* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download CHAPTER 17: DIGESTIVE SYSTEM
Survey
Document related concepts
Transcript
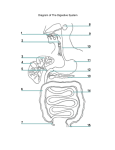
UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM LEARNING OUTCOMES: 17.1 17.2 17.3 Introduction 1. Describe the general functions of the digestive system. 2. Name the major organs of the digestive system. General Characteristics of the Alimentary Canal 3. Describe the structure of the wall of the alimentary canal. 4. Explain how the contents of the alimentary canal are mixed and moved. Mouth 5. Describe the functions of the structures associated with the mouth. 6. Describe how different types of teeth are adapted for different functions, and list the parts of a tooth. 17.4 - 17.10. Salivary Glands – Large Intestine 7. Locate each of the organs and glands; then describe the general function of each. 8. Identify the function of each enzyme secreted by the digestive organs and glands. 9. Describe how digestive secretions are regulated. 10. Explain control of movement of material through the alimentary canal. 11. Describe the mechanisms of swallowing, vomiting, and defecating. 12. Explain how the products of digestion are absorbed. 17.11 Life-Span Changes 13. Describe aging-related changes in the digestive system. 17-1 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.1 INTRODUCTION A. Definition: Digestion The process by which food substances are changed into forms that can be absorbed through cell membranes. B. Digestive Processes: 1. 2. 3. 4. 5. C. Ingestion = taking food into the mouth. Movement of Food = the passage of food along the gastrointestinal (GI) tract. Digestion = the breakdown of food by chemical and mechanical means. Absorption = the passage of digested food from GI tract into bloodstream (and lymph) for distribution to cells. Defecation = the elimination of undigested material from GI tract. Digestive Organs See Fig 17.1, page 650. 1. Two categories: a. Alimentary canal (GI Tract), which extends from mouth to anus. o Organs include: See Fig 17.2, page 651. 1. 2. 3. 4. 5. 6. b. mouth pharynx esophagus stomach small intestine large intestine Accessory organs release secretions into the alimentary canal that help digest food: o Organs include: 1. salivary glands 2. liver 3. gallbladder 4. pancreas 17-2 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.2 GENERAL CHARACTERISTICS OF THE ALIMENTARY CANAL A. Structure of the Wall There are Four Distinct Layers of the wall. See Fig 17.3 and Table 17.1, page 652. 1. Mucosa = innermost (surrounds lumen) a. b. c. d. composed of epithelium + CT (areolar) and small amounts of smooth muscle Epithelium extends into lumen = villi (increases surface area). contains many glands that secrete mucus (lubrication & protection from harmful action of digestive enzymes) functions: o o o 2. Submucosa = beneath mucosa a. b. composed of areolar CT, blood vessels, lymph vessels, and nerves functions: o o 3. nourishment of mucosa carrying absorbed nutrients away Muscularis = two layers of muscle a. b. c. 4. protection secretion absorption (of nutrients) circular muscle layer around submucosa longitudinal layer around circular layer function: movements of food through canal (mixing & peristalsis) Serosa = outermost layer a. visceral peritoneum b. functions: o lubrication o free movement of canal in abdominal cavity c. Intestinal peritoneal extensions = mesentery. o suspend the length of the intestine within abdominal cavity 17-3 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.2 GENERAL CHARACTERISTICS OF THE ALIMENTARY CANAL B. Movements of the Tube See Figure 17.4, page 653. 