* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Nefrologie číslo X, 200X
Coronary artery disease wikipedia , lookup
Rheumatic fever wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Electrocardiography wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Myocardial infarction wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Heart failure wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
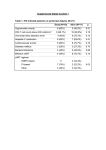
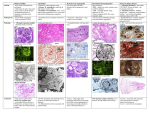
RENAL FUNCTION IN HEART FAILURE RENÁLNÍ FUNKCE PŘI SRDEČNÍM SELHÁNÍ A. Frangiosa, L. S. De Santo, M. Cirillo, A. Perna, M. Cotrufo, F. Rossi and N. G. De Santo Chairs of Nephrology, Heart Surgery, Pharmacology and Excellency Center for Heart Failure, Second University of Naples, Naples, Italy The importance of renal function in chronic heart failure Significant changes in renal function occur in heart failure due to cross talks brought about by the long-known relationships between pressures and flow rates and by neurohormonal activation. In the patient with a failing heart, survival has been linked to hyponatremia, hypomagnesemia as well as to potassium concentration (Leier and Boudolas 1992, Leier et al., 1994, Parameshawar et al., 1995, Hillege et al., 2000). Furthermore, plasma creatinine concentration has been identified as a strong predictor of mortality in patients with chronic heart failure (Hillege et al., 2000). Patients with chronic heart failure and creatinine clearance < 44 ml/min have a relative risk of mortality which is 2.85 times that measured in patients with a creatinine clearance > 76 ml/min. In the same group of patients, a weak prognostic value for mortality (< 2.0) was measured for NYHA class III-IV, and a relative risk of 1.35 left ventricular ejection fraction (LVEF) below 21%. Even azotemia, the worst index of renal function, has been identified as a predictor of mortality in patients with end-stage heart failure (ESHF). Blood urea in heart failure is slightly increased and is a significant indicator both of further deterioration of heart function as well as of excessive diuretic therapy. Azotemia may also increase following the administration of ACE inhibitors, today the cornerstone of therapy in patients with heart failure. The heart-kidney axis – the development of the concept Everything started with Richard Bright who, in his Report of Medical Cases, in 1837 stated that ”I have never yet examined the body of a patient dying of dropsy attended by coagulable urine, in whom some obvious derangement was not discovered in the kidneys. In all cases …it has appeared to me that the kidney has itself acted a more important part, and has been deranged both functionally and organically than has generally been imagined.” Subsequent developments of the concept emerged slowly (Andreoli 1999, Andreoli 1997). Nearly 16 decades has elapsed from this observation and Starling’s description of edema formation in heart failure. In this talk at the Royal College of Surgeons in 1896, having observed that in heart failure there is increased reabsorption of fluid from the limbs and from the gastrointestinal tract, Starling concluded that ”ultimate result of heart failure is a condition of hydraemic plethora and therefore, a raising of the mean systemic blood pressure above its normal height … the heart will be unable to send onwards into the arteries even its normal quantity” thus leading to hypothesize the importance of the effective circulating volume (Starling 1996). However, only with Peter’s monograph on Body Water (Peters 1935) published in 1935—that is more than two centuries after Bright—was the notion that the effective circulating volume greatly affected renal function definitely ascertained. Two final steps were outlined by Harrison who introduced the concept of forward and backward failure, and shed light on diastolic dysfunction (Harrison 1935), and by Stead and Erbert, who made clear that reduction in effective blood volume was the result of the difficulties in translocating fluid to the