* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Unit 3-4 Circulatory System Notes File
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Artificial heart valve wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
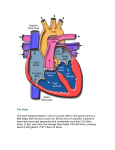
Cardiovascular system – The Heart and blood vessesls Overview of Blood Circulation Blood leaves the heart via arteries that branch repeatedly until they become capillaries Oxygen (O2) and nutrients diffuse across capillary walls and enter tissues Carbon dioxide (CO2) and wastes move from tissues into the blood Oxygen-deficient blood leaves the capillaries and flows in veins to the heart This blood flows to the lungs where it releases CO2 and picks up O2 The oxygen-rich blood returns to the heart Pathway of Blood Through the Heart and Lungs 1. Right atrium tricuspid valve right ventricle 2. Right ventricle pulmonary semilunar valve pulmonary arteries lungs 3. Lungs pulmonary veins left atrium 4. Left atrium bicuspid valve (mitral) left ventricle 5. Left ventricle aortic semilunar valve aorta 6. Aorta systemic circulation Coronary Circulation Coronary circulation is the functional blood supply to the heart muscle itself Atria of the Heart •Function: Atria are the receiving chambers of the heart •Blood enters right atria from superior and inferior venae cavae and coronary sinus •Blood enters left atria from pulmonary veins Ventricles of the Heart •Function: Ventricles are the discharging chambers (pumps) of the heart •Right ventricle pumps blood into the pulmonary trunk •Left ventricle pumps blood into the aorta Vessels returning blood to the heart include: Right and left pulmonary veins (from lungs) Superior and inferior venae cavae (from the rest of the body) Vessels conveying blood away from the heart include: Aorta Right and left pulmonary arteries Superior vena cava Right pulmonary vein Left pulmonary Vein Mitral Valve Pulmonary Valve Tricuspid Valve Inferior vena cava Aortic Valve Heart Valves •Heart valves ensure unidirectional blood flow through the heart Atrioventricular Valve Function •Atrioventricular (AV) valves lie between the atria and the ventricles •AV valves prevent backflow into the atria when ventricles contract •Chordae tendineae anchor AV valves to papillary muscles Semilunar Valve Function Aortic Valve - Aortic semilunar valve lies between the left ventricle and the aorta Coronary Valve - Pulmonary semilunar valve lies between the right ventricle and pulmonary trunk Heart sounds (lub-dup) are associated with closing of heart valves First sound occurs as AV valves close and signifies beginning of systole Second sound occurs when SL valves close at the beginning of ventricular diastole Microscopic Anatomy of Heart Muscle •Cardiac muscle is striated, short, fat, branched, and interconnected •The connective tissue endomysium acts as both tendon and insertion •Intercalated discs anchor cardiac cells together and allow free passage of ions •Heart muscle behaves as a functional syncytium (like a single unit) Heart muscle: •Is stimulated by nerves and is self-excitable (automaticity) •Contracts as a unit •Has a long (250 ms) absolute refractory period Cardiac muscle contraction is similar to skeletal muscle contraction Heart Physiology: Intrinsic Conduction System Specialized cells with rythmic changing membrane potential Autorhythmic cells: sinoatrial node & atrioventricular node Initiate action potentials Have unstable resting potentials called pacemaker potentials Use calcium influx (rather than sodium) for rising phase of the action potential Pacemaker and Action Potentials of the Heart 1. 2. 3. Hyperpolarization opens Na+ channels (Na+ influx, depolarization) Depolarization causes Ca2+ channels to open (Ca2+ influx, big depolarization) Ca2+ and Na+ channels close K+ channels open (Ca2+ outflow, repolarization then hyperpolarization) Depolarization of autorythmic cells is spread to rest of cardiac muscle through gap junctions. There, normal excitation-contraction coupling occurs. Signal does not spread from atria to ventricles because there is no gap junction between the two regions of heart. Heart Physiology: Sequence of Excitation Sinoatrial (SA) node generates impulses about 75 times/minute Atrioventricular (AV) node delays the impulse approximately 0.1 second Impulse passes from atria to ventricles via the atrioventricular bundle (bundle of His) AV bundle splits into two pathways in the interventricular septum (bundle branches) Bundle branches carry the impulse toward the apex of the heart Purkinje fibers carry the impulse to the heart apex and ventricular walls Heart Excitation - Electrocardiography (ECG or EKG) •Electrical activity is recorded by electrocardiogram (ECG) •P wave corresponds to depolarization of SA node •QRS complex corresponds to ventricular depolarization •T wave corresponds to ventricular repolarization •Atrial repolarization record is masked by the larger QRS complex AP for cardiac muscle has extra SLOW voltage-gated Ca2+-channel (slow = opens after faster) Ca2+ K+ Membrane potential Na+ 2. Na+ Influx 1. Fast volt-gated Na+-ch opens 2. Na+ Influx 3. volt-gated Na+-ch closes time ++ + 1. volt-gated Na+-ch