* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Pertussis
Sarcocystis wikipedia , lookup
Meningococcal disease wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Tuberculosis wikipedia , lookup
Marburg virus disease wikipedia , lookup
Hepatitis C wikipedia , lookup
Hepatitis B wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Cryptosporidiosis wikipedia , lookup
Schistosomiasis wikipedia , lookup
Gastroenteritis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Trichinosis wikipedia , lookup
Leptospirosis wikipedia , lookup
Neonatal infection wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
Lymphocytic choriomeningitis wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
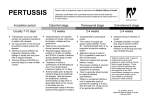
PERTUSSIS MEAGHAN MOLLARD DEFINITION • “Whooping cough” • Highly contagious, acute respiratory illness cause by Bordetella pertussis bacteria • Most commonly affects children <6 months of age who are not completely vaccinated and children 11-12 years as childhood vaccination coverage wears off • Inspiratory whoop • Paroxysmal cough • Post-tussive emesis (CDC, 2014) ETIOLOGY • B. pertussis is caused by gram negative pleomorphic bacillus • Pertussis is highly contagious infecting 80-90% of susceptible individuals that are exposed • 3 Species of Bordetella can affect respiratory tract • B. parapertussis, B. bronchiseptica, B. holmesii (Bocka, 2014) PATHOPHYSIOLOGY • Pertussis is primarily a toxin-mediated disease. • Bacteria attach to the cilia of the respiratory epithelial cells. • Bacteria produce toxins that paralyze the cilia causing inflammation of the respiratory tract. • Inflammation interferes with the clearing of pulmonary secretions. • Pulmonary secretions are described as a mucopurulosanguineous exudates. (Bocka, 2014) TRANSMISSION • Spread from person to person when coughing, sneezing, talking, and laughing while in close contact. • Inhalation of infected respiratory droplets. • Many infants and children who are not fully vaccinated are infected by older siblings, parents and caregivers. • Contagious from the onset of cold like symptoms through 3rd week, after paroxysmal coughing onset, or until after 5 days of effective antibiotic treatment. (CDC, 2014) INCUBATION • Incubation period can be as short as one week but as long as 3 weeks • Typically 7-10 days • Incubation period is longer than that of the common cold, which is about 1 to 3 days (Bocka, 2014) INCIDENCE • 48.5 million yearly cases world wide • 4,838 cases of pertussis reported from January 1, 2014 to April 14, 2014 • High infant mortality rate prior to whole cell vaccine in the 1940’s. • Cyclical epidemics every two to five years, present in the pre-vaccine era • Most cases occur in late summer and early fall • 5-10% of cases are recognized and reported • Most commonly reported vaccine-preventable disease in the United States in children younger than 5 years. (Bocka, 2014), (CDC, 2014) FIGURE 1: REPORTED CASES OF PERTUSSIS FROM 1922- 2013 (CDC, 2014) REDUCE THE RISK • Prevention: GET VACCINATED!!! • Recommendations for infants and children: • 5 doses of diphtheria, tetanus and pertussis (DTaP) vaccine given between 6 weeks and 7 years of age, usually at 2 months, 4 months, 6 months, between 15-18 months and 4-6 years. (CDC, 2014), (Cornia & Lipsky, 2014) REDUCE THE RISK • Vaccine recommendation for children >7 and adults: • Tdap given between 11-18 years old, preferred administration is between 11-12 years • Adults 19 and older who have not had Tdap vaccine need a booster shot • Tdap administered to pregnant individuals during each pregnancy between 27- 36 weeks gestation • Td every 10 years (CDC, 2014), (Cornia & Lipsky, 2014) RISK FACTORS • Young infants born prematurely • Patients with underlying cardiac, pulmonary, neuromuscular, or neurologic disease • Non-vaccinated individuals • Contact with an infected person • Epidemic exposure • Pregnancy (Cornia & Lipsky, 2014) SCREENING • Vaccination screening should be done routinely