arterial side thus pointing to systolic dysfunction (Stead and Erbert 1942). However, it was only with Epstein, Post and Mc Dowell (Epstein et al., 1953) that the hypothesis of underfiling as ”the inadequate filling of the systemic arterial tree” was officially described and acquired to the pathophysiology and clinical practice. Renal plasma flow and glomerular filtration rate Renal blood flow is reduced in heart failure without changing the relation to cardiac output that remains in the range of 18-22%. However, GFR is to a lesser extent; thus the filtration fraction increases. Of course, peripheral vascular resistance and renal vascular resistance are significantly increased. Animal studies have revealed that efferent arteriolar resistance and glomerular hydraulic pressure increased. This notion was clearly established in humans by A. P. Merril et al as early as 1945 (Merill 1946). The evidence was put forward in a paper without using statistics. We do also know that there is a relation of renal plasma flow to cardiac index and to systemic resistance, but not to mean plasma flow (Stead and Erbert 1942). In our experience, the reduced GFR of ESHF patients does not prevent the capacity of the kidney to increase its function following an oral protein load; this was shown in an unpublished study performed at a time when ACE inhibitors (ACEi) were not a rule for such patients. A group of patients with heart failure was also studied before and after ACEi following a meat meal (2 g/kg BW of protein). Renal reserve was present in ACEi(-) and further increased when ACEi were added to therapy (Table 1). The renal hemodynamic response to a meat meal was also studied (Frangiosa et al., 1999) in ESHF patients on the waiting list for heart transplantation receiving ACEi, and in healthy age-, sex-, weight-, and height-matched controls. A reserve existed in ESHF and was not different from those in healthy controls (Table 2). Patient with mild heart failure had no reserve following intravenous amino acid administration; however, when ACEi were administered, a renal reserve was also found (Magri et al., 1998). However, it is difficult to understand why patients with mild heart failure have no reserve in the absence of ACEi while patients with NYHA III-IV have a reserve in ESHF in the absence of ACEi when receiving a meat meal. This points to a different mechanism between a protein meal and intravenous amino acids, and may also support the physiology of the meat meal. GFR in heart failure is preserved by efferent vasoconstriction with increasing hydrostatic pressure definitely enhancing net filtration. This vasoconstriction is mediated by hormonal mechanisms. In peritubular capillaries, hydrostatic pressure is low. However, oncotic pressure increases since protein remains in the capillary. This favors net fluid reabsorption. The hormonal cascade In heart failure, there is an increase in renin, angiotensin II, endothelin, ADH, aquaporin, aldosterone, noradrenaline, ANP, BNP, prostaglandin, and NO (Table 3). There has been long discussion about the nephrocentric view of heart failure. As reported in the book From Fish to Philosopher, Homer W. Smith defined renin secretion in heart failure as an unfortunate result of a well intentioned attempt of the kidney to preserve circulation (Smith 1953, Pacher 1990). Milton Pacher stresses the fact that the renin-angiotensin system evolved millions of years ago before the appearance of the macula densa and aldosterone secretion to maintain extracellular volume when life moved from sea water to dry land, i.e., from sea salt to salt depletion in the kidney when perfusion is reduced and the hormonal system is activated, which further decreases renal blood flow. Such nephrocentric response has been described as a heroic sacrifice by the kidney for the good of the body (Pacher 1990). This generates some pertinent questions. Why is renin secreted in HF? Why does the body neglect its detrimental action? Would not it be easier for the good of the organism to act on afferent arteriole