* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Hyperthyroidism and Thyroid Storm
Survey
Document related concepts
Transcript
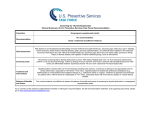
Hyperthyroidism and Thyroid Storm Jeffrey S. Freeman DO FACOI FNLA Chairman Division of Endocrinology and Metabolism Philadelphia College of Osteopathic Medicine Who is at risk for hyperthyroid? • Individuals with – – – – Diffuse or Nodular Goiters Type 1 diabetes (also, other endocrine and AI diseases) Family history of hyper/hypo Medications • • • • • • Amiodarone Alpha-interferon Interleukin-2 Lithium Iodide Iodinated contrast agents – Only for those with preexisting Symptoms to consider… • Nervousness (99%) • Increased sweating (91%) • Palpitations (89%) • Tachycardia (82%) • Heat intolerance (89%) • Fatigue (88%) • Weight loss (85%) • Shortness of breath (75%) • Weakness (70%) • Leg swelling (65%) • Eye symptoms (54%) • Hyperdefication (33%) • Menstrual irregularity (22%) • Emotional lability (3060%) Physical Exam findings • • • • • Tachycardia (100%) Goiter (100%) Skin changes (97%) Tremor (97%) Bruit (77%) • • • • Eye Signs (30-45%) Atrial fibrillation (10%) Splenomegaly (10%) Gynecomastia (10%) How do you diagnose? • Order Serum TSH – Low: free T4 or free T4 index • If not elevated, order total T3 or free T3 • Radioiodine uptake • Thyroid scan • Radioisotope studies contraindicated… – Blood tests: • TSH-receptor antibodies • Thyroid-stimulating immunoglobulins • Thyroid-peroxidase antibodies • Thyroglobulin • HCG • Sed rate – Color Doppler US – Whole body radioiodine scan Lab studies--indications • TSH—suspected hyperthyroidism – Free thyroxine (FT4)—suppressed TSH – Free triiodothyronine (FT3) --suppressed TSH, normal FT4 • Thyroglobulin --suspected thyroiditis • Erythrocyte sed rate ESR--suspected subacute thyroiditis • TSH-receptor antibodies--euthyroid Graves ophthalmopathy – assess remission with antithyroid drug Rx in Graves disease; – assess neonatal risk in pregnant patients with Graves disease • Thyroid peroxidase antibodies--confirm Hashimoto thyroiditis or autoimmune thyroid disease – assess risk for Rx-induced thyroid dysfunction and postpartum thyroiditis RAIU--confirmed biochemical thyrotoxicosis, if cause unclear Thyroid scan--confirmed biochemical thyrotoxicosis, if cause unclear Whole body scan--suspected struma ovarii Color Doppler US--type I vs. type II amiodarone-induced thyrotoxicosis • Human chorionic gonadotropin HCG--choriocarcinoma Alternative Explanations • Infection • Sepsis • Anxiety • Depression • Chronic Fatigue Syndrome • Atrial fibrillation of other causes • Pheochromocytoma TSH usually distinguishes these from hyperthyroidism • BUT Serum TSH is low in: – pregnancy, hyperemesis gravidarum; – euthyroid sick syndrome; – central hypothyroidism (with glucocorticoids, dopamine, heparin) What non-drug therapies? • Until thyroid disease is adequately controlled – – – – – Avoid heavy physical exertion Reduce/eliminate caffeine intake Ovoid OTC decongestants and cold remedies Discontinue smoking Avoid exogenous sources of iodine Choosing drug therapies • Beta-adrenergic blockade: symptomatic hyperthyroidism of any cause – Propranolol, atenolol, metoprolol, nadolol • Side effects: CHF + asthma exacerbations • Antithyroid medications: inhibits thyroid hormone synthesis, thus lower thyroid hormone – Methimazole: preferred – Propylthiouracil: alternative • If 1st trimester of pregnancy, if MZ allergy, thyroid storm – Side effects: beware LIVER FAILURE, agranulocytosis in 0.2-0.4% – Use: Graves, toxic multinodular goiter, toxic adenoma – Don’t use for: low RAIU, hyperthyroidism Ancillary Therapy • Potassium iodine : acutely reduces thyroid hormone release – Use before thyroidectomy for Graves – Don’t use before radioactive iodine therapy • Lithium: reduces thyroid hormone release • Cholestyramine: binds thyroid hormone in intestines • Nonsteroidal anti-inflammatory: treats subacute thyroiditis • Glucocorticoids: for severe subacute thyroiditis When do you consider I-131? • Graves disease – Achieves remission in 90% – Good choice