* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Nutrition, Diet in prevention of oral conditions. The role
Survey
Document related concepts
Low-carbohydrate diet wikipedia , lookup
Hadrosaur diet wikipedia , lookup
Diet-induced obesity model wikipedia , lookup
Gluten-free diet wikipedia , lookup
Vegetarianism wikipedia , lookup
Malnutrition wikipedia , lookup
Plant nutrition wikipedia , lookup
Calorie restriction wikipedia , lookup
Malnutrition in South Africa wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Vitamin D deficiency wikipedia , lookup
Food choice wikipedia , lookup
Transcript
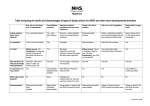
Prof. R.Kabaktchieva - 2014 Oral health, Diet, Nutritional status and General health are closely linked Nutrition is essential for the growth, development, and maintenance of oral structures and tissues. During periods of rapid cellular growth, nutrient deficiencies can have an irreversible effect on the developing oral tissues. Before tooth eruption, nutritional status can influence tooth enamel maturation , chemical composition, tooth morphology and size. Early malnutrition increases a child's susceptibility to dental caries in the primary teeth. Throughout life, nutritional deficiencies can affect host resistance, healing, oral function, and oral-tissue integrity. After tooth eruption, diet affects the dentition topically rather than systemically. Dietary factors and eating patterns can: initiate, exacerbate, or minimize dental decay. Fermentable carbohydrates are essential for the implantation, colonization, and metabolism of bacteria in dental plaque. Factors such as eating frequency and carbohydrate retentiveness on the dentition influence the progression of carious lesions, while foods containing calcium and phosphorus, such as cheese, enhance remineralization. Frequent intake of acidic foods or beverages can cause enamel erosion. Diet Assessment and Counseling in Dental Care The modern dental practitioner is concerned not only with educating patients for the prevention of caries and periodontal disease, but also plays an important role in screening patients for some health risks. a dietary assessment and screening can help identify potential nutritional problems that may affect, or be affected by, dental care. The role of the dental provider should be to screen patients for nutritional risk, provide dietary guidance related to oral health, and refer patients to nutrition professionals for treatment of other nutrition-related systemic conditions. Example: “Adolescents are at risk of caries because they have high intake of soft drinks and snack foods” Using current diet patterns patients should be taught : the role of diet in caries, what are cariogenic and noncariogenic eating patterns, how to adapt the current diet to lower cariogenic risk. - = Primary Prevention Secondary Prevention This strategy targets individuals showing early danger signs of caries, such as extensive cervical demineralization. Examples : Adolescents with cervical demineralization after removal of orthodontic appliances. Adolescents with demineralization due to gastroesophageal reflux disease. These individuals need from more-detailed guidance on how to reduce cariogenicity of their current diet. Thе guidance would involve determining the factors influencing current habits, Have to work with the patient to develop appropriate and acceptable strategies for improvement. Tertiary Prevention This strategy provides supportive and rehabilitative services to maximize the quality of life. Example: Pacients with a history of caries and many restorations This level of prevention should provide dietary advices to promote long-term change to prevent recurrence of caries. Example: Children with new orthodontic devices. This level of prevention may require dietary counseling to identify methods of preparing foods to facilitate consumption of a healthy diet when chewing may be compromised by tooth loss or new orthodontic devices. The Basis for a Healthy Diet “Dietary Reference Intakes” Daily food intake must meet metabolic requirements for energy (calories); Have to provide the essential nutrients that the body cannot synthesize in sufficient quantities to meet physiologic needs. The Dietary Reference Intakes (DRIs) are quantitative estimations of nutrient values to be used for planning and assessing diets for healthy people. These reference values vary by gender and life stage group. The Dietary Reference Intakes /DRIs / consist : - Estimated Average Requirement (EAR) - Recommended Dietary Allowance (RDA) - Adequate Intake (AI) - Тolerable Upper Intake Level (UL) Types of Daily Reference Intakes (DRI) Estimated Average Requirement (EAR) The daily nutrient intake value estimated to meet the needs of half (50%) of all healthy people in a life stage and gender group. Recommended