opens + + + SLOW volt-gated Ca2+-ch opens 3. v-g Na+-ch closes v-g Ca2+-ch opens v-g K+-ch opens volt-gated K+-ch opens 4. Ca2+ Influx K+ Outflux 4. Ca2+ Influx K+ Outflux + in depol Cancel each other out 5. volt-gated Ca2+-ch closes 6. only K+ outflux + out repol + 5. v-g Ca2+-ch closes + 6. only K+ Outflux Regulation of Heart Rate Autonomic Nervous System •Sympathetic nervous system (SNS) stimulation is activated by stress, anxiety, excitement, or exercise •Parasympathetic nervous system (PNS) stimulation is mediated by acetylcholine and opposes the SNS •PNS dominates the autonomic stimulation, slowing heart rate and causing vagal tone Chemical Regulation of the Heart •The hormones epinephrine and thyroxine increase heart rate •Intra- and extracellular ion concentrations must be maintained for normal heart function Tachycardia – abnormally fast heart rate – over 100bpm Bradycardia – slow heart rate – under 60 bpm (good in athletes who have higher stroke volume (SV) Normal sec Bradycardia, Sinus Rhythm Normal P, QRS, T, rate < 60 sec Tachycardia, Sinus Rhythm Normal P, QRS, T, rate > 100 sec Ventricular Tachycardia (VTAC) Bizarre, wide QRS, no Pwav, rate > 100 sec Hypercalcemia Short/absent ST segment sec Ventricular Fibrillation (VFIB) Chaotic waves sec Asystole Flatline http://www.gwc.maricopa.edu/class/bio202/cyberheart/ekgqzr0.htm Blood Flow Actual volume of blood flowing through a vessel, an organ, or the entire circulation in a given period: Is measured in ml per min. Is equivalent to cardiac output (CO), considering the entire vascular system Is relatively constant when at rest Varies widely through individual organs Blood Pressure (BP) Force per unit area exerted on the wall of a blood vessel by its contained blood Expressed in millimeters of mercury (mm Hg) Measured in reference to systemic arterial BP in large arteries near the heart The differences in BP within the vascular system provide the driving force that keeps blood moving from higher to lower pressure areas Resistance – opposition to flow •Measure of the amount of friction blood encounters •Generally encountered in the systemic circulation •Referred to as peripheral resistance (PR) The three important sources of resistance are 1. blood viscosity – “stickiness” of the blood 2. total blood vessel length – longer = more resistance 3. blood vessel diameter Changes in diameter are frequent and significantly alter resistance Resistance varies inversely with the fourth power of vessel radius For example, if the radius is doubled, the resistance is 1/16 as much Blood Flow, Blood Pressure, and Resistance Blood flow (F) is directly proportional to the difference in blood pressure (P) between two points If P increases, blood flow speeds up; if P decreases, blood flow declines Blood flow is inversely proportional to resistance (R) If R increases, blood flow decreases R is more important than P in influencing local blood pressure Systemic Blood Pressure The pumping action of the heart generates blood flow through the vessels along a pressure gradient, always moving from higher- to lower-pressure areas Pressure results when flow is opposed by resistance •Is highest in the aorta •Declines throughout the length of the pathway •Is 0 mm Hg in the right atrium steepest change in blood pressure at arterioles Arterial Blood Pressure Arterial BP reflects two factors of the arteries close to the heart Their elasticity (compliance or distensibility) The amount of blood forced into them at any given time Blood pressure in elastic arteries near the heart is pulsatile (BP rises and falls) Systolic pressure – pressure exerted on arterial walls during ventricular contraction Diastolic pressure – lowest level of arterial pressure during a ventricular cycle Pulse pressure – the difference between systolic and diastolic pressure Mean arterial pressure (MAP) – pressure that propels the blood to the tissues MAP = diastolic pressure + 1/3 pulse pressure Capillary Blood Pressure Capillary BP ranges from 20 to 40 mm Hg Low capillary pressure is desirable because high BP would rupture fragile, thin-walled capillaries Low BP is sufficient to force filtrate out into interstitial space and distribute nutrients, gases, and hormones between blood and tissues Venous Blood Pressure Venous BP is steady and changes little during the cardiac cycle The pressure gradient in the venous system is only about 20 mm Hg A cut vein has even blood flow; a lacerated artery flows in spurts Factors Aiding Venous Return Venous BP alone is too low to promote adequate blood return and is aided by the: Respiratory “pump” – pressure changes created during breathing suck blood toward the heart by squeezing local veins Muscular “pump” – contraction of skeletal muscles “milk” blood toward the heart Valves prevent backflow during venous return Monitoring Circulatory Efficiency Efficiency of the circulation assessed by taking pulse and blood pressure Vital signs – pulse and blood pressure, along with respiratory rate and body temperature Pulse – pressure wave caused by the expansion and recoil of elastic arteries Radial pulse (taken on the radial artery at the wrist) is routinely used Varies with