at primary care visits • Screen: • High risk individuals- infants, pregnant women, and non vaccinated children • OR • Individuals who have had cough >2 weeks CLINICAL FINDINGS • Incubation period 7-10 days after exposure to B. pertussis • Followed by the onset of nonspecific symptoms • Total duration of pertussis is about 3 months • “The cough of 100 days.” • 3 stages of Pertussis: • Catarrhal • Paroxysmal • Convalescent (Yeh & Mink, 2014), (CDC, 2014) CLINICAL FINDINGS- CATARRHAL • Lasts 1-2 weeks • Pertussis most infectious during catarrhal phase • Indistinguishable from common upper respiratory infections • • • • • • • Nasal Congestions Rhinorrhea Sneezing Occasional low grade fever Occasional cough Red, watery eyes Apnea in infants (Yeh & Mink, 2014), (CDC, 2014) CLINICAL FINDINGS- PAROXYSMAL • • • • • Stage lasts 2 to 6 weeks Paroxysmal attacks Characteristic “Whoop” Posttussive emesis Extreme fatigue (Yeh & Mink, 2014), (CDC, 2014) CLINICAL FINDINGS- CONVALESCENT • 3rd and final stage, lasts 1-2 weeks • Gradual reduction in the frequency and severity of cough • Cough usually disappears after 2-3 weeks • Coughing symptoms can reappear with subsequent upper respiratory infections during the convalescence phase (Yeh & Mink, 2014), (CDC, 2014) DIFFERENTIAL DIAGNOSIS • • • • Mycoplasma pneumoniae Chlamydia pneumoniae Adenoviruses Respiratory syncytial virus infection • (Bocka, 2014) DIFFERENTIAL DIAGNOSIS • • • • • • • • • Common cold Influenza Interstitial pneumonitis Bronchiolitis Croup Dehydration Aspiration pneumonia Bacterial pneumonia Viral pneumonia • • • • • Febrile Seizures Fever Gastroenteritis Tachycardia Tuberculosis (Bocka, 2014) SOCIAL/ENVIRONMENTAL CONSIDERATIONS • Social: • Get vaccinated • High risk patients like infants and immuno-compromised individuals should avoid potential exposure • Drink plenty of fluids • Adequate rest Environmental: • Be aware of stimuli that can trigger coughing fits, ie: laughing, talking • Keep air clean and free from triggers, ie: tobacco smoke DIAGNOSIS • Detailed history • potential exposure to pertussis from infected individuals • common signs and symptoms associated with pertussis • Duration of symptoms • Physical exam • Rule out other potential causes of signs and symptoms • Most common physical findings include: • • conjunctival hemorrhage facial petechiae (Bocka, 2014) LABORATORY TESTS • • • • Nasopharyngeal culture PCR and Elisa Serology Testing CBC trend • The CDC recommends a combination of a culture and PCR assay if a patient has a cough lasting longer than 3 weeks. (CDC, 2014) MANAGEMENT • Goals of treatment • Limit the number of paroxysms • Maximize nutrition, rest, and recovery • Practice good hand hygiene to prevent the spread of respiratory illnesses TREATMENT • Starting treatment within first 1-2 weeks of symptom onset before paroxysmal cough starts might decrease the severity of symptoms. (Bocka, 2014) • CDC suggests treating prior to test results if clinical history strongly suggestive or if high risk patient, ie: infants. (CDC, 2014) • If patient diagnosed late, ABX will not change course of illness and should only be treated with an ABX if still contagious. (Bocka, 2014) TREATMENT • Treatment indications: • Antimicrobial tx with B.Pertussis isolated from culture or + PCR • Patient with a clinical diagnosis who has had symptoms for less than 21 days • Antimicrobial therapy for pt.’s who have >21 days of symptoms, especially those in contact with high risk individuals. • The Committee on Infectious Diseases (COID) of the American Academy of Pediatrics (Red Book Committee) recommends treating household members of infected individuals to limit secondary infection. (CDC, 2014) PHARMACOLOGICAL MANAGEMENT Antimicrobial agents and antibiotics help to eradicate B pertussis and prevent spreading Macrolides: Erythromycin, Azithromycin, Clarithromycin • Azithromycin preferred for infants <1 month • Erythromycin administered for 14 days • Azithromycin administered for 5 