and immediately reduce GFR? Indeed, is it the kidney that benefits from this action (Pacher 1990)? When underfilling occurs, angiotensin II, endothelin, ADH and catecholamines are secreted, and as potent vasoconstrictors, further reduce renal perfusion (Andreoll 1997, Andreoli 1999, Martin and Schrier 1997). Angiotensin II, which represents the most relevant stimulus for the secretion of aldosterone, stimulates (when at small concentrations) and depresses (when at high doses) sodium reabsorption in the proximal tubule. It also promotes thirst and potentiates the action of catecholamines and reduces glomerular filtration area. In turn, aldosterone stimulates sodium-potassium-ATPase and the sodium-hydrogen exchanger distally, thus increasing sodium retention and potassium excretion. Potassium stores are depleted in heart failure, even in patients who are well handled and this makes the case for sudden death due to hypokalemia. More has to be said on aldosterone since we do know that it is also produced in the rat heart thus indicating that there is a tissue system which makes autocrine and paracrine action possible (Silvestre et al., 1998). Furthermore, the pathways of aldosterone and glucocorticoid biosynthesis are changed after myocardial infarction. Under normal conditions, the action of 11-beta hydroxylase prevails and desoxicorticosterone is transformed mainly into corticosterone. After myocardial infarction, aldosynthase prevails and desoxicorticosterone is mainly transformed into aldosterone thus leading to fibrosis (Delcayre et al., 2000). ANP is produced by the atria and ventricles following an elevated atrial pressure, and opposes to angiotensin IIassociated vasoconstriction and reduces the effects of angiotensin II on proximal reabsorption of sodium. There is resistance to ANP in CHF. BNP is a 32-amino acid polypeptide that contains a 17-amino acid ring structure, which is typical of natriuretic peptides. The cardiac ventricles are the major source. BNP is now considered a marker for congestive heart failure. According to the 2001 ACC/ACA guidelines and BNP level greater than 100 pg/ml supports the diagnosis of abnormal ventricular function or symptomatic HF. Its use in differentiating dyspnoe due to HF from pulmonary disease and in managing patients with HF is under investigation. Vasodilatory PGE2 and PGI2 are released in heart failure and their plasma concentration correlates with that of angiotensin II; however, prostaglandin inhibitors reduced cardiac output in hyponatremic patients with heart failure. Two suicides The reduced filling of the arterial tree promotes hemodynamic changes and sodium avidity thus leading to increased end-diastolic volume by increased afterload and preload. This results in a depressed ejection fraction, which represents a suicidal arterial filling (Andreoli 1997, Andreoli 1999). The second suicide occurs via TNF alfa, which enhances the expression of proto-oncogenes involved in the apoptotic process and induces the expression in inducible NO synthase. There is great interest in the use of chimeric monoclonal antibodies to TNF alfa. Acid-base balance in heart failure In heart failure, various acid-base disorders may occur, either singly or in combination, which may depend on: 1. Renal loss of the hydrogen ion due to mineralocorticoid excess and/or diuretic therapy; 2. Angiotensin II; 3. Endothelin; 4. Adrenergic stimulation; 5. Hydrogen ion movements within the cell (hypokalemia); 6. Hypoxia; 7. Renal failure; 8. Increased respiratory rate; 9. Post hypercapnic states (after pulmonary edema due to left ventricular failure); 10. Reduced effective circulating volume. The patient may show metabolic alkalosis (due to potassium depletion, hypochloremia due to sodium intake and diuretics) as well as metabolic acidosis. The latter is a rare event as it may occur in patients with very low injection fraction impaired tissue metabolism or lactic acidosis or impaired renal excretion of the hydrogen ion (renal failure). Respiratory alkalosis supervenes with hypoxia, pulmonary