Dietary Allowance (RDA) The average daily nutrient value considered adequate to meet the nutrient needs of nearly all (97%-98%) healthy people in a life stage and gender group. Adequate Intake (AI) An intake value assumed to be adequate for healthy people in each life stage and gender group when there is not enough data to determine an RDA. Тolerable Upper Intake Level (UL) The highest level of daily nutrient intake, what not cause adverse health risks for individuals in a life stage and gender group. The risk of adverse effects increases with intakes above the UL. Dietary Guidelines Dietary Guidelines include 9 interrelated focus areas. Each of the focus areas has several recommendations. The Guidelines place emphasis on consuming a nutrient-dense diet that does not exceed energy needs, having regular physical activity, and maintaining a healthy weight. Dietary Guidelines 1. Adequate Nutrients within Calorie Needs • Consume a variety of nutrient-dense foods and beverages in the basic food groups • Choos foods that limit the intake of saturated fats, cholesterol, added sugars, salt, and alcohol. • Choose a balanced eating pattern within energy needs Dietary Guidelines 2. Weight Management To maintain body weight in a healthy range, have to balance calories from foods and beverages with calories expended. make small decreases in food and beverage calories and increase physical activity. Dietary Guidelines recommend 3. Physical Activity Engage in regular physical activity and reduce sedentary activities to promote health, psychological well-being, and a healthy body weight. Through physical fitness achieve muscle strength and endurance. Dietary Guidelines recommend 4. Food Groups to Encourage Consume a sufficient amount of fruits and vegetables within energy needs. Choose a variety of fruits and vegetables each day. Consume 3 or more ounce of whole-grain products per day. Consume 3 cups per day of fat-free or low-fat milk or equivalent milk products. Dietary Guidelines recommend 5. Fats less than 10% of calories to be from saturated fatty acids and less than 300 mg/day of cholesterol. total fat intake have to be 20% - 35% of calories; Most fats coming from sources of polyunsaturated and monounsaturated fatty acids. When selecting and preparing meat, poultry, dry beans, and milk or milk products, make choices that are with, low-fat, or fat-free. Limit intake of fats and oils high in saturated fatty acids, and choose products low in such fats and oils. Dietary Guidelines recommend 6. Carbohydrates Choose fiber-rich fruits, vegetables, and whole grains often. Choose and prepare foods and beverages with little added sugars or caloric sweeteners. Reduce the incidence of dental caries by practicing good oral hygiene and consuming sugar- and starch-containing foods and beverages less frequently. Dietary Guidelines recommend 7. Sodium and Potassium Consume less than 2,300 mg (approximately 1 teaspoon of salt) of sodium per day. Choose and prepare foods with little salt. Dietary Guidelines recommend 8. Alcoholic Beverages does not apply to children !!! Dietary Guidelines recommend 9. Food Safety To avoid microbial foodborne illness: Clean hands, food contact surfaces, and fruits and vegetables. Meat and poultry should not be washed or rinsed. Separate raw, cooked, and ready-to-eat foods while shopping, preparing, or storing foods. Cook foods to a safe temperature to kill microorganisms. Refrigerate perishable food promptly and defrost foods properly. Avoid raw (unpasteurized) milk or any products made from unpasteurized milk, raw or partially cooked eggs or foods containing raw eggs, raw or undercooked meat and poultry, unpasteurized juices, and raw sprouts. MyPyramid MyPyramid is based on the Dietary Guidelines and the Daily Reference Intakes (DRIs). It translates this information into a diet that meets individual nutrition needs and urges moderation of dietary components that are commonly consumed in excess. Food pyramid - guide for rational nutrition Created in collaboration with the Health Ministry of USA. “MyPyramid “ is a symbol to the 6 food categories represented as vertical bands. The new pyramid has a symbol “a person climbing the side of the pyramid” it indicate the need for being physically active every day Foods are grouped according to similar nutrient composition. The food categories are : - whole grains, - vegetables, - fruits, - milk, - meats ,beans - oils Variety is essential to ensure adequate nutrition, because each group provides some, but not all, essential nutrients. It is recommended people to eat more of some foods (fruits, vegetables, whole grains, and fat-free or low-fat milk products) and less of other foods (saturated and trans fats, added sugars, cholesterol, salt, and alcohol) The narrowest part of the pyramid indicates foods that should be minimized because they