* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Diphtheria (Corynebacterium diphtheriae)
Chagas disease wikipedia , lookup
Meningococcal disease wikipedia , lookup
Orthohantavirus wikipedia , lookup
Brucellosis wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Trichinosis wikipedia , lookup
West Nile fever wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Sarcocystis wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Gastroenteritis wikipedia , lookup
Hepatitis C wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Hepatitis B wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
Yellow fever wikipedia , lookup
Marburg virus disease wikipedia , lookup
1793 Philadelphia yellow fever epidemic wikipedia , lookup
Schistosomiasis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Oesophagostomum wikipedia , lookup
Neonatal infection wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Rocky Mountain spotted fever wikipedia , lookup
Yellow fever in Buenos Aires wikipedia , lookup
Leptospirosis wikipedia , lookup
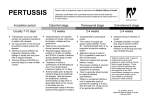
Typhoid fever wikipedia , lookup
Bacterial infections Diphtheria, Pertussis and Enteric fever Dr Mubarak Abdelrahman Assistant Professor Jazan University Gram negative: Diplococci Bacilli Coccobacilli Gram Positive: Diplococci Chains Clusters Rods & cocobacilli Diphtheria (Corynebacterium diphtheriae) •An acute toxic infection caused by •Corynebacterium diphtheriae •A gram-positive bacilli. Epidemiology C. diphtheriae : • An exclusive inhabitant of human mucous membranes and skin. • Spread by airborne respiratory droplets and direct contact. • Can remain viable in dust for 6 months. Pathogenesis The exotoxin: • Inhibits protein synthesis and causes local tissue necrosis. • In respiratory tract leads to pseudo-membrane. • Absorption can lead to systemic manifestations: e.g. kidney tubule necrosis, thrombocytopenia, cardiomyopathy, demyelination of nerves, .. Clinical Manifestations The manifestations are influenced by: • The anatomic site of infection. • The immune status of the host. • The production and distribution of the toxin. Respiratory Tract Diphtheria • Incubation period of 2-4 days (<7). • Local signs and symptoms of inflammation. • Soft tissue edema + enlarged lymph nodes causes a bull-neck appearance. A B A: Bull neck B: pseudo membrane C: Skin diphtheria C Diagnosis • Differential diagnoses: - Epiglottitis. - Exudative pharyngitis caused by Streptococcus pyogenes or Epstein-Barr virus. • Diagnosis: - Helped by the characteristic adherent membrane and relative lack of fever. - Specimens for culture from nose, throat and any other mucocutaneous lesion. Complications • Respiratory tract obstruction . • Toxic cardiomyopathy In 10-25% of patients with respiratory diphtheria and is responsible for 50-60% of deaths. • Toxic Neuropathy acutely or 2-3 weeks after onset of oropharyngeal inflammation: - Local paralysis: soft palate, pharynx, larynx, .. - Cranial neuropathies: oculomotor paralysis. - Symmetric polyneuropathy. Treatment • Specific antitoxin: Should be administered on the basis of clinical diagnosis. • The antibiotics (Erythromycin or penicillin) - Stop toxin production. - Treat localized infection. - Prevent transmission of the organism to contacts. • Supportive Care: - Bed rest is essential for ≥2 weeks (the period of risk for symptomatic cardiac damage). Prevention • Protection by immunization with toxoid. • All contacts are: - Closely monitored through the incubation period. - Given Antimicrobial prophylaxis regardless of immunization status. • Asymptomatic carriers also treated. Pertussis (Bordetella pertussis and Bordetella parapertussis) Pertussis meaning intense cough. Also known as whooping cough. Etiology: by Bordetella organisms: - Gram-negative coccobacilli. - Colonize only ciliated epithelium. Epidemiology • Pertussis is extremely contagious. • B. pertussis does not survive for prolonged periods in the environment. • Chronic carriage by humans is not documented. • Subclinical infection is around 80% . • Neither natural disease nor vaccination provides complete or lifelong immunity. Pathogenesis • The exact mechanism of disease remains unknown. • B. pertussis expresses pertussis toxin (PT) and other biologically active substances may be responsible for the local epithelial damage that produces respiratory symptoms and this facilitates absorption of PT. Clinical Manifestations • Incubation period 3-12 days. • Classically divided into 3 stages: 1. The catarrhal stage (1-2 weeks) congestion, rhinorrhea, low-grade fever, sneezing, lacrimation, .. 