1. Mixing: (mechanical digestion) a. b. c. 2. food + digestive juices + mucus circular muscle layer segmentation occurs in small intestine Peristalsis: a. b. c. d. accomplished by movements of longitudinal muscle layer propelling action As food passes, one section of tube relaxes (receptive relaxation), opening next section and food moves on. Sphincter Muscles play an important role in movements throughout the GI tract also. 1. 2. C. Definition: Sphincter = a strong circular muscle which prevents regurgitation of food. Locations: between (regions) organs of digestive tract. a. esophagus and stomach o gastroesophageal sphincter b. stomach and small intestine o pyloric sphincter c. small and large intestine o ileocecal valve d. large intestine to outside o internal anal sphincter o external anal sphincter Innervation of the Tube 1. Autonomic Nervous System a. Parasympathetic – activates digestion b. Sympathetic – slows digestion 2. Post-ganglionic networks a. Submucosal plexus controls secretions. b. Myenteric plexus controls peristalsis. 17-4 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.3 MOUTH A. Introduction: 1. 2. B. The terms oral cavity and buccal cavity refer to the mouth. The mouth is adapted to receive food and start mechanical and chemical digestion by chewing and mixing food with saliva. The mouth is surrounded by cheeks, lips, tongue and palate: 1. Cheeks and Lips a. b. c. 2. Tongue a. b. c. d. e. 3. Cheeks form the lateral walls of mouth. Lips surround the opening of mouth; important in monitoring food temperature. See Fig 17.5, page 653. muscular (skeletal) organ on floor of mouth important in mixing food (mechanical digestion) and swallowing contains many bumps called papillae, which house taste buds posterior root contains lymphatic tissue called the lingual tonsil See Figure 17.6, page 654. Palate = roof of mouth. a. b. c. d. Anterior portion = hard palate. Posterior portion = soft palate. Median extension of soft palate = uvula. tonsils: 1. Palatine tonsils = masses of lymphatic tissue lateral to palate. * Tonsillitis = inflammation of palatine tonsils. See box on page 654. 2. e. D. Pharyngeal tonsils = adenoids lymphatic tissue on posterior pharynx See Figure 17.5, page 653, and Fig 17.7, page 655. composed of 2 chambers: a. b. Oral cavity proper = chamber that extends from teeth/gums to pharynx. Vestibule = narrow space between teeth, cheeks and lips. 17-5 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.3 MOUTH E. Teeth: 1. 2. 3. two sets of dentitions: See Fig 17.8, page 655, and Fig 17.9 and Table 17.2, page 656. a. deciduous teeth 1. number 20 2. erupt from 6 - 32 months 3. lost between 6 - 12 years b. permanent (secondary) teeth 1. number 32 2. erupt from 6 yrs - adulthood 3. See Fig 17.9, page 656. function: to break food into smaller pieces. (mechanical digestion) a. increasing surface area of food b. increasing effectiveness of digestive enzymes 4 types with different functions: See Fig 17.9, page 656. a. Incisors = front teeth. break food into bite-size pieces b. Cuspids = canine (eye) teeth. grasps and tears food c. Bicuspids = grinding food particles. d. Molars = grinding food particles. See box on page 658 re: stem cells and replacement teeth. 4. Tooth Structure: Teeth are located in alveolar processes of maxilla and mandible. See Fig 17.10, page 656. a. b. c. d. Crown = exposed area of tooth. Root = area below gum (gingiva). Enamel =covering on crown Ca2+ salts hardest substance in body. Dentin = bulk of tooth. * See Clinical Application 17.1, page 657 re: Dental Caries. * See Table 17.3, page 657, Parts of the Mouth. 17-6 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.4 SALIVARY GLANDS A. B. Introduction: 1. Salivary glands secrete saliva. 