contain more added sugars and fat. Tips to Get Started Make half your grains whole. Vary your veggies. Focus on fruit. Get your calcium-rich foods. Go lean with protein. Find your balance between food and physical activity. Nutritional Factors Affecting the Oral Cavity Nutrition plays an important role in the initial growth and development of oral tissues and in their continuous integrity through the lifespan. Optimal nutrition during periods of hard and soft tissue development allow these tissues to reach their optimal potential for growth and resistance to disease. Malnutrition, over- or undernutrition, during critical periods of organogenesis can have irreversible effects on developing tissues. Examples of this effect can be seen in - the tetracycline staining of teeth, - dental fluorosis, - enamel defects in children born prematurely, - the fever-induced enamel hypoplasia seen in the primary teeth. clinical cases Nutrients for which deficiencies or excesses have been directly associated with oral conditions are : - calories; - protein; - calcium; - phosphorus; - vitamins C, A, and D; - iodine; - fluoride. A summary of the oral symptoms of nutrient deficiencies can be found in Table . Oral Symptoms of Nutrient Deficiencies Nutrient- Oral Symptom of Deficiency Dietary Considerations- Cheilosis or angular stomatitis Rule out other etiology Glossitis Palliative treatment Riboflavin Hyperemia and Refer to MD/RD for (vitamin B2) or edema of the treatment with diet iron pharyngeal and modifications and/or oral mucous supplements membranes Oral Symptoms of Nutrient Deficiencies Nutrient- Oral Symptom of Deficiency Dietary Considerations- •Rule out other etiology •Palliative treatment •Refer to MD/RD for diet modifications: avoiding Niacin (vitamin •Bright red, sore tongue spicy or acidic foods, eat B3) or vitamin foods at room temperatur B12 eating nutrient and energ dense foods that are soft and moist Oral Symptoms of Nutrient Deficiencies Nutrient- Vitamin C Vitamin A Oral Symptom of Deficiency •Inflamed, bleeding gingiva and impaired wound healing (symptoms of scurvy, which is rare) •Changes in taste Dietary Considerations- •Rule out other etiology •Treat with diet modifications and/or supplements •Rule out other etiology •Refer to MD/RD for treatment with diet modifications to include nutrient and energy-dense foods and/or supplements •· Avoid foods that may Protein/Calorie Malnutrition Protein, the most abundant organic compound in the body, is required for the synthesis of virtually all body tissues and structures. Proteins account for the structure of DNA, the tensile strength of collagen, and the viscosity of saliva. Thus, aberrations in protein nutrition can have far-reaching oral and systemic effects. The normal turnover of epithelial tissue in the oral cavity requires a continual supply of nutrients. For example, every 3 to 6 days, the basal epithelium of the gingiva undergoes renewal. Thus, any severe deficiency of protein/calorie intake will result in a decrease in mitotic activity in the crevicular epithelium, as well as elsewhere throughout the body. In chronically malnourished children, studies have shown delays in tooth eruption and increased tooth enamel solubility, leading to increased caries susceptibility. The linear hypoplasia reported in the enamel of primary teeth to be related to the severity of the malnutrition. Оral defense mechanisms of saliva depend on an adequate supply of proteins. The glycoproteins that result in aggregation of bacteria arise from the salivary glands Lysozyme, salivary peroxidase, and lactoferrin are also glycoproteins. Secretory immunoglobulin A (sIgA) arises mainly from the labial and buccal glands The cell types involved in cellular immunity, polymorphonuclear lymphocytes , macrophages and the enzymes used in phagocytosis, also require protein for their production. Severe effects of protein/calorie deficiency are decrease of the cellular and immuno-cellular defenses of both the oral and the connective sides of the barrier epithelial cells lining the gingival crevice. The severity of the impaired immunologic response parallels the severity of the protein or calorie deficiency. Chronic malnutrition may also compromise cytokine response and affect immune cell function. In other words, undernutrition may impact immune response , tissue regeneration, and response to insult or infection. Minerals Calcium, in association with vitamin D and phosphorus, is essential for proper development and maintenance of mineralized tissues, especially teeth and alveolar bone. A deficiency of these nutrients during critical phases of tooth development in children results in hypomineralization of developing teeth and possible delayed eruption patterns. Enamel hypoplasia in primary teeth occurs in children born prematurely; Enamel hypoplasia in permanent