days • Clarithromycin administered for 7 days Trimethoprim-sulfamethoxazole alternative agent for persons >2months who can not tolerate macrolides • Bactrim is administered for 14 days (Yeh, 2014), (CDC, 2014), (Bocka, 2014) NON-PHARMACOLOGICAL • • • • • • Rest Drink plenty of fluids Eat smaller, more frequent meals Vaporize the room Keep the air clean Prevent transmission (CDC, 2014) COMPLICATIONS • Related the infection: • Pneumonia • Otitis Media • Reintroduction of paroxysmal coughing with upper respiratory infections • Sequelae of severe cough: • • • • • • • • • • • • Subconjunctival hemorrhage Development or exacerbation of abdominal wall hernia Rib fractures Loss of bladder control Weight loss, loss of appetite Dehydration Bloody nose Hemoptysis Cerebral hemorrhage, Encephalopathy Seizures (Bocka, 2014), (CDC, 2014), FOLLOW-UP • Most patients older than 1 year can be treated on an outpatient basis if they do not fulfill the criteria for hospital admission • Hospital admission is warranted for respiratory distress, pneumonia, inability to feed, apnea, and seizures • Frequent outpatient re-evaluations are required • frequency based on the patient's age, disease severity, and presence of comorbid conditions. (Bocka, 2014) COUNSELING/EDUCATION • Education regarding importance of vaccination administration *key to prevention* • Review risks associated with vaccine • Provide information regarding the infectious and contagious potential of pertussis • Seek medical attention if exposed for preventative antibiotics • Practice good hand hygiene • Avoid contact with high risk patients for at least 5 days after treatment initiation if diagnosed with B. pertussis CONSULTATION/REFERRAL • Consultation with subspecialists is usually not indicated • Unless…. • The diagnosis is unclear • Infectious disease consultation • (Bocka, 2014) QUESTION 1 • What is the macrolide used in infants <1 month? A. Erythromycin B. Azithromycin C. Clarithromycin ANSWER • B: Azithromycin is preferred in infants <1 month of age, unknown reaction with erythromycin and clarithromycin. Increased potential of pyloric stenosis with the use of erythromycin. Less side effects noted with azithromycin (Cornia & Lipsky, 2014) QUESTION 2 • What antibiotic can be used in the treatment of pertussis instead of a macrolide? • • • • A. Azithromycin B. Amoxicillin C. TMP-SMZ D. Ceftriaxone ANSWER C: TMP-SMZ: trimethoprim-sulfamethoxazole is an alternative agent for persons >2months who can not tolerate macrolides Infants: trimethoprim 8 mg/kg per day, sulfamethoxazole 40 mg/kg per day in 2 divided doses for 14 days. Adults: trimethoprim 320 mg per day, sulfamethoxazole 1,600 mg per day in 2 divided doses for 14 days. (Bocka, 2014) QUESTION 3 • How many vaccines are included in the diphtheria, tetanus, and pertussis (DTaP) series and at what ages are they administered? • A. 5 injections at birth, 6 months, 1 year, 18 months, and 2 years • B. 5 injections at 2, 4, 6 months, between 15-18 months and 4-6 years • C. 3 injections at birth, 1 year, and 2 years • D. 3 injections at 2, 6, 12 months ANSWER 3 • B: DTaP is given in a series of 5 injections between 6 weeks and 7 years of age. Given at 2 months, 4 months, 6 months, between 15-18 months and between 4-6 years of age. (CDC, 2014) QUESTION 4 • How long should individuals with Pertussis avoid contact with other individuals after starting antibiotics? • A. 24 hours B. 3 days C. 5 days D. 7 days ANSWER • C. Patients with B. pertussis should avoid contact with young children and infants until after they have completed 5 days of antibiotics. (Cornia & Lipsky, 2014) QUESTION 5 • Pregnant women can not get vaccinated with Tdap during pregnancy. • True or false? ANSWER • False • It is recommended that women get vaccinated with Tdap during each pregnancy preferably between 27-36 weeks gestation (CDC, 2014) QUESTION 6 • What test is the gold standard used by clinician’s to diagnose B. pertussis • • • • A. PCR B. Blood culture C. Nasopharyngeal