2. Saliva binds food together and begins chemical polysaccharides by the enzyme salivary amylase. digestion of Major Salivary Glands 1. parotid = largest lies over masseter, mostly serous cells 2. submandibular = floor of mouth lateral, mix of serous and mucous cells 3. sublingual = floor of mouth, medial, mostly mucous cells See Figure 17.11, page 659 and Table 17.4, page 658. C. Salivary Secretion Composition: 1. Each salivary gland is composed of 2 types of cells: a. Mucous cells secrete mucus b. Serous cells secrete watery substance containing the enzyme salivary amylase. See Fig 17.12, page 659. D. Salivary Secretion Functions: 1. provide lubrication 2. bind food together 3. begin chemical digestion of carbohydrates Enzyme = salivary amylase breaks polysaccharides into disaccharides. a. b. starch disaccharides glycogen disaccharides 17-7 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.5 PHARYNX AND ESOPHAGUS A. PHARYNX 1. 2. 3. throat passageway of food into esophagus (and air into larynx/trachea) Structure of the Pharynx: See Fig 17.7, page 655. nasopharynx – superior to soft palate, posterior to nasal cavity oropharynx – posterior to mouth down to epiglottis laryngopharynx – inferior to oropharynx from epiglottis to cricoid cartilage Muscles of the Pharynx Wall: See Fig 17.13, page 640. Swallowing Mechanism (deglutition): 3 stages See Figure 17.14, page 661. A. B. C. 4. 5. a. Stage 1 (voluntary): Chew food & mix with saliva into bolus at back of pharynx. b. Stage 2 (involuntary): Swallowing reflex triggered, c. B. o Epiglottis closes over larynx (no breathing). o Muscles in lower pharynx relax. o Esophagus opens and food moves in. Stage 3 (involuntary) Esophagus brings bolus to stomach by peristalsis. ESOPHAGUS See Fig 17.15 and Fig 17.16, page 662. 1. passageway for food from pharynx to stomach 2. Location: mediastinum behind trachea goes through diaphragm at esophageal hiatus a. See box on page 662 re: Hiatal hernia. 3. many mucous glands 4. Movement of food: A. gravity b. Peristaltic waves from esophagus meet sphincter muscle (cardiac sphincter). c. Gastro esophageal sphincter muscle relaxes. d. Food moves into stomach all at once. gastroesophageal 17-8 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.6 STOMACH: See Fig 17.18, page 663. A. B. Introduction: 1. The term gastric refers to the stomach. 2. The stomach functions to mix bolus into chyme and begin the chemical breakdown of proteins. Structure of Stomach: 1. Description = J-shaped, pouch-like organ. 2. contains extra oblique layer in muscularis 3. Location = under diaphragm left side. 4. Capacity = 1 liter. 5. Parts of the Stomach: a. b. c. d. 6. cardiac region - around esophagus fundic region - large ballooned area body – main portion pyloric region - near duodenum o The pyloric region narrows into pyloric canal. o The pyloric sphincter muscle lies between pylorus & duodenum. d. greater curvature e. lesser curvature f. body Mucosal Structure a. Note the macroscopic rugae (mucosal folds) in Fig 17.17b, page 663. b. Microscopically, these rugae are formed by: See Fig 17.19, page 664. o Gastric villi that project into the lumen which result in the formation of… o Gastric pits that are located between the gastric villi. 1. Gastric glands are located along these gastric pits. a. C. Gastric juice is secreted by these gastric glands. Functions of Stomach: 1. mechanical digestion – churning 2. chemical digestion of proteins – gastric juice 17-9 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.6 STOMACH D. Gastric Secretions (Juice): See Table 17.5, page 665. 1. composed of: a. mucus ○ Function: lubrication, protection of mucosa from digestion b. digestive enzyme pepsin ○ Function: protein digestion (into peptides) c. hydrochloric acid (HCl) ○ Functions: 1. denatures proteins 2. kills microbes in food d. intrinsic factor ○ Function: aids absorption of Vitamin B12 needed for erythropoiesis e. gastrin Function: regulatory hormone 2. Four types of gastric cells in Gastric Glands: a. b. c. d. E. Mucous cells secrete mucus. Chief cells secrete pepsin. Parietal cells secrete HCl & intrinsic factor. G-cells secrete gastrin. Regulation of Gastric Secretions: See Fig 17.20, page 665 and Table 17.6, page 666. 