interstitial edema and activation of chemoreceptors and chest stretch receptors. We have studied (Frangiosa et al., 1999) the acid-base status of 50 patients with ESHF before heart transplantation and 21 days after implantation when the patients underwent their endomyocardial biopsy. Data are given in Table 4. In pre-transplantation, a combined defect was present as mixed mild hypocapnic alkalosis and metabolic alkalosis. In fact, pH was in the upper limit of normalcy (alkalotic), pCO2 was reduced to about 2.5 mmHg, bicarbonates were in the limit of normalcy. After operation, the improved ejection fraction erased the respiratory alkalosis and only a mild metabolic alkalosis was present (pH in the alkaline range, normal pCO2, bicarbonate in the alkalosis range). Such changes do not call for therapy. Assessment of prognosis in chronic heart failure According to the 2001 ACC/AHA practical guidelines for the evaluation and management of chronic heart failure in the adult, the utility of LVEF diminishes once its value has declined to less that 25%. As the disease progresses, measurement of serum sodium concentration and renal function become increasingly important in defining the prognosis. Patients with chronic heart failure may develop diuretic resistance which may be defined as the failure to effect a negative net sodium balance, most often defined as failure to lose weight in a patient with edema receiving a diuretic drug (Suki 1999). There are many reasons for diuretic resistance; they are outlined in Table 5. For the patient with refractory ESHF, ACC/AHA practical guidelines 2001 suggest that ”If the degree of renal dysfunction is severe, or if the edema becomes resistant to treatment, ultrafiltration or hemofiltration may be needed to achieve control of fluid retention. The use of such methods can produce meaningful clinical benefits in patients with diuretic-resistant HF, and may restore responsiveness to conventional doses of loop diuretics”. At Cassino General Hospital in Italy (Iorio et al., 1997, Iorio et al., 2001), 16 patients were treated with daily hemofiltration with excellent results (Stellato et al., 1999), as indicated in Table 6. Bioelectrical impedance analysis before and after heart transplantation Patients with ESHF, when treated appropriately, may have total body water in the range of normal limits. A group of 23 patients was studied by body impedance analysis along with 69 age-, sex-, height-, and weight-matched healthy controls showing normal reactivity, and increased Xc (Stellato et al., 1999). The data support the notion that total body water may be in the normal range in ESHF patients, while extracellular water may be reduced and intracellular water increased. However, 3 days after heart transplantation, Xc fell below normal values 3 days after heart transplantation and normalized 12 days after transplantation (Stellato et al., 2001). Heart transplantation in patients with diuretic resistant edema In a study in patients undergoing heart transplantation, it was shown that patients in ”UNOS state 1” with severe hemodynamic distress despite massive dosage of diuretics, inotropes, vasodilators and intraortic balloon pump, with low urine output, hypotension and vasoconstriction requiring CAVH/dialysis and ad horas transplantation of the left ventricular assist system, have higher perioperative mortality (De Vivo et al., 1997, De Vivo et al., 1999). End-stage renal disease in heart transplant recipients With the advent of cyclosporin, heart transplantation has become a viable option in ESHF, with 5-year survival rates of 75% and 10-year survival rates of nearly 50%. The quality of life after transplantation is excellent. Long-term complications include coronary artery disease, malignancy and progressive renal dysfunction leading to end-stage renal disease and may therefore require dialysis and/or transplantation. Table 7 indicates (Myers and Newton 1991, Parameshawar et al., 1995, Pattison et al., 1995, Goldstein et al., 1997, Van Gelder et al., 1998) that the mean