasodilatory effects on coronary resistance vessels increases intracellular platelet cAMP activating the enzyme adenylate cyclase, and inhibiting uptake of adenosine from vascular endothelium and erythrocytes *even the usual oral doses of dipyridamole may enhance exercise-induced myocardial ischemia in patients with stable angina Dipyridamole + Aspirin ESPS 2 Odds ratios for active treatment versus placebo Stroke ASA DP DP - ASA Stroke and / or Death ASA DP DP - ASA Risk Reduction % ASA 19.3 DP 21.5 DP - ASA 40.2 ASA 15.4 DP 18.5 DP - ASA 28.6 0.0 0.25 0.5 0.75 1.0 1.25 1.5 1.75 2.0 Summary Aspirin + Clopidogrel proven in - acute MI - ACS - prior to PCA + stenting - but not indicated in stroke prevention Summary GP IIb/IIIa inhibitors proven benefit - prior to PCI - provided CABG not required Dipyridamole possible role in stroke UFH/LMWH proven benefit in - acute coronary syndromes - short term therapy only Fibrinolytics Fibrinolytics Streptokinase, Urokinase, Alteplase (rt-PA), Reteplase, Tenecteplase MOA: Plasminogen activators Plasmin degrades fibrin and breaks up thrombi Streptokinase Derived from bacterial protein Antigenic (abys after 4 days) Cleaves Plasminogen Low fibrin specificity Cheap Urokinase Intrinsic compound Isolated from urine or renal cell cultures Non-antigenic Cleaves plasminogen Not licensed for MI Tissue plasminogen activator Intrinsic compound Recombinant DNA manufacture Non-antigenic Short half-life – give heparin afterwards Higher fibrin specificity Expensive ? More effective Reteplase/Tenecteplase Variants of TPA Longer half-life Easy to use More fibrin specific Indications Acute trans-mural MI within 12 hrs Ischaemic stroke within 3 hrs Massive PE Peripheral arterial thrombus Blocked lines Massive DVT Thrombosed prosthetic valves Indications in MI Clinical history of MI and either ST elevation or new LBBB True posterior MI As early as possible Little benefit after 12 hrs and no benefit after 24 Contra-indications Aortic dissection Recent or active bleeding Recent major surgery Bleeding diathesis or coagulation disorder Pregnancy Previous intracranial bleed Recent embolic CVA Complications Bleeding Allergic reactions Hypotension Arrhythmias Re-perfusion injury