1. Neural a. parasympathetic – increases gastric secretion b. sympathetic – decreases gastric secretion 2. Hormonal a. Gastrin – increases gastric secretion b. Somatostatin – decrease acid secretion from parietal cells c. Cholecystokinin – decreases gastric motility 17-10 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.6 STOMACH E. Regulation of Gastric Secretions: 3. Three phases of Gastric Secretion a. Cephalic Phase (30-50% of control) ○ increased parasympathetic due to sight, taste, smell, and thought of food b. Gastric Phase (40-50% of control) ○ Stretch of stomach wall increases gastrin secretion, which increases gastric secretions. ○ pH changes alter gastrin release. Food enters stomach, increasing pH. The reflexive increase in gastrin lowers pH. When pH lowers to 1.5 gastrin release ceases. ○ HCl released from parietal cells comes from blood. Blood pH needs to maintain 7.4. Parietal cells release bicarbonate to blood. This is called the alkaline tide. c. Intestinal Phase (5% of control) ○ Initially releases intestinal gastrin which increases gastric secretions. ○ As duodenum fills, a sympathetic reflex inhibits gastric release. ○ Proteins and fats in duodenum stimulate cholecystokinin release which decreases gastric motility. F. Gastric Absorption = Minimal (5%); includes some salts, water, lipid-soluble drugs, and alcohol G. Mixing and Emptying Actions See Fig 17.21, page 667, and Fig 17.22, page 668. 1. Mixing of bolus of food + gastric juice = chyme. 2. Peristaltic waves of stomach push chyme toward pyloric sphincter; it relaxes and food moves into duodenum a little at a time!!! ○ See box on page 664 re: hypertrophic pyloric stenosis. 3. Enterogastric reflex – ensures stomach slows down as duodenum fills. 4. Vomiting may occur to quickly remove toxins. * * See Clinical Application 7.2, A Common Problem: Stomachache, page 667. See box on page 665 re: Helicobacter pylori and gastritis and peptic ulcers. 17-11 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.7 PANCREAS A. Location: B. Inferior to stomach; retroperitoneal See Fig 17.23, page 669. Structure of the Pancreas 1. Shrimp–like with head in concave curve of duodenum; Tail extends to the left to the spleen. 2. Endocrine cells (alpha and beta cells of Islets of Langerhans) produce hormones glucagon and insulin, respectively. See Chapter 13. 3. Most cells make up pancreatic acini, which produce pancreatic juice. a. 4. C. Secretes pancreatic juice into a pancreatic duct; Pancreatic duct leads to duodenum (small intestine). Pancreatic duct joins bile duct at the Hepatopancreatic ampulla (ampulla of Vater) before passing through the Hepatopancreatic sphincter (sphincter of Oddi) to enter duodenum. Pancreatic Juice: Pancreatic juice contains four classes of enzymes that break down the four ingested organic macromolecules. 1. Carbohydrates (Starch and Glycogen) a. 2. Fats/Triglycerides a. 3. * Proteinases, trypsin, chymotrypsin, and carboxypeptidase proteins → peptides o These enzymes are stored and released as inactive form in zymogen granules. o Trypsinogen is activated to trypsin by enterokinase. o Trypsin then activates chymotrypsin and carboxypeptidase. Nucleic Acids a. * pancreatic lipase → 2 fatty acids + monoglyceride Proteins a. 4. pancreatic amylase → disaccharides nucleases nucleotides Note bicarbonate ions are also released to neutralize acidic chyme entering from the stomach. See box on page 668 re: acute pancreatitis. 17-12 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.7 PANCREAS D. Regulation of Pancreatic Secretions: See Fig 17.24, page 670. 