risk in 1,827 heart implants was 6.18% risk (range 3.4%-10%). There are many reasons for this high risk including older age, gender, black people, prevalence of hypertension (44-90% after 2 years), cyclosporin, hyperlipidemia, and creatinine clearance at the time of transplantation. In the experience at the Second University of Naples with 300 patients followed for 6 months to 11 years, only 3 patients needed continuous hemodialysis, that is only 1%. A very low prevalence, the lowest of the literature, which was obtained in patients with a mean pre-transplant creatinine clearance of about 71 ml/min. The cardiologist-nephrologist interaction There is a need for cardiologist-nephrologist interaction. The examples reported here support the notion of the nephrologist as the main consultant to the cardiologist caring for patients with a failing heart. Other examples could be easily provided supporting the need for the nephrologist to have the cardiologist as the main consultant when caring for patients with end-stage renal failure (De Santo et al., 2001). But—as observed by Milton Pacher (Pacher et al., 1992)—”as medicine is practiced in the 1990’s, patients with heart disease and renal disease are frequently managed by physicians who are interested only in one of the two organ systems.’’ Acknowledgements Studies at the Second University of Naples were financed by Regione Campania, ASI, and Second University of Naples. References 1. Andreoli T. Edematous states: an overview. In De Santo NG, Capasso G, Papalia T and De Napoli N, Eds. Edema Pathophysiology and Therapy. Kidney Int; 51 (Suppl): 2-10, 1997. 2. Andreoli T.E. Pathogenesis of renal sodium retention in congestive heart failure. In De Santo NG and Iorio L Eds, The Heart, Kidney and Renal Failure. Miner Electrolyte Metab 25: 11-20,1999. 3. De Santo NG, Perna A, De Santo LS, Cirillo M, Anastasio P, Pollastro RM, De Santo RM, Cotrufo M, Rossi F. The heart in uremia: role of hypertension, hypotension, and sleep apnea. Am J Kidney Dis 38: 115-117, 2001 4. De Vivo F, De Santo LS, Maiello C, Marra C, Marmo J, Cotrufo M. Heart transplantation in patients with diuretic resistant edema. Miner Electrolyte Metabol 25: 47-50, 1999. 5. De Vivo F, Luca S, De Santo, Maiello C, Trunfio R, Marra C, De Feo M, Damiani G, Galdieri N, Cotrufo M. Role of the heart surgeon in the emergency treatment of diuretic resistant edema grades III-IV heart failure. Kidney Int; 51 (suppl 59): 66-68, 1997. 6. Delcayre C, Silvestre JS, Garneierr A, Oubenaissa A, Cailmail S, Tatara E, Swynghedauw B, Robert V. Cardiac aldosterone production and ventricular remodeling. Kidney Int 57:1346-1351, 2000 7. Epstein FH, Post RS, McDowell M. The effect of an arteriovenous fistula in renal hemodynamics and electrolyte excretion. J Clin Invest 32: 233-241, 1953. 8. Frangiosa A, Favazzi P, Anastasio P, De Santo LS, Marra C, Molino C, Cirillo E, Stellato D, Saviano C, Pascale C, Pollastro RM, Cirillo M, Cotrugo M, De Santo NG, Adrogue HJ. The effects of transplantation on the acid-base state of patients with end stage heart failure pages 285-293. In Acid Base Balance- From bench to bedside, De Santo NG, Ed. Istituto Italiano per gli Studi Filosofici, Naples, 1999 9. Frangiosa A, Spitali L, Molino D, Cirillo E, De Santo LS, Marra C, Maiello C, De Vivo F, Pascale C, Favazzi P, Di Leo VA, De Santo NG, Anastasio P. Renal reserve is normal in patients with dilative cardiomyopathy waiting for heart transplantation. Miner Electrolyt Metab 25: 24-27, 1999. 10. Goldstein DJ, Zuech N, Sehgal V, Weinberg AD, Drusin R, Cohen D. Cyclosporine-associated end-stage nephropathy after cardiac transplantation. Transplantation 63: 664-668, 1997. 11. Harrison TR. The pathogenesis of congestive heart failure. Medicine 14: 255-260, 1935. 12. Hillege HL, Girbes ARJ, de Kam PJ, Boosma F, de Zeeuw D, Charlesworth A, Hampton JR, ven Veldhuisen DJ. Renal function, neurohormonal activation and survival in patients with chronic heart failure. Circulation 102:203210, 2000. 13. HW Smith. From Fish to Philospher, Boston, Little Brown, 1953. 