teeth in these children is more that of controls. Preterm infants miss the intrauterine period when 80% of the body calcium, phosphorus, and magnesium are accumulated. In addition, very low birthweight infants have immature kidneys and may not metabolize adequate levels of vitamin D, further impairing tooth development. Iron - iron deficiency is the most common nutrient deficiency ; Iron deficiency anemia manifests in the oral cavity as pallor of oral tissues, especially the tongue. The tongue may appear shiny, with blunted filiform papillae. The effects of iron deficiency on mineralized tissues are less clear. Supplementing a caries-promoting diet with iron produced a major reduction in caries, Iron serves as a cofactor with ascorbic acid in collagen synthesis, as does copper. Zinc regulates function in inflammation by inhibiting the release of lysosomal enzymes and histamines. A zinc deficiency can inhibit collagen formation and reduce cell-mediated immunity. Zinc deficiency can also result in delayed wound healing, defective keratinization of epithelial cells, epithelial thickening, atrophic oral mucosa, and xerostomia. In addition, zinc is essential for taste and odor sensitivity. Vitamins Vitamin A is essential for the development and continued integrity of all body organs and tissues, including the epithelial mucosa of the oral cavity. In vitamin A deficiency, cell differentiation is impaired. The result is defective tissue formation and impaired healing. In Vitamin A deficiency both specific and nonspecific immuno-protective mechanisms are impaired Deficiency can affect tissue response to bacterial infection, mucosal immunity, parasitic and viral infection, activity of natural killer cells, and phagocytosis. Vitamin A toxicity can show similar effects, with impaired healing response being the most direct affect in the oral cavity. Vitamin A toxicity include other effects: proliferation of oral epithelium, reduction of the keratin layer, thickening of the basal membrane, and increase in the granular layer. Vitamin C, ascorbic acid, is essential to oral health. Synthesis of hydroxyproline, an essential component of collagen, requires ascorbic acid. Clinical manifestations of vitamin C deficiency called scurvy defects in collagen synthesis Signs of scurvy in the oral cavity include spontaneous bleeding, infusions of blood into interdental papillae, loosening and exfoliation of teeth, detachment of oral epithelial tissue, Frank scurvy is rare, The development of gingivitis is one of the early manifestations of vitamin C deficiency. The odds of having periodontal disease are greater in those with low dietary vitamin C intakes. After grapefruit consumption by patients with periodontitis, plasma vitamin C levels increase and bleeding scores improved. People with vitamin C deficiency supplemented with ascorbic acid have increase in hydroxyproline in periodontal tissues. Because the impact of deficient levels of vitamin C is first observed in gingival tissues, dentists and dental hygienists in clinical practice may be the first to diagnose the phenomenon. !!! The B-complex vitamins primarily function is as coenzymes in energy metabolism. B-complex vitamins are found widely in foods, and are usually found together. Deficiencies uncommon. of single B vitamins are Oral signs and symptoms of Bcomplex vitamin deficiencies include : - cracks in the corners of the mouth referred to as cheilosis, - inflammation, - burning, - redness, - pain and swelling of the tongue. Diet and Enamel Demineralization Dental demineralization can result from excessive tooth brushing, regurgitation of stomach acid, as in the eating disorder bulimia, or from excessive consumption of acid-containing foods or beverages. The demineralizing effect of acid from the diet is magnified in the presence of xerostomia, because saliva helps to neutralize acids and remove them from the oral cavity. Dietary sources of acid may include ; - citrus fruits and juices, - acidogenic sports drinks, - snacks containing citrus acid, - carbonated beverages, - chewable vitamin C tablets, - excessive regurgitation of gastric contents into the mouth. Recently, attention has been focused on the constant use of carbonated beverages, both regular and diet. Both contain acids and are possible contributors to an increase in enamel demineralization, leading to dental caries in young people. It is important to differentiate this type of erosion or demineralization from the caries process in which acid produced from plaque bacteria causes the enamel demineralization. Diet and Dental Caries Role of Carbohydrates Next lecture Dental caries is a diet-related, infectious, and transmissible disease that is strongly affected by diet. Streptococcus mutans are the predominant oral bacteria that initiate the caries process. To development of clinical