1. 2. Hormones secretin and cholecystokinin regulate pancreatic secretions. Secretin Activation: a. b. c. 3. Cholecystokinin Activation: a. b. c. 17.8 When duodenum fills with acidic chyme, secretin is released from the intestinal wall. Secretin stimulates the release of bicarbonate rich pancreatic juice into duodenum. Once acid is neutralized, proteins and fats signal cholecystokinin release from the intestinal wall. CCK stimulates the release of enzyme rich pancreatic juice into the duodenum. LIVER A. Introduction: The term hepatic refers to the liver. The liver has many functions; however its digestive function is emulsification of fats. B. Location/Description: See Fig 17.25, page 670 and Fig 17.26, page 671. 1. below diaphragm 2. right side 3. largest internal organ C. Liver Structure: 1. 4 lobes: a. b. c. Fig 17.26, page 671. large right & small left quadrate and caudate lobe in posterior region each lobe is made up of: o Hepatic lobules = functional unit of the liver. See Fig 17.27, page 671. 1. hexagon shaped around a central vein 2. contains hepatocytes which provide most functions 3. also contains Kupffer’s cells (macrophages) See Fig 17.28, page 672. a. remove and destroy: microbes foreign matter worn platelets and erythrocytes 17-13 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.8 LIVER D. E. Liver Functions: 1. 2. 3. 4. 5. metabolism of monosaccharides, lipoproteins, and amino acids storage (glycogen, Vitamin A, B12, D, iron) filtering of blood (worn blood cells and debris) destruction of toxic chemicals (alcohol and drugs) production/secretion of bile * See Table 17.7, page 673 for more specifics on liver functions. Blood Supply to Liver: See Figure 17.28, page 672. 1. 2. 3. from 2 sources: a. hepatic artery supplies oxygenated blood b. hepatic portal vein supplies deoxygenated blood filled with: ○ newly absorbed nutrients from small intestine ○ toxins from stomach ○ worn blood cells from spleen Blood enters the liver sinusoids where hepatocytes remove the following: a. oxygen b. nutrients (stored or used to make new materials) c. poisons (detoxified) d. worn cells and debris (phagocytosis). Blood leaving the liver cells (deoxygenated plus liver secretions) drains into central veins, which come together and leave the liver as the hepatic vein. 17-14 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.8 LIVER E. Blood Supply to Liver: See Figure 17.28, page 672. 4. Overall scheme of Liver Blood Flow: Hepatic Artery (Oxygenated Blood) from aorta) Hepatic Portal Vein (Deoxygenated Blood with newly absorbed nutrients from small intestine, etc.) Liver Sinusoids (Exchange) Central Vein of Hepatic Lobule Hepatic Vein Inferior Vena Cava F. Composition of Bile Bile is composed of: 1. 2. 3. 4. bile salts (digestive function) bile pigments (biliverdin and bilirubin) a. breakdown products of hemoglobin cholesterol electrolytes * See box on page 672 re: hepatic coma. * See from Science to Technology 17.1, page 673, Replacing the Liver. * See Clinical Application 17.3, page 674, Hepatitis. * See box on page 673 re: jaundice. 17-15 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.8 LIVER G. Gall Bladder See Fig 17.26, page 671, and Fig 17.29, page 674. 