* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Lobna Al AL Juffali Fall 2010
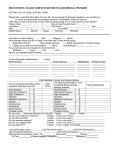
Survey
Document related concepts
Transcript
Lobna Al AL Juffali Fall 2010 Upper respiratory tract ◦ Nose, oropharynx, and larynx Lower respiratory tract ◦ Lower airways and lungs Upper and lower airways Nose Passageways that allow air to reach the Pharynx lungs 1. Purify Larynx (speech) 2. Humidify Trachea 3. Warm incoming air Bronchi and their smaller branches lungs Alveoli Gas exchange The major function of the respiratory system is to supply the body with oxygen and to dispose of carbon dioxide. Hypoxia: Decreased levels of oxygen in the tissues. Hypoxemia: Decreased levels of oxygen in arterial blood. Hypercapnia: Increased levels of CO2 in the blood. Hypocapnia: Decreased levels of CO2 in the blood. Dyspnea: Difficulty breathing. Tachypnea: Rapid rate of breathing. Cyanosis: Bluish discoloration of skin and mucous membranes due to poor oxygenation of the blood. Hemoptysis: Blood in the sputum. Pharyngitis is an acute infection of the oropharynx or nasopharynx that results in 1% to 2% of all outpatient visits. The incubation period is 2 to 5 days, and the illness often occurs in clusters PHARYNGITIS viral causes are most common rhinovirus, coronavirus, and adenovirus causes ACUTE Pharyngitis Bacterial Group A β-hemolytic Streptococcus 15% to 30% Streptococcus pyogenes bacteria or viruses may directly invade the pharyngeal mucosa, causing a local inflammatory response. rhinovirus and coronavirus, can cause irritation of pharyngeal mucosa secondary to nasal secretions. Streptococcal infections are characterized by local invasion and release of extracellular toxins and proteases. acute rheumatic fever acute glomerulonephritis reactive arthritis may occur as a result. Signs and symptoms A sore throat of sudden onset that is mostly selflimited Pain on swallowing. Fever. Headache, nausea, vomiting, and abdominal pain (especially children). Erythema/inflammation of the tonsils and pharynx with or without patchy exudates. Enlarged, tender lymph nodes. Red swollen uvula, petechiae on the soft palate Several symptoms that are not suggestive of Group A are cough, conjunctivitis, and diarrhea. Streptococcus Throat swab and culture or rapid antigen detection testing Rhinitis ◦ Inflammation of the nasal mucosa Sinusitis ◦ Inflammation of the paranasal sinuses that persists beyond 7–14 days Chronic/recurrent infections occur three to four times a year and are unresponsive to steam and decongestants. Acute rhinosinusitis Subacute rhinosinusitis Chronic rhinosinusitis ◦ May be of viral, bacterial, or mixed viral-bacterial origin ◦ May last from 5 to 7 days up to 4 weeks ◦ Lasts from 4 weeks to less than 12 weeks ◦ Lasts beyond 12 weeks Occurrence ◦ Occurs in conjunction with allergic rhinitis ◦ Mucosal changes are the same as allergic rhinitis Symptoms ◦ Nasal stuffiness, itching and burning of the nose, frequent bouts of sneezing, recurrent frontal headache, watery nasal discharge Treatment ◦ Oral antihistamines, nasal decongestants, and intranasal cromolyn Acute -disease lasts less than 30 days with complete resolution of symptoms -S. Pneumoniae and H. influenzae Chronic Bacterial SINUSITIS viral -episodes of inflammation lasting more than 3 months with persistence of respiratory symptoms. -Polymicrobial - anaerobes -gram-negative bacilli -fungi condition Signs and symptoms Acute •Nasal discharge/congestion. •Maxillary tooth pain, • facial or sinus pain that may radiate (unilateral in particular) as well as deterioration after initial improvement. • Severe or persistent (beyond 7 days) signs and symptoms are most likely bacterial and should be treated with antimicrobials. Children: •Nasal discharge and cough for greater than 10–14 days •temperature 39°C (102.2°F) • facial swelling •pain Chronic Symptoms •are similar to those of acute sinusitis but more nonspecific. • Rhinorrhea is associated with acute exacerbations. •Chronic unproductive cough, laryngitis, and headache may occur. Adults: The common cold is a viral infection of your upper respiratory tract . more than 200 viruses can cause a common cold, symptoms tend to vary greatly. Most adults are likely to have a common cold two to four times a year. Children 6-10 times a year. Most people recover from a common cold in about