caries is necessary the interaction of three local factors in the mouth: a susceptible tooth, cariogenic bacteria, and fermentable carbohydrate. Plaque bacteria ferment starches and sugars, producing organic acids. These acids demineralize dental enamel. Other dietary factors counteract the damaging effects of carbohydrates. The presence of protective minerals and ions, such as fluoride, calcium, and phosphorus in plaque and saliva, promote remineralization of incipient lesions. In addition to transporting minerals, saliva contains buffering agents, bicarbonate and phosphates, which neutralize organic acids. Thus, the amount and composition of saliva affect the caries process. Other host factors that influence caries risk include genetic predisposition, immune status, malnutrition during tooth formation, education level, and income status. Caries-Protective Foods and Nutrients Some components of foods are protective against dental caries - protein, fat, phosphorus, and calcium inhibit caries . Aged natural cheeses have been shown to be cariostatic. The protective effect of cheeses is attributed to their texture, which stimulates salivary flow, and their protein, calcium, and phosphate content, which neutralizes plaque acids. Many dairy products are now fortified with probiotic Lactobacillus rhamnosus GG, which has been shown to have an inhibitory affect on a wide range of bacteria including Streptococcus species. 37% to 56% reduction in caries risk after exposure, to these probiotic dairy products. Fluoride found in drinking water, foods, and dentifrices increase a tooth's resistance to demineralization and enhance remineralization of carious lesions. Lipids seem to accelerate oral clearance of food particles. Some fatty acids, linoleic and oleic, in low concentration, inhibit growth of mutans streptococcus. Lectins, proteins found in plants, appear to interfere with microbial colonization and may affect salivary function. Measuring the Cariogenic Potential of Foods next lecture Nutrition and Periodontal Diseases Like caries, periodontal disease is an infectious disease, is multifactorial in etiology, and occurs when virulence of the bacterial challenge is greater than the host defense and repair capability. The course of periodontal disease involves periods of progression and remission. Unlike the direct causative relationship between carbohydrates and caries, nutritional factors seem to play a much more subtle role in periodontal status. Nutritional factors can alter host susceptibility to periodontal disease and/or modulate its progress. The nutritional factors related to preventing infection and enhancing wound healing in general, applies to the prevention and management of periodontal disease as well. If both challenges, and the defense and repair capabilities of the periodontal tissues are in balance, nutrition could be the deciding factor in whether health or disease results. Even when the periodontium is healthy, there is continual need for nutrients to maintain the tissues. Once inflammation is established, the need for nutrients increases. There is a close relationship between malnutrition and infection, - infection aggravate malnutrition and malnutrition help infection. Host defense in the gingival crevice and connective tissue requires an adequate intake of all nutrients to ensure adequate production and function of defense and supporting cells. With the increased needs of cellular immunity and the additional demands by the tissue cells attempting to maintain and repair damaged areas, a greater supply of all nutrients is needed. Epidemiologic research also indicates that increasing intake of whole grains may reduce the risk for periodontitis. Whenever routine scaling, prophylaxis, and oral plaque-control procedures fail to reverse gingivitis and before any treatment for periodontitis is attempted, a session involving thorough diet evaluation and patient counseling is indicated. The patient should be informed about the importance of systemic nutrition in the defense and repair of oral tissues. Recommendations should be made to help ensure optimal nutrition to help prevent and manage periodontal disease. end Importance of Diet Assessment and Counseling in Dentistry Question 1 What are appropriate nutrition interventions for dental clinicians? A. Assess patients' nutritional status using laboratory and other biochemical assessment tools. B. Screen patients for nutritional risk. C. Recognize dietary problems in denture patients. D. Provide diet guidance related to oral health. 