health, body position, and activity Measuring Blood Pressure Systemic arterial BP is measured indirectly with the auscultatory method 1.A sphygmomanometer (blood pressure cuff) is placed on the arm superior to the elbow 2.Pressure is increased in the cuff until it is greater than systolic pressure in the brachial artery 3.Pressure is released slowly and the examiner listens with a stethoscope 4.The first sound heard is recorded as the systolic pressure 5.The pressure when sound disappears is recorded as the diastolic pressure Blood Flow Through Tissues Blood flow, or tissue perfusion, is involved in: Delivery of oxygen and nutrients to, and removal of wastes from, tissue cells Gas exchange in the lungs Absorption of nutrients from the digestive tract Urine formation by the kidneys Blood flow is precisely the right amount to provide proper tissue function Velocity of Blood Flow Blood velocity: Changes as it travels through the systemic circulation Is inversely proportional to the cross-sectional area Slow capillary flow allows adequate time for exchange between blood and tissues Blood Vessels Blood is carried in a closed system of vessels that begins and ends at the heart The three major types of vessels are arteries, capillaries, and veins Arteries carry blood away from the heart, veins carry blood toward the heart Capillaries contact tissue cells and directly serve cellular needs Blood Vessels Structure Endothelium, Smooth Muscle & Connective Tissue • • • Arteries – have thicker walls protect against blood pressure that are necessary for blood flow – Increased smooth muscle for more control Capillaries – Very thin(only endothelium) best for exchange – Susceptible to higher pressures – Allow only a single RBC to pass at a time – There are three structural types of capillaries: continuous, fenestrated, and sinusoids Veins – Flexible walls: can store blood – Low pressure, muscles milk for return flow Regulation of Blood Pressure • Blood pressure is determined by cardiac output and peripheral resistance due to constriction of arterioles • Vasoconstriction is the contraction of smooth muscle in arteriole walls; it increases blood pressure • Vasodilation is the relaxation of smooth muscles in the arterioles; it causes blood pressure to fall Regulation of blood flow / microcirculation (capillaries) = tissue perfusion • Two mechanisms regulate distribution of blood in capillary beds: – Contraction of the smooth muscle layer in the wall of an arteriole constricts the vessel – Precapillary sphincters control flow of blood between arterioles and venules Terminal arteriole Precapillary sphincters Postcapillary venule Regulation of Blood Flow and Pressure • Heart – Neural: Autonomic Nervous sytstem, ANS • Parasympathetic – Acetylcholine – decreases H.R. • Sympathetic – norepinephrine – increases H.R. & Strength – Hormonal • Epindephrine (adrenal medulla) increase H.R. & Strength • Blood Vessels – Neural – sympathetic (norepindephrine) • Vasoconstriction or vasodilation At Capillaries Diffusion is sufficient Net outward flow Fluid Return by the Lymphatic System • The lymphatic system returns fluid that leaks out in the capillary beds • This system aids in body defense • Fluid, called lymph, reenters the circulation directly at the venous end of the capillary bed and indirectly through the lymphatic system • The lymphatic system drains into veins in the neck Circulatory Systems • While diffusion gets nutrients into and out of the blood. Transport system for mass blood movement (circulation) is required to connect organs • In small and/or thin animals, cells can exchange materials directly with the surrounding medium • Most complex animals have internal transport systems that circulate fluid Diffusion Rates Distance (µm) 1 0.5 msec 10 50 msec 100 5 seconds 1,000 (1mm) 8.3 minutes 10,000 (1cm) 14 hours Open and Closed Circulatory Systems • • More complex animals have either open or closed circulatory systems Both systems have three basic components: – A circulatory fluid (blood or hemolymph) – A set of tubes (blood vessels) – A muscular pump (the heart) Both need to come near surface of body for nutrient exchange Open Circulatory system: (insects, mollusks & arthropods) • hemolymph = general body fluid (blood and interstitial fluid combined) • bathes the organs a) Hemolymph is pumped out through open-ended vessels & flows out among the cells b) muscle contractions move hemolymph toward tail & around when the heart relaxes the fluid returns through several pores Time required Closed Circulatory system vertebrates, earthworms, octopus • blood confined to vessels - cardiovascular system • heart pumps the blood through larger vessels (arteries) to smaller ones (capillaries) then back through larger vessels (veins) again to heart Single Circulation • Vertebrate hearts contain two or more chambers • Blood enters atrium and is pumped out through a ventricle single circulation with a two-chambered heart • blood leaving the heart passes through two capillary beds before returning Double Circulation • Amphibian, reptiles, and mammals • Oxygen-poor and oxygen-rich blood are pumped separately from the right and left sides of the heart