1. stores bile between meals 2. Location: 3. Bile can flow to small intestine by either of 2 routes: the liver or gall bladder (see below) 4. Bile secretion, storage, flow: underside of liver, connected via cystic duct From liver: From Gall Bladder: Common Hepatic duct Cystic Duct COMMON * BILE DUCT Duodenum * * 5. Hepatopancreatic sphincter muscle usually keeps common bile duct closed. See Clinical Application 17.4, page 675, Gallbladder Disease. Regulation of Bile Release See Fig 17.30, page 675. a. Hormone = CHOLECYSTOKININ (CCK) b. When small intestine fills with fatty chyme: o o o o c. cholecystokinin is released into blood. CCK stimulates walls of gallbladder to contract. Bile passes down into cystic duct and common bile duct. Hepatopancreatic sphincter in common bile duct opens and bile is deposited into duodenum. Functions of Bile Salts: Emulsification of fat molecules! o Emulsification = breaking up of fat globules into small droplets (increases surface area and increases effectiveness of lipases). o Bile is released into duodenum to emulsify fat. o Bile also aids in absorption of fats and fat-soluble vitamins. 17-16 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.9 SMALL INTESTINE A. Parts of Small Intestine: 1. 2. 3. duodenum - nearest stomach jejunum - mid-region ileum - near large intestine. a. b. c. B. C. See Fig 17.31, page 676. The distal end of the ileum narrows to form the ileocecal valve (sphincter muscle between small & large intestine). Jejunum and ilium are attached to the posterior abdominal wall by folds in peritoneum called mesentery. See Figure 17.33, page 677. Functions of Small Intestine 1. Major site of chemical digestion (duodenum) a. bile deposition b. pancreatic juice deposition c. small intestinal digestive enzymes 2. Secretions a. mucus b. digestive enzymes 3. Major site of ABSORPTION of Nutrients a. about 90% of all b. through the proximal mucosa Structure of the Small Intestine Wall See Fig 17.35 and Fig 17.36, page 678. 1. Intestinal villi project into lumen (increasing surface area). 2. Each villus is composed of simple columnar epithelium, with microvilli (further increasing surface area; See Figure 17.37, page 679) and connective tissue with many blood & lymphatic vessels (lacteals). 3. Absorbed nutrients are carried away by blood & lacteals. 4. Intestinal glands are located between villi and further increase surface area (SA). 5. Submucosal folds called plicae circulares also further increase SA; See Figure 17.38, page 679. 6. * Muscularis and serosa are typical. See box on page 678 re: small intestine muscosal turnover. 17-17 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.9 SMALL INTESTINE D. Secretions of Small Intestine 1. 2. mucus (from Brunner’s glands in submucosa and goblet cells) digestive enzymes: a. peptidases peptides amino acids b. sucrase, maltase, lactase disaccharides monosaccharides * See box on page 680 re: lactose intolerance. c. intestinal lipases triglycerides * 3 fatty acids + glycerol See Table 17.9, page 680 for Summary of Major Digestive Enzymes. E. Regulation of Small Intestinal Secretions 1. Mechanical and chemical stimulation of duodenal wall by entering chyme regulates intestinal secretions. F. Absorption in Small Intestine (90% of total) Fig 17.42, page 682. 1. Intestinal villi and microvilli (See Fig 17.37, page 679) increase absorptive surface area. 2. Simplest forms of ingested food molecules are absorbed into the intestinal mucosa: a. monosaccharides 1. by facilitated diffusion or active transport 2. carried away by submucosal blood capillaries b. amino acids 1. active transport 2. carried away by blood capillaries c. fatty acids 1. by simple diffusion into intestinal mucosa 2. Fatty acids are used to synthesize endoplasmic reticulum “ER”. 2. Once in mucosal cells’ ER, the fats collect in clusters encased in protein to form chylomicrons (lipoproteins). 3. Chylomicrons are absorbed by lacteals (lymphatic capillaries) into the lymphatic system. d. Ions and water are also absorbed. * See box on page 682 re: Malabsorption. 17-18 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.9 SMALL INTESTINE G. Movements of the Small Intestine 1. mixing of chyme + intestinal juices by segmentation (mechanical digestion) 2. Peristaltic waves push residual chyme toward ileocecal sphincter; It relaxes, moving food into large intestine. * Irritation or over distension may cause peristaltic rush which is rapid emptying of small intestine resulting in diarrhea. 