if no remission with antithyroid medications • Side effects of I-131 – Hypothyroidism: eventually – Sialadenitis: due to uptake by salivary glands (can be quite painful) – Worsening of orbitopathy – Possible small increase in thyroid cancer When should you consider I-131? • Toxic multinodular goiters & toxic adenomas – Pretreat with beta-adrenergic blockade and/or – Methimazole: if very symptomatic or free T4 or FT4I levels exceed upper limit more than 2x • D/C Methimazole at least 7 days before I-131 • Propylthiouracil use may also apply • Side effects of I-131 (not in pregnancy) – Hypothyroidism: 50-70% – Worsened symptoms in first 2 weeks from thyroid hormone increase – Thyroid storm, if severely hyperthyroid When thyroidectomy? • Most often recommended for… Those who can’t tolerate or refuse alternative forms of RX – Pregnancy – Patients who don’t achieve remission with antithyroid RX – Unable to perform I131 therapy do to exopthalmus Antithyroid medication monitoring – Agranulocytosis, liver injury, vasculitis: discontinue – Fever or pharyngitis: repeat CBC with differential WBC – Symptoms of liver injury: order liver profile Once symptoms resolved + results in reference range… • Discontinue β-adrenergic blocker + reduce antithyroid Rx • Continue clinical and lab assessments every 3–6 months After 12-18 months reduced dose + normal TSH: ? Remission – Taper or stop antithyroid Rx – Measure TRAb: normal = greater likelihood remission No remission: consider I-131 or surgery Case • 57 y/o female presents to the ER with anxiety, disruptive, nervousness, SOB. She notes exacerbation of these symptoms over the course of a month. She is currently too weak to walk up steps with proximal muscle weakness. • PMH: Grave’s disease treated with Methimazole 20 mg/daily. • PE: Temp: 101.2 b/l proptosis, conjunctival injection, neck b/l thyroid enlargement (with bruits) firm to palpation, HR: 140 (regular), coarse systolic murmur, lungs CTA, abdomen flat. Integument smooth in texture and warm in temperature. Reflexes: brachioradialis 3+/4+ • Labs: ultrasensitive TSH <0.01 mg, FreeT4 6.8, WC 12,000, LFT: normal, What is thyroid storm? • Acute, life-threatening exacerbation of thyrotoxicosis • After surgery for thyroidectomy? Infection? Recognizing Thyroid Storm Thyroid crisis: exaggerated manifestations of thyrotoxicosis – Unrecognized/untreated thyrotoxicosis + precipitating event (infection, trauma) – Radioiodine therapy may precipitate – Dx: often based on suspicious, non-specific clinical findings • Cardinal manifestations: fever >102 fever • Other features: tachycardia, tachypnea; nausea/vomiting, diarrhea, CNS manifestations, anemia, hyperglycemia • Elevated serum total, free T4 and T3 levels; undetectable serum TSH levels Use Thyroid Scoring System Thyroid Storm Scoring System Fever ° F Score 99–99.9 5 99–109 5 100–100.9 10 110–119 10 N, V, D, Pain 10 101-101.9 15 120–129 15 Jaundice 20 102-102.9 20 130–139 20 Precipitant history 103-103.9 25 ≥140 25 Absent 0 >104 30 Atrial fibrillation 10 Present 10 GI signs Absent Cardiac–CHF CNS agitation Absent 0 Cardiac–pulse, bpm 0 Absent 0 5 Mild 10 Mild (edema) Moderate 20 Moderate (rales) 10 Severe 30 Severe (pulm edema) 15 Total Score <25= unlikely 25-44= suggestive >45= likely 0 How does a clinician treat? 1. Decrease thyroid hormone synthesis – Propylthiouracil or methimazole 2. Inhibit thyroid hormone release – Sodium iodide (IV) or potassium iodide (oral) (not before blocked) 3. Reduce heart rate – β-blocker (esmolol, metoprolol, propranolol) or diltiazem 4. Support circulation • Glucocorticoids in stress doses • Fluids (IV), oxygen, cooling 5. Treat precipitating cause 6. NO ASPIRIN!! When should patients be hospitalized? • When thyroid storm present, impending, or suspected – Prognosis with aggressive therapy ≈20% mortality (was once 100%) – Dx usually based on suspicious, nonspecific findings – Do not wait for test results on serum TSH levels: delays potentially lifesaving therapy – Also, TSH levels don’t reliably distinguish thyroid storm from uncomplicated thyrotoxicosis Questions?