14. Iorio L, De Santo LS, Violi F. Hemodialytic treatment of cardiac failure. Semin Nephrol 21: 278-281, 2001. 15. Iorio L, Simonelli R, Nacca RG, De Santo LS. Daily hemofiltration in severe heart failure. Kidney Int 51(Suppl. 59): 62-65, 1997. 16. Leier CV and Boudolas H. Cardiorenal Diseases and Disorders. Futura Publishing Company, 1992. 17. Leier CV, Dei Cas L, Metra M. Clinical relevance and management of the major electrolyte abnormalities in heart failure: hyponatremia, hypokalemia and hypomangesemia. Am Heart Journal 128:564-574, 1994. 18. Magri P, Rao MA, Cangialniello S, Bellizzi V, Russo R, Mele AF, Andreucci M, Memoli B, De Nicolo L, Volpe M. Early impairment of renal hemodynamic reserve in patients with asymptomatic heart failure is restored by angiotensin II antagonism. Circulation 98:2489-2854, 1998. 19. Martin PY, Schrier RW. Sodium and water retention in heart failure: pathogenesis and treatment. Kidney Int 51, Suppl. 59: 57-61, 1997 20. Merril AJ. Edema and decreased renal blood flow in patients with congestive heart failure: evidence of forward failure as the primary cause of edema. J Clin Invest 25:389-400, 1946 21. Myers BD, Newton L. Cyclosporine-induced chronic nephropathy: an obliterative microvascular renal injury. J Am Soc Nephrol 2: 45-52, 1991 22. Pacher M. Foreword. In Leier CV and Boudolas H Eds. Cardiorenal Diseases and Disorders. Futura Publishing Company, 1992. 23. Pacher M. Why do the kidneys release renin in patients with congestive heart failure? A nephrocentric view of converting-enzyme inhibition. Eur Heart J 11 (Suppl D); 44-45, 1990. 24. Parameshawar J, Keegan J, Sparrow J, Sutton GC, Poole-Wilson PA. Predictors of prognosis in severe heart failure. Br Heart Journal 74:341-342, 1995. 25. Parameshawar J, Schofield P, Large S. Long-term complications of cardiac transplantation. Br Heart J 74: 341-342, 1995 26. Pattison JM, Petersen J, Kuo P, Valantine V, Robbins R, Theodore J. The incidence of renal failure in one hundred consecutive heart-lung recipients. Am J Kidney Dis 26: 643-648, 1995. 27. Peters JP. Body Water. Springfield, Thoams 1935. 28. Silvestre JS, Heymes C, Aupetit-Faisant B, Mouas C, Moalic JM, Swyngheauw B, Delcayre C. Myocardial production of aldosterone and corticosterone in the rat: physiological regulation. J Biol Chem 272: 4483-4891, 1998. 29. Starling EH. Physiological factors involved in the causation of dropsy. Lancet 1407-1410, 1996 30. Stead EA Jr., Erbert RV. Shock syndrome produced by failure of the heart. Arch Intern Med 69: 75-89, 1942. 31. Stellato D, Cirillo M, De Santo LS, Maielloo C, Marra C. De Vivo F, Anastasio P, Frangiosa M, Cirillo G, Cotrufo M, De Santo NG, Di Iorio B. Body impedance studies in end stage heart failure. Miner Electrolyte Metab 25: 21-23, 1999 32. Stellato D, Ciruillo M, De Santo LS, Anastasio P, Frangiosa A, Cotrufo M, De Santo NG, Di Iorio B. Bioelectrical impedance analysis in heart transplantation: early and late changes. Semin Nephrol 21: 282-285, 2001. 33. Suki WN. Diuretic resistance. Miner Electrolyte Metab 25: 28-31, 1999. 34. Van Gelder T, Balk AHHM, Zietse R, Hesse C, Mochtar B. Renal insufficiency after heart transplantation: a case control study. Nephrol Dial Transplant 12: 2322-2326, 1998. Annamaria Frangiosa, MD 5 via Pansini, Pad 17, Nephrology SUN 80131 Naples, Italy phone: 0039 081 5666650 fax: 0039 081 5666655 Table 1: GFR and renal reserve (ml/min x 1.73 m2) following a meat meal (2 g/kg b.w. of proteins as cooked red meat) in end-stage heart failure Table 2: GFR, RPF, and renal reserve (ml/min x 1.73 m2) and FF (%) in patients with end-stage heart failure receiving ACEi (Frangiosa et al., 1999) Table 3: Hormonal activation in end-stage heart failure Table 4: Acid-base status before and after heart transplantation in 50 patients (Frangiosa et al., 1999) Table 5: Mechanisms of diuretic resistance (Suki 1999) Table 6: Hemofiltration in heart failure (Iorio et al., 1997, Iorio et al., 2001) Table 7: Patients with end-stage renal disease after heart transplantation (29-33)