* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Heart and Pericardium
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Artificial heart valve wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Myocardial infarction wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
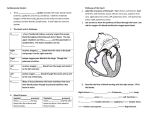
HEART AND PERICARDIUM I. Heart – Surface Landmarks Slide 2 A. Heart is a muscular pump slightly larger than a closed fist located in middle mediastinum 1. Approximately 1/3 of mass lies to right of midline and about 2/3 to the left Slide 3 2. Topographic surface landmarks on thoracic wall a. Apex of heart Left midclavicular line (MCL), at 5th intercostal space (ICS) b. Inferior border Horizontal from apex (MCL, 5th ICS) across midline to right border of sternum c. Left border From apex (MCL, 5th ICS) curves upward and medially to sternal end of left 2 nd intercostal space Runs at an oblique angle Slide 4, 5, 6 d. Valves Aortic semilunar valve o Surface projection Posterior to sternum, level of 3rd intercostal space o Auscultation location Right sternal margin, 2nd right intercostal space Pulmonary semilunar valve o Surface projection Left side of sternum, 3rd costal junction o Auscultation location Left sternal margin, 2nd left intercostal space Left sternal margin, 3rd left intercostal space Tricuspid valve o Surface projection Posterior to sternum, 4-5th costal junction o Auscultation location Lower-left sternal margin, 3rd or 4th left intercostal space Bicuspid (mitral) valve o Surface projection Left of 4th costal junction o Auscultation location 5th left intercostal space at MCL (location of apex of heart) Pericardium and Heart Page 1 of 6 II. Pericardium Slide 7 A. A tough fibroserous structure surrounding heart and initial portions of great vessels B. Closed sac composed of 2 layers Slide 8 1. Fibrous pericardium a. Tough outer connective tissue layer Consists of compact collagenous fibrous tissue b. Continuous superiorly with tunica adventitia of great vessels and pretracheal fascia of deep cervical fascia a. Because of the continuity, if you get an infection if can run up and down from these facial connections c. Attaches to posterior sternum via sternopericardial ligaments that are highly variable d. Continuous inferiorly with the central tendon of the diaphragm Site of continuity is referred to as the pericardiophrenic ligament Slide 9 2. Serous pericardium a. Thin, membranous inner layer b. Mainly a single layer of mesothelium (simple squamous epithelium) on a thin subserosal layer of connective tissue Subserosal layer contains fat of varying amounts o Prevalent along atrioventricular groove, inferior cardiac border and interventricular grooves o Main coronary vessels are embedded in this fat c. Two different layers described (continuous, double walled sac) Parietal Visceral 3. During development, the heart and great vessels invade serous pericardium Slide 10 and 11 a. Results in two layers of serous pericardium One layer lines inside surface of the fibrous pericardium and is referred to as parietal serous pericardium A second layer of serous pericardium directly adheres to the surface of the heart and is referred to as visceral serous pericardium (epicardium) b. The pericardial cavity is located between the visceral and parietal serous pericardiums Slide 12 c. Pericardial cavity is a potential space that contains a thin layer of serous fluid to reduce friction The heart is NOT contained in the pericardial cavity! Slide 13 Cardiac tamponade o Accumulation of fluid in the pericardial cavity compromises heart movement due to external compression o This is a confined space, so as fluid starts to build up it will compress the heart o This accumulation of fluid can be any fluid, not just blood, and is an abnormal collection of fluid o Compression of right atrium reduces venous return, and ultimately cardiac output o Ventricular walls are much thicker, so the atrium will compress before the ventricles Page 2 of 6 4. Visceral and parietal layers of serous pericardium become continuous where the great vessels enter and exit the heart Slide 15 a. Two sinuses form during development of heart due to heart tube folding Pericardial sinuses mark the points where visceral and parietal layers of serous pericardium reflect and become continuous with each other This occurs where the great vessels enter and exit the heart Location in the adult heart is marked by two sinuses: o Transverse and Oblique cardiac sinuses Slide 16, 17 b. Transverse cardiac sinus Associated with the reflection of serous pericardium along ascending aorta and pulmonary trunk Transversely oriented passage within pericardial cavity o Posterior to the ascending aorta and pulmonary trunk o Anterior to superior vena cava o Superior to