a week or two. Is a viral infection that can affect the upper or lower respiratory tract. influenza season usually runs from November to April Three distinct forms of influenza virus have been identified: A, B and C. Of these three variants, type A is the most common and causes the most serious illness. The influenza virus is a highly transmissible respiratory pathogen. Because the organism has a high tendency for genetic mutation, new variants of the virus are constantly arising in different places around the world. Influenza infection can cause marked Inflammation of the respiratory epithelium leading to acute tissue damage and a loss of ciliated cells that protect the respiratory passages from other organisms. As a result, influenza infection may lead to coinfection of the respiratory passages with bacteria. It is also possible for the influenza virus to infect the tissues of the lung itself to cause a viral pneumonia. influenza cold onset sudden gradual fever Charecteristic , high >38˚C 3-4 days duration rare cough Dry hacking headache prominent rare myalgia (muscle aches/pains) Usual ; often severe slight Tiredness and weakness Can last up to 2-3 weeks Very mild Extreme exhaustion Early prominent never Chest discomfort common Mild to moderate Stuffy nose sometimes common Sneezing sometimes usual Sore throat sometimes common Pneumonia is the most common cause of death due to infectious disease Seventh most common cause of death in the USA Hospital acquired Pneumonia is the second most common nosocomial infection(0.6%-1.1%) Mortality rates are CAP without hospitalization 1% CAP with hospitalization about 14% Nosocomial about 33-50% approximately three million cases are diagnosed annually at a cost of more than $20 billion to the healthcare system. Pneumonia occurs throughout the year, with the relative prevalence of disease resulting from different etiologic agents varying with the seasons. It occurs in persons of all ages clinical manifestations are most severe in the very young, the elderly, and the chronically ill. Pneumonia Hospital Acquired Pneumonia Ventilator Hospital acquired Health care Community Acquired Pneumonia Pneumonia (depending on the type of organism Typical Atypical S. pneumoniae, H. influenzae, Staphylococcus aureus, and enteric Gram-negative bacteria Mycoplasma, Legionella,Chlamydia Viral and TB inhaled as aerosolized particles via the bloodstream from an extrapulmonary site of infection aspiration of oropharyngeal contents may occur. 1.Mechanical Epithelial cells are covered with beating cilia blanketed by a layer of mucus. Each cell has about 200 cilia that beat up to 500 times/min, moving the mucus layer upward toward the larynx. The mucus itself contains antimicrobial compounds such as lysozyme and secretory IgA antibodies. the cough reflex to clear aspirated material 2.Cellualr Bacteria that reach the terminal bronchioles, alveolar ducts, and alveoli are inactivated primarily by alveolar macrophages and neutrophils. 3.Humoral Opsonization of the microorganism by complement and antibodies enhances phagocytosis by these cells. Depends on the etiologic agent Bacterial An intraalveolar suppurative exudate with consolidation Lobar pneumonia bronchopneumonia Viral or Mycoplasma pneumonia An interstial inflammation with accumulation of an infiltrate in the alveolar walls No exudates No consolidation Fungal Patchy distribution of granulomas Which undergo caseous necrosis with the development of cavaties Age >65 Aspiration of oropharyngeal secretions Viral respiratory infections Chronic illness and debilitation Chronic respiratory disease(COPD,astha,cystic fibrosis) Cancer Prolonged bedrest Tracheastomy or endotracheal tube Abdominal thoracic surgery Rib fractures Immunosuppressive therapy AIDS Smocking history Alcoholism malnutrition Acute Infection of the pulmonary parenchyma accompanied by the presence of an acute infiltrate on chest radiograph or ausculatory findings consistent with pneumonia . in patients who are not hospitalized or in a long –term care facility for 14 days or more before symptoms appear Microbiology S. pneumoniae H. Influenzae S. aures Gram –ve bacilli Legionella species M. Pneumoniae viral No diagnosis Pneumococci reachs the alveoli in droplets of mucus or saliva. The lower lobes of the lungs are frequently involved because of the effect of gravity. 