2. The paroxysmal stage (2-6 weeks) the cough begins as dry, intermittent, irritative, paroxysmal followed by a loud whoop ± Post-tussive vomiting. 3. The convalescent stage (≥2 weeks) the number, severity and duration of episodes diminish. Clinical Manifestations cont. • Infants <3 months: - No classic stages. - Apnea may be the only symptom. - Cyanosis is common. - Sudden infant death. • In non immunized infants: - Cough and whooping louder and more classic. • Adolescents and previously immunized children: - Mild illness. On physical examination: • No signs of lower respiratory tract disease. • Can be complicated by secondary pneumonia. • Conjunctival hemorrhage. • Petechiae on the upper body are common. Diagnosis • A clinical case definition of cough of ≥14 days’ duration with at least 1 associated symptom of paroxysms, whoop, or post-tussive vomiting. • Absolute lymphocytosis is characteristic in the catarrhal stage. • Diagnosis confirmed by: 1. Isolation of B. pertussis in nasopharyngeal swab culture (main). 2. Serologic tests: detection of antibodies to B. pertussis. Complications 1. Apnea. 2. Secondary infections (otitis media, pneumonia, ..). 3. Physical sequelae of forceful coughing e.g: - conjunctival hemorrhages. - epistaxis. - hemorrhage in the central nervous system. - pneumothorax. - umbilical and inguinal hernias. 4. Bronchiectasis has been reported. Treatment • Infants <3 months of age with suspected pertussis are always admitted to hospital. • Antibiotics are always given when pertussis is suspected or confirmed. • Macrolides are the preferred agents (erythromycin, Azithromycin) • Isolation of patients and prophylaxis antibiotics to all contacts regardless of age or immunization. Prevention • Immunization with pertussis vaccine, beginning in infancy with periodic reinforcing doses through adolescence and adulthood. Enteric Fever (Typhoid Fever) Etiology: Typhoid fever is caused by Salmonella Typhi and S. Paratyph, a gram-negative bacilli. Epidemiology • In developed countries: <15 cases/100,000. • In the developing world, estimated rates bet. 100 to 1,000 cases/100,000 population. • The highest incidence, complications and hospitalization in children <5 years of age. • Direct or indirect contact with an infected person (sick or chronic carrier) is a prerequisite for infection. Pathogenesis • After ingestion, S. typhi invade through the gut mucosa to mesenteric lymphoid system then into the bloodstream causing bacteremia. • The incubation period 7-14 days; (3-30)days. Clinical Features • Mild illness (low-grade fever, malaise, dry cough). • Severe (high-grade fever, generalized myalgia, abdominal pain, hepatosplenomegaly, anorexia, ..). • The classic stepladder rise of fever is relatively rare. In children, diarrhea may be followed by constipation. • Rose spots: - Macular/maculopapular rash. - appear around the 7-10th day of the illness. - on the lower chest and abdomen. - last 2-3 days. Complications • Hepatitis and cholecystitis. • Intestinal hemorrhage and perforation. • Toxic myocarditis. • Neurologic complications (delirium, psychosis, Guillain-Barre syndrome..). • Others: DIC, hemolytic-uremic syndrome, nephrotic syndrome, meningitis and suppurative lymphadenitis. Differential Diagnosis • Acute gastroenteritis, bronchitis, and bronchopneumonia. • Malaria and sepsis with other bacterial pathogens. • Tuberculosis, brucellosis, Dengue fever, acute hepatitis, infectious mononucleosis. • Others (malignancies, rheumatological, …) Diagnosis • The mainstay is by a positive culture . - Blood cultures early. - Stool and urine culture after the 1st wk. • Leukocyte counts frequently low in relation to fever and toxicity. • Thrombocytopenia: severe illness (may accompany DIC). • Liver function test. • Widal test but many false-positive and false-negative results. • Other diagnostic tests: PCR and monoclonal antibodies. • In the developing world the mainstay of diagnosis is clinical. Treatment • Supportive: adequate rest, hydration, correct fluid and electrolyte. • Antipyretic therapy. • A soft, easily digestible diet if no abdominal distention or ileus. • Antibiotic therapy (chloramphenicol or amoxicillin quinolones or third-generation cephalosporin) Prevention • Good sanitation services and central chlorination of water. • Avoid consumption of street foods! • Hand washing. Vaccination: (two vaccines) 1. An oral, live-attenuated preparation of S. Typhi, from 6 years of age. 2. The Vi capsular polysaccharide for ≥2 years of age. Intramuscular with a booster every 2 years.