atria of heart Important landmark used by cardiac surgeons o Can physically fit your finger in this space and that is particularly useful in bypass surgery Slide 18, 19 c. Oblique cardiac sinus Associated with the reflection of serous pericardium along pulmonary veins and inferior and superior venae cavae o Basically, reflection along where all the venous structures return to the heart Wide, pouch/pocket-like, blind recess that has an inverted “J” shaped border Posterior to base of heart (left atrium) Slide 20 C. Innervation of pericardium 1. Phrenic nerves the man innervation a. Sensory function ONLY – pain fibers b. Pericardium is sensitive to pain c. Ventral rami of C3,4,5 d. Runs over the anterior scalene m. in neck to run along sides embedded in the fibrous pericardium for this overall goal to gain access to the diaphragm a. it will give motor to the diaphragm, sensory branches just come off to give sensory to the pericardium (note Terreberry didn’t even mention 2 and 3) 2. Vagus nerves a. Function uncertain 3. Sympathetic trunks a. Vasomotor function Slide 21 D. Blood supply of pericardium 1. Branches of the following arteries supply the pericardium a. Mainly via Pericardiacophrenic branches of internal thoracic artery (which comes off the subclavian) - These course with the phrenic n. (note Terreberry didn’t even mention b, c, or venous drainage) b. Bronchial, esophageal and superior phrenic branches of thoracic aorta c. Coronary arteries Supply visceral pericardium only 2. Venous drainage of pericardium is via: a. Pericardiacophrenic veins either to internal thoracic or brachiocephalic veins b. Various tributaries of azygos system of veins in thorax Page 3 of 6 II. Heart Slide 22 A. The heart has three layers 1. Epicardium a. Outer layer b. This is the same as the thin layer of visceral serous pericardium (mesothelium) on surface of heart 2. Myocardium a. Middle layer of cardiac muscle 3. Endocardium a. Inner layer b. Thin layer of endothelium and subendothelial connective tissue that lines heart and covers valves Slide 23, 24 B. A fibrous framework within the heart provides attachment and support for cardiac muscle fibers and the valves 1. Complex framework of dense collagen rings a. Four rings surround orifices of valves b. Right and left fibrous trigones Near right trigone, there is an opening for the bundle of His This opening in the “insulation” allows information to go from the atria above to the ventricles below c. Membranous portions of interatrial and interventricular septa 2. This framework provide the following functions a. Keeps orifices of AV and semilunar valves patent (open), prevents them from being overly distended keep from collapsing under pressure b. Provides attachments for leaflets and cusps of valves c. Forms an electrical “insulator” by separating the atria and ventricles - This is a good thing because it keeps them from opening and closing at the same time Slide 24 C. Heart has four chambers (they are not all in the same plane with each other) 1. Right and left atria a. Atria are separated by a thin interatrial septum 2. Right and left ventricles a. Ventricles are separated by a thick interventricular septum 3. Right atrium and right ventricle referred to as the “right heart” a. Receives deoxygenated blood from body b. Pumps deoxygenated blood to lungs 4. Left atrium and Left ventricle referred to as the “left heart” a. Receives oxygenated blood from lungs b. Pumps oxygenated blood to body Slide 25 D. Surface anatomy 1. Surface of the heart is usually covered with variable amounts of fat 2. Apex of the heart a. Formed by the inferolateral part of the left ventricle b. Located downward and to the left along a point approximately 9 cm from the midline, in the left 5th intercostal space in adults c. Remains motionless throughout cardiac cycle Therefore, regardless of when the heart beats, it is always at the L 5 th intercostal space d. Is where sounds of mitral (bicuspid) valve closure are maximal – referred to as apex beat 3. Base (posterior aspect) of heart a. Formed primarily by the left atrium with some contribution from the right atrium b. Located along a horizontal line drawn across the level of the 3rd costal cartilage c. Faces posteriorly towards bodies of T 6-T9 vertebrae Separated from vertebrae by pericardium, oblique pericardial sinus, esophagus, aorta Page 4 of 6 d. The left atrial portion receives the pulmonary veins, while the right atrial portion receives the superior and inferior venae cavae Slide 26, 27 4. Four surfaces defined a. Anterior (sternocostal) surface Mainly right ventricle b. Diaphragmatic (inferior) surface Mainly left ventricle, partly right ventricle Related to central tendon of diaphragm c. Right pulmonary surface Mainly right atrium d. Left pulmonary