1.Engorgement • Serious exudates Pours into the alveoli from the dilated ,leaking blood vessels (4-12 hrs) 2. Red hepatization Next 48 hrs 3.Gray hepatization 3-8 days 4.Resolution 7-11days • The lung becomes red As RBCS, fibrin, and PMN leukocytes fill the alveoli. • Lung become gray as the leukocytes and fibrin consolidate in the involved alveoli • Exudate is lysed and resorbed by macrophages, restoring the tissue to its original structure Sudden Chills ,fever Pleuritic pain Cough Rust colored sputum Hypoxemia As a result of shunting of blood through the non ventilated, consolidated area of lung Consolidation Plural effusions Death chronically ill elderly Bacteremia which leads to ( endocarditis, meningitis and peritonitis) Chest radiograph Dense lobar or segmental infiltrate Laboratory examination Leukocytosis with a predominance of polymorphonuclear cells Sputum examination (gross appearance ,microscopic examination and culture) Blood culture Should be done in certain high risk patients (e.g. sever CAP, chronic liver disease). Low oxygen saturation on arterial blood gas or pulse oximetry HAP: Pneumonia that occurs 48 hrs or more after admission Which was not incubating at the time of admission Ventilator- associated Pneumonia that arises more then 48-72 hrs after endotracheal intubation Health care associated Pneumonia: pneumonia developing in a patient who is hospitalized in an acute care hospital for 2 or more days within 90 days of the infection; resides in a nursing home or along-term facility received recent IV AB therapy, chemotherapy, or wound care within the past 30 days of the current infection ; or attended a hospital or hemodialysis clinic Microorganisms Gram-negitive bacilli S. Aures Anarobic bacteria H. Influenzae Gram-negitive bacilli Pseudomonas aeruginosa Acinetobacter Spp. Enterobacter Spp. Viral Cytomegalovirus Influenza Respiratory syncytial virus Fungi Aspergillus Cause extensive damage to the lung parenchyma Complications such as lung abscess and emphysema Mortality is high 33% 1. 2. 3. 4. 5. 6. 7. Intubation and mechanical ventilation Supine patient position Enteral feeding pharyngeal colonization Stress bleeding prophylaxis Blood transfusion Hyperglycemia 8. 9. 10. 11. 12. 13. 14. 15. Immunosuppression/corticosteriods Surgical procedures :thoracoabdominal, upperabdominal ,thoracic Immobilization Nasogastric tubes Prior antibiotic therapy Admission to ICU Elderly Underlying chronic lung disease Pathological consequences of the entery of oropharyngeal secretions,particulate matter,or gastric contents into the lower airway. Colonization of oropharynx and gastric plays a critical role in aspiration pneumonia. GM-ve organisms within 48 hrs of hospitalization Aspiration of orophyrngeal secretions occurs during sleep and is enhanced by 1. 2. 3. 4. nasogastric tube Altered consciousness Depressed gag reflex Delayed gastric emptying Bacterial counts rise Sucrulfate is a medication that heals ulcer without altering the gastric pH. Aspiration of particulate matter Aspiration pneumonia Anaerobic pneumonia Mendelson’s pneumonia Aspiration of oropharyngeal secretions containing anerobes Such as Bacteroids, Fusobacterium, Peptococcus,and Peptostreptococcus species. Common among patient with poor hygieneand chronic alcoholism Onset of symptoms 1-2 weeks Most distinguish symptom is productive cough of foul- smelling sputum Related to the regurgitation and aspiration of the acidic stomach contents. May lead to sudden death (obstruction) It follows three patterns 1. Rapid recovery (small amount or alkaline) 2. Rapid development of acute respiratory distress syndrome 3. Bacterial superinfection If the object is lodged high in the trachea complete obstruction ,apnea, aphonia and rapid death If the object is lodged in smaller airways Chronic cough And recurrent infections Atypical pneumonia refers to pneumonia caused by certain bacteria - namely, Legionella pneumophila, Mycoplasma pneumoniae, and Chlamydophila pneumoniae or virsus. atypical pneumonias are commonly associated with milder forms of pneumonia, pneumonia due to Legionella, in particular, can be quite severe and lead to high mortality rates. Symptoms Confusion (especially with Legionella pneumonia) Diarrhea (especially with Legionella pneumonia) Muscle stiffness and aching , Rash (especially with mycoplasma pneumonia)