culture D. Serology Testing ANSWER • C: Nasopharyngeal culture is the gold standard for identifying pertussis because it is a 100% specific. Results take 5-7 days. (CDC, 2014) • Best to collect sample within two weeks of symptom onset when viable bacteria are still present in the nasopharynx. After 2 weeks sensitivity is decreased and the risk of false-negatives increases. (CDC, 2014) QUESTION 7 • What is true about B. pertussis? • A. It does not affect adults over the age of 65. • B. Parents don’t need to get vaccinated if they vaccinate their children • C. It is the most commonly reported vaccine preventable illness in individuals less than 5 years old. ANSWER • C: Pertussis can affect individuals over the age of 65, they more frequently hospitalized than individuals between 11 and 64. • Parents who are in close contact with children need to get vaccinated despite vaccination status of other individuals. Adolescents and adults usually infect infants unknowingly. • Pertussis is a nationally reported illness, and the CDC states that is it the most commonly reported vaccine preventable illness in children less than 5. (CDC, 2014) QUESTION 8 • What is the best way to prevent B pertussis? • • • • A. Avoid contact with potentially infected individuals B. Vaccination C. Stay away from children D. Wash hands routinely ANSWER • B: The CDC states, “The best way to prevent pertussis (whooping cough) among infants, children, teens, and adults is to get vaccinated.” (CDC, 2014) QUESTION 9 • What is the most significant clinical finding in the second phase of B. pertussis? • • • • A. Fever B. Malaise C. Runny nose D. Paroxysmal cough ANSWER • D: Fever and runny nose are both clinical findings in the catarrhal phase • Malaise is a finding in the second phase but the malaise is typically a side effect related to the paroxysmal coughing fits(Cornia & Lipsky, 2014) QUESTION 10 • What is the most common complication of B. Pertussis? • • • • A. Pneumonia B. Rib Fractures C. Seizure D. Dehydration ANSWER • A: Pneumonia is the most common complication of B. pertussis, affecting about 1 in 20 individuals who are infected (CDC, 2014), (Bocka, 2014) REFERENCES • • • • • • • • • Bocka, J. (2014). Pertussis. Retrieved on October 6, 2014 from http://emedicine.medscape.com/article/967268-overview. Cornia, P. & Lipsky, B.A. (2014 April 9). Treatment and prevention of bordetella pertussis infection in adolescents and adults. Retrieved October 3, 2014, from http://www.uptodate.com/contents/treatment-and-prevetion-of-bodretella-pertussis. Cornia, P. & Lipsky, B.A. (2014 February 4). Microbiology, epidemiology, and pathogenesis of bardetella pertussi infection. Retrieved October 3, 2014, from http://www.uptodate.com/contents/microbiology-epidemiology-and-pathogenesis. Cornia, P., & Lipsky, B.A. (2014 March 13). Clinical manifestations and diagnosis of bardetlla pertussi infections in adolescents and adults. Retrieved October 3, 2014, from http://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-bodetella. Drutz, J.E.(2014, July14). Diphtheria, tetanus, and pertussis immunization in infacts and children 0 through 6 years of age. Retrieved on October 3, 2014 from http://www.uptodate.com/contents/diphtheria-tetanus-and-pertussis. Centers for Disease Control and Prevention. (2014). Pertussis, whooping cough. Retrieved on October 3, 2014 from http://www.cdc.gov/pertussis. MayoClinic. (2013). Whooping cough. Retrieved on October 6, 2014 from http://www.mayoclinic.org/diseases-conditions/whooping-cough/basics. Yeh, S. & Mink, C.M. (2014, June 17). Bordetella pertussis infection in infants and children: Clinical features and diagnosis. Retrieved October 3, 2014, from http://www.uptodate.com/contents/bordetella-infection-in-infants-and-children. Yeh, S. (2014, April 9). Treatment and prevention of bordetella pertussis in adolescents and adults. Retrieved October 3, 2014, from http://www.uptodate.com/contents/treatmentprevention-of-bordetlla-pertussis-infection.