17.10 LARGE INTESTINE A. Parts of Large Intestine: See Fig 17.43, page 684. 1. 2. 3. 4. B. Colon is divided into four (4) portions: 1. 2. 3. 4. C. ascending colon - from cecum to liver (right) transverse colon - runs across top of abdomen descending colon - from spleen downward (left) sigmoid colon - S-shaped portion, which becomes rectum Structure of the Large Intestinal Wall 1. 2. 3. 4. 5. D. cecum - nearest ileum of small intestine; Appendix is a blind pouch in this region. * See box on page 683 re: appendicitis. colon - majority of length rectum - distal region of colon * See box on page 683 re: hemorrhoids. anal canal - narrowing of rectum and opening to outside relatively same as typical wall; See page 652. lacks villi Longitudinal muscularis layer forms 3 bands called teniae coli. Pouches or haustra develop due to the tension of the teniae coli. Serosa may have fatty extensions called epiploic appendages. Functions of Large Intestine: 1. 2. 3. 4. Secretion = mucus. Absorption = water & electrolytes. Storage = feces. Minimal digestion by intestinal flora (bacteria) which digest substances humans cannot digest. 17-19 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.10 LARGE INTESTINE E. Movements of the Large Intestine: 1. mass movements only 2-3 times a day a. F. Control of Anal Sphincter Muscles: 1. G. Peristaltic waves of large intestine move residual chyme toward anal sphincter muscles. both voluntary & involuntary nervous control Feces: 1. undigested & unabsorbed material 2. color due to bile pigments 3. odor due to intestinal bacteria and bacterial products formed in digestion 4. 75% water * See box on page 686 explaining sources of intestinal gas. H. Defecation = emptying of rectum. * See box on page 686 re: Hirschsprung Disease. * See Clinical Application 17.5 page 687, Disorders of the Large Intestine. 17-20 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM DIGESTIVE SYSTEM SUMMARY TABLE I (keyed at the end of this outline) NAME OF DIGESTIVE ORGAN ALIMENTARY CANAL OR ACCESSORY? DESCRIPTION OF STRUCTURE SECRETIONS DIGESTIVE FUNCTION HORMONAL CONTROL OF SECRETIONS? 17-21 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM DIGESTIVE SYSTEM SUMMARY TABLE I (CONTINUED) NAME OF DIGESTIVE ORGAN ALIMENTARY CANAL OR ACCESSORY? DESCRIPTION OF STRUCTURE SECRETIONS DIGESTIVE FUNCTION HORMONAL CONTROL OF SECRETIONS? 17-22 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM DIGESTIVE SYSTEM SUMMARY TABLE I (CONTINUED) NAME OF DIGESTIVE ORGAN ALIMENTARY CANAL OR ACCESSORY? DESCRIPTION OF STRUCTURE SECRETIONS DIGESTIVE FUNCTION HORMONAL CONTROL OF SECRETIONS? 17-23 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM DIGESTIVE SYSTEM SUMMARY TABLE I (CONTINUED) NAME OF DIGESTIVE ORGAN ALIMENTARY CANAL OR ACCESSORY? DESCRIPTION OF STRUCTURE SECRETIONS DIGESTIVE FUNCTION HORMONAL CONTROL OF SECRETIONS? 17-24 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM DIGESTIVE SYSTEM SUMMARY TABLE II (Keyed at the end of this outline) MACROMOLECULE INGESTED SITE OF DIGESTION DIGESTIVE ENZYME(S) ENDPRODUCT(S) SITE AND MODE OF ABSORPTION ABSORBED INTO BLOOD OR LYMPH REGULATION 17-25 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM 17.11 LIFE SPAN CHANGES A. Mouth changes that occur with age reduce chewing ability. 1. Enamel thins increasing sensitivity to hot and cold. 2. Gums recede. 3. Teeth loosen. B. Slowing peristalsis causes: 1. heartburn 2. constipation C. Absorption of nutrients decreases with age. OTHER INTERESTING TOPICS: A. B. C. The Gut Microbiome. See Introduction on page 649. GI Camera. See box on page 651. Cheek cells used to provide DNA for genetic testing. See box on page 654. INNERCONNECTIONS OF THE DIGESTIVE SYSTEM - See page 689. CHAPTER SUMMARY – see pages 688, 690-692. CHAPTER ASSESSMENTS – see pages 692-693. INTEGRATIVE ASSESSMENTS/ CRITICAL THINKING – see page 693. 