surface Mainly left ventricle Forms cardiac impression in left lung Slide 28, 29 5. Four borders defined a. Right border Slightly convex Right atrium between superior and inferior venae cavae b. Inferior border Nearly horizontal Mainly right ventricle, slight left ventricle (*ask) c. Left border Oblique, nearly vertical Mainly left ventricle, slight left auricle d. Superior border Right and left atria in anterior view 6. Coronary (atrioventricular groove) sulcus is a groove on the surface of the heart that delineates the separation of the atria from the ventricles a. This sulcus encircles the heart 7. Anterior and posterior interventricular sulci are surface grooves delineating the interventricular septum Slide 30, 31 E. Great vessels enter and emerge from the chambers of the heart 1. Superior vena cava and inferior vena cava drain into right atrium a. Return deoxygenated blood to heart 2. Pulmonary trunk exits from right ventricle a. Divides into right and left pulmonary arteries b. Delivers deoxygenated blood to lungs 3. Right and left pulmonary veins drain into left atrium a. There are usually four pulmonary veins Superior and inferior right pulmonary veins Superior and inferior left pulmonary veins b. Return oxygenated blood from lungs to heart 4. Ascending aorta exits from left ventricle a. Delivers oxygenated blood from heart to rest of body Slide 32, 33 F. Blood flow through the heart 1. Deoxygenated blood flows into the right atrium from the superior and inferior venae cavae 2. From right atrium into the right ventricle through the tricuspid valve 3. Blood is pumped through the pulmonic semilunar valve into the pulmonary trunk and pulmonary arteries into the lungs for oxygenation 4. Oxygenated blood returns to the left atrium via the pulmonary veins 5. From left atrium into the left ventricle through the bicuspid (mitral) valve 6. Through aortic semilunar valve into ascending aorta for the systemic distribution Page 5 of 6 III. Extrinsic Innervation of Heart (slide 40 – summary pic) Slide 34 A. Cardiac plexus 1. A network of fibers with sympathetic, parasympathetic and sensory fibers 2. Located on the anterior surface of the bifurcation of the trachea into main bronchi as seen in the cadaver lab a. Associated with the posterior aspect of the ascending aorta and bifurcation of the pulmonary trunk Slide 35 B. Cardiac sympathetic fibers (short preganglionic, long post ganglionic) 1. Preganglionic cell bodies in IML (intermedial lateral cell column in the lateral horn of the spinal cord) of T1-T6 spinal cord levels 2. Axons leave out of the ventral root of the spinal cord, into sympathetic chain through white rami (whites are always preganglionic, and gray are always postganglionic) 3. Postganglionic cell bodies in cervical and upper thoracic sympathetic chain ganglia a. Synapse occurs in ganglia b. Postganglionic fibers contribute to cardiac plexus and terminate in the SA and AV nodes c. Most go to ventricles, some to atria Slide 36 4. Stimulation results in: a. Increased heart rate b. Increased force of contraction c. Increased impulse conduction d. Increased coronary blood flow Slide 37 C. Cardiac parasympathetic fibers (long preganglionic, short post ganglionic) 1. Preganglionic cell bodies in DMN X (dorsal motor nucleus of vagus nerve) in caudal medulla a. Preganglionic fibers contribute to cardiac plexus and terminate in intrinsic ganglia 2. Postganglionic cell bodies in unnamed intrinsic ganglia located in the atrial wall and interatrial septum near SA and AV nodes, and along the coronary arteries - Postganglionic neurons terminate in SA and AV nodes SA nodes mainly from right vagus AV nodes mainly from left vagus Slide 38 3. Stimulation results in: a. Decreased heart rate b. Reduced force of contraction c. Constriction of coronary vessels Slide 39 D. Afferent visceral pain fibers 1. Accompany the sympathetic fibers 2. These fibers enter the spinal cord mainly at the T 1-T4 levels, especially on the left side 3. Sensory information from the arm enters spinal cord at similar levels a. Pain from heart may appear to be pain in left arm as well b. An example of referred pain IV. Intrinsic Conducting System of Heart Slide 41 A. The heart has an intrinsic automatic rhythm, which is generated by the intrinsic conducting system of the heart 1. Consists of nodal tissue (initiates heartbeat) and specialized conducting fibers B. Role of extrinsic autonomic innervation is to modify the heart rhythm, but not to generate it parasympathetic and sympathetic only speed up the rate or slow it down, but do not determine what it is because of this intrinsic conductiong system Intrinsic conductions all by itself determine rate at about 70 beats per min C. See Heart Chambers and Valves lecture for more details Page 6 of 6