1. b, c, and d correct. a incorrect. It is not appropriate or possible for the dental team to attempt to assess actual nutritional status. This requires sophisticated laboratory testing under the supervision of a qualified medical professional. The Basis for a Healthy Diet Dietary Reference Intakes Dietary Guidelines for Americans Food Guide Pyramid Food Labels Question 2 The Daily Reference Intakes (DRI) are set at: A. the minimum amount of a nutrient needed to prevent deficiency. B. the maximum amount that will not cause toxicity. C. the average estimated requirement for healthy people. D. the average requirement plus a margin of safety. 2. d correct. a incorrect. The minimum amount of a nutrient needed to prevent deficiency is not considered an appropriate standard of adequacy b incorrect. The maximum amount of a nutrient that will not cause toxicity is the UL or upper tolerable limit c incorrect. The average estimated requirement for healthy people would mean that half of the population would require more. Thus it is not used as the criteria for healthy populations Nutrition in the Development and Integrity of Oral Tissues and Structures Protein/Calorie Malnutrition, Minerals , Vitamins Question 3 Which is true about vitamins and oral health? A. Vitamin-C-deficient wounds heal as well as nonvitamin-C-deficient wounds B. B. Vitamin A-toxicity does not have oral effects C. The oral manifestations of vitaminC. C deficiency are related to defects in collagen formation D. D. Effects of deficiency and toxicity are best studied in humans 3. c correct. a incorrect. Vitamin C-deficient wounds have poorer healing ability b incorrect. Vitamin-C deficiency affects all epithelial tissues including those in the oral cavity d incorrect. It is not ethical to conduct such studies in humans Diet and Nutrition in Oral Conditions: Background and Counseling Strategies Who Needs Diet Guidance Caries Prevention Question 4 The diet assessment process in dentistry is designed to: A. diagnose nutrient deficiencies B. help screen patients for oral-health risk factors C. serve as a teaching tool D. determine patients' daily caloric intake E. provide a therapeutic diet prescription for patients F. be part of total preventive assessment 4. b, c, and f correct. a incorrect. The diet assessment process can be used to screen patients for possible nutrition risk, but cannot be used for true nutritional assessment d incorrect. Daily calorie intake cannot be determined using a diet screening tool. Patient's daily calorie intake is best assessed by a registered dietitian using an assessment tool designed for that purpose. e incorrect. The dental team can use screening information to refer the patient to a registered dietitian who is qualified to provide therapeutic diets. The dental team can provide nutrition information about healthy diet and diet/oral health relationships. Dental Caries: Role of Carbohydrates in Caries Development Effects of Eating Patterns and Physical Form of Foods ( next lecture) Question 5. In the diet of a patient with rampant dental caries, which is most relevant to the problem? A. otal amount of sucrose consumed B. total amount of sticky sweets consumed C. nutrient quality of the meals and snacks D. number of meals and snacks E. what is eaten for desert in the evening 5. d correct a incorrect. Sucrose is not the only cariogenic factor, and the amount is not as important as the distribution in the diet. b incorrect. The amount of sticky sweets is not as relevant as the frequency of usage of these items. c incorrect. The nutrient quality of the diet is only related to the caries process after tooth eruption through remineralization effects. e incorrect. Dessert is only one of many contributing factors to dental caries. Measuring the Cariogenic Potential of Foods Question 6 Tooth erosion can be caused by A. acid from vomiting B. sugar-containing carbonated beverages C. gastro-esophageal reflux D. sugar-free carbonated beverages E. all of the above 6. e correct. Tooth erosion can be caused by acid from vomiting, sugar-containing carbonated beverages, gastroesophageal reflux, and sugarfree carbonated beverages to name but a few factors. Early Childhood Caries Nutrition and Periodontal Disease Diet Guidelines Question 7 Periodontal disease is caused by dietary deficiencies. Calcium deficiency is thought to be a contributing factor in alveolar bone loss in humans. A. both statements are true. B. both statements are false. C. the first statement is true: the second is false. D. the first statement is false the second is true. 7. d correct. Periodontal disease is not caused by dietary deficiencies. However, calcium deficiency is thought to be a contributing factor to alveolar bone loss in humans. Eating Disorders Question 8 Oral problems that may be seen in patients with eating disorders include: A. swollen salivary glands B. orange-stained teeth C. decreased salivary flow D. decreased oral pH E. severe enamel demineralization 8. a, c, d, e correct. b incorrect. Orange-stained teeth are not necessarily caused by eating disorders. The staining can come from food, beverages, or other sources.