17-26 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM DIGESTIVE SYSTEM SUMMARY TABLE I: NAME OF DIGESTIVE ORGAN MOUTH SALIVARY GLANDS PHARYNX ALIMENTARY CANAL OR ACCESSORY? ALIMENTARY CANAL ACCESSORY ALIMENTARY CANAL DESCRIPTION OF STRUCTURE SEE OUTLINE SEE OUTLINE SEE OUTLINE SECRETIONS MUCUS SALIVA WITH AMYLASE MUCUS DIGESTIVE FUNCTION MECHANICAL BREAKDOWN OF STARCH AND GLYCOGEN TO DISACCHARIDES NONE HORMONAL CONTROL OF SECRETIONS? N/A N/A N/A 17-27 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM DIGESTIVE SYSTEM SUMMARY TABLE I: NAME OF DIGESTIVE ORGAN ESOPHAGUS STOMACH (GASTRIC) LIVER ALIMENTARY CANAL OR ACCESSORY? ALIMENTARY CANAL ALIMENTARY CANAL ACCESSORY DESCRIPTION OF STRUCTURE SEE OUTLINE SEE OUTLINE SEE OUTLINE MUCUS PEPSIN SECRETIONS MUCUS HYDROCHLORIC ACID BILE INTRINSIC FACTOR GASTRIN DIGESTIVE FUNCTION NONE PEPSIN BREAKS PROTEINS INTO PEPTIDES EMULSIFICATION OF FATS HCl DENATURES THE PROTEINS HORMONAL CONTROL OF SECRETIONS? N/A GASTRIN SECRETED BY GCELLS PROMOTES RELEASE OF GASTRIC JUICE, ETC. CHOLECYTOKININ (CCK) OPENS COMMON BILE DUCT WHEN FATTY CHYME FILLS DUODENUM 17-28 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM DIGESTIVE SYSTEM SUMMARY TABLE I: NAME OF DIGESTIVE ORGAN GALL BLADDER PANCREAS SMALL INTESTINE ALIMENTARY CANAL OR ACCESSORY? ACCESSORY ACCESSORY ALIMENTARY CANAL DESCRIPTION OF STRUCTURE SEE OUTLINE SEE OUTLINE SEE OUTLINE AMYLASE PEPTIDASES PROTEASES (PROTEINASES) SUCRASE, MALTASE, LACTASE SECRETIONS STORED BILE PRODUCED IN LIVER LIPASES NUCLEASES DIGESTIVE FUNCTION HORMONAL CONTROL OF SECRETIONS? EMULSIFICATION OF FATS CCK CAUSES CONRTACTION OF GALLBALLDER AND OPENS COMMON BILE DUCT WHEN FATTY CHYME FILLS DUODENUM LIPASES AMYLASE: STARCH AND GLYCOGEN TO DISACCHS. PROTEASES: PROTEINS TO PEPTIDES. LIPASES: TRIGLYCERIDES TO FATTY ACIDS & MONOGLYCERIDES. NUCLEASES: NUCLEIC ACIDS TO NUCLEOTIDES. PEPTIDASES: PEPTIDES TO AMINO ACIDS. SUCRASE, MALTASE, LACTASE: DISACCHARIDES TO MONOSACCHARIDES. LIPASES: TG TO FATTY ACIDS AND GLYCEROL. SECRETIN CAUSES PANCREATIC JUICE TO BE DEPOSITED INTO DUODENUM N/A 17-29 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM DIGESTIVE SYSTEM SUMMARY TABLE I NAME OF DIGESTIVE ORGAN LARGE INTESTINE ALIMENTARY CANAL OR ACCESSORY? ALIMENTARY CANAL DESCRIPTION OF STRUCTURE SEE OUTLINE SECRETIONS MUCUS DIGESTIVE FUNCTION REABSORPTION OF WATER AND ELECTROLYTES FROM CHYME HORMONAL CONTROL OF SECRETIONS? N/A 17-30 UNIT 5 - CHAPTER 17: DIGESTIVE SYSTEM DIGESTIVE SYSTEM SUMMARY TABLE II MACROMOLECULE INGESTED CARBOHYDRATES PROTEINS FATS (TRIGLYCERIDES OR TG) NUCLEIC ACIDS SITE OF DIGESTION 1.MOUTH 2.DUODENUM 3.DUODENUM 1.STOMACH 2.DUODENUM 3.DUODENUM 1. DUODENUM 2. DUODENUM DUODENUM DIGESTIVE ENZYME(S) 1. SALIVARY AMYLASE 2. PANC. AMYLASE 3. SUCRASE, LACTASE, MALTASE 1.PEPSIN *HCl 2. PANCREATIC PROTEASES 3. PEPTIDASES 1. PANCREATIC LIPASES *BILE 2. DUODENAL LIPASES *BILE PANCREATIC NUCLEASES END-PRODUCT (S) 1 & 2. STARCH AND GLYCOGEN TO DISACCHARIDES HCl DENATURES PROTEINS 1 & 2. PROTEINS TO PEPTIDES 3. PEPTIDES TO AMINO ACIDS BILE EMULSIFIES TG’S. PANCREATIC LIPASES BREAK TG’S INTO FATTY ACIDS & MONOGLYCERIDES; DUODENAL LIPASES BREAK TG’S INTO FATTY ACIDS & GLYCEROL NUCLEOTIDES 3. DISACCHARIDES TO MONOSACCHARIDES SITE AND MODE OF ABSORP-TION DISTAL SM. INTESTINE FACILITATED DIFFUSION DISTAL SM. INTESTINE ACTIVE TRANSPORT DISTAL SM. INTESTINE SIMPLE DIFFUSION DISTAL SM. INTESTINE ABSORBED INTO BLOOD OR LYMPH BLOOD BLOOD LYMPH BY LACTEAL BLOOD REGULATION SECRETIN FOR PANC. AMYLASE GASTRIN FOR PEPSIN CCK FOR BILE SECRETIN FOR PANC. LIPASES SECRETIN FOR PANC. NUCLEASES 17-31