* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Left Ventricular Untwisting Is an Important Determinant of Early
Cardiac contractility modulation wikipedia , lookup
Electrocardiography wikipedia , lookup
Heart failure wikipedia , lookup
Artificial heart valve wikipedia , lookup
Echocardiography wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
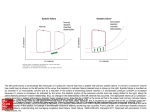
JACC: CARDIOVASCULAR IMAGING VOL. 2, NO. 6, 2009 © 2009 BY THE AMERICAN COLLEGE OF CARDIOLOGY FOUNDATION PUBLISHED BY ELSEVIER INC. ISSN 1936-878X/09/$36.00 DOI:10.1016/j.jcmg.2009.01.015 Left Ventricular Untwisting Is an Important Determinant of Early Diastolic Function Andrew T. Burns, MB, BS (HONS), BMEDSCI, MD,* Andre La Gerche, MB, BS,* David L. Prior, MBBS, PHD,*† Andrew I. MacIsaac, MBBS, MD*† Melbourne, Victoria, Australia O B J E C T I V E S We sought to establish the relationship between invasive measures of diastolic function and untwisting parameters measured with speckle tracking imaging. B A C K G R O U N D Left ventricular (LV) diastolic function is determined by early diastolic relaxation (which creates suction gradients for LV filling) and myocardial stiffness. Assessment of LV torsion has shown that untwisting begins before aortic valve closure and, in animals, might be an important component of normal diastolic filling. Studies in human subjects using indirect indexes derived from right heart catheterization have suggested a relationship between and measures of untwisting, but the relationship between directly measured diastolic function indexes with micromanometer catheters and untwisting parameters has not been established in human subjects. M E T H O D S Simultaneous Millar micromanometer LV pressure and echocardiographic assessment was performed on 18 patients (10 male, mean age 66 years) with normal systolic function and a spectrum of diastolic function. Invasive rate of the rise of LV pressure, dp/dt minimum and were recorded as measures of active relaxation, and the LV minimum diastolic pressure was recorded as an index of diastolic suction. The LV stiffness constant and functional chamber stiffness were estimated from hybrid pressure-volume loops. Echocardiographic speckle tracking imaging was used to quantify torsion. R E S U L T S As relaxation was impaired, (prolonged ) untwisting was delayed (r ⫽ 0.35, p ⬍ 0.01). There were nonsignificant associations between reduced untwisting and longer values of and lower dp/dt minimum. Reduction in the extent of untwisting before mitral valve opening was associated with increased LV minimum diastolic pressure (r ⫽ ⫺0.30, p ⬍ 0.034). No relation was observed between the LV stiffness constant (: r ⫽ 0.11, p ⫽ NS) or the functional LV chamber stiffness (b: r ⫽ 0.11, p ⫽ NS) and untwisting. C O N C L U S I O N S Untwisting parameters are related to invasive indexes of LV relaxation and suction but not to LV stiffness. These data suggest that untwisting is an important component of early diastolic LV filling but not later diastolic events. (J Am Coll Cardiol Img 2009;2:709 –16) © 2009 by the American College of Cardiology Foundation From the *Cardiac Investigation Unit and †University of Melbourne Department of Medicine, St. Vincent’s Hospital Melbourne, Victoria, Australia. Dr. Burns is supported by a Postgraduate Research Scholarship from the National Heart Foundation of Australia. Manuscript received July 28, 2008; revised manuscript received December 18, 2008, accepted January 23, 2009. 710 Burns et al. Untwisting in Diastolic Function JACC: CARDIOVASCULAR IMAGING, VOL. 2, NO. 6, 2009 JUNE 2009:709 –16 T raditional measures of left ventricular (LV) diastolic function have focused on relaxation and stiffness. Early diastolic LV relaxation creates intraventricular pressure gradients or suction gradients that are important, because they allow efficient LV filling without increasing left atrial (LA) pressure (1,2), particularly during exercise (3,4). See page 717 Torsion, the rotation of the apex and the base of the LV on its longitudinal axis in opposite directions, results from the contraction of the obliquely oriented subendocardial and subepicardial helixes (5,6). The LV untwisting results begins before aortic valve closure and before longitudinal and radial expansion (7). Because it is one of the earliest events leading to LV filling, untwisting might be a critical determinant of early diastolic function. The quantification of LV untwisting might provide novel insights into diastolic function (8,9), ABBREVIATIONS in particular the generation of intravenAND ACRONYMS tricular pressure gradients (10). Dong et al. (11) found, in a canine dp/dt ⴝ rate of the rise of left model, a strong correlation between recoil ventricular pressure rate assessed with cardiac magnetic resoGTN ⴝ glyceryl trinitrate nance and invasively measured . More IVRT ⴝ isovolumic relaxation recently, Wang et al. (12) showed that time untwisting rate was related to a time conLA ⴝ left atrial stant of isovolumic relaxation, both paLV ⴝ left ventricle/ventricular rameters being derived from echocardioMVO ⴝ mitral valve opening graphic data (13) rather than invasive STI ⴝ speckle tracking imaging measurement. Clinical studies have shown a consistent reduction in the magnitude and delay in the timing of untwisting in the context of diastolic dysfunction due to aortic stenosis (14), hypertrophic cardiomyopathy (15), and severe LV hypertrophy (16), supporting an important role for untwisting in abnormal diastolic function. Thus, the relationship between invasively measured indexes of diastolic function and torsion parameters in human subjects is not known. We set out to establish the relationship between parameters of untwisting and invasive hemodynamic measures of early and late diastolic filling in human subjects with a range of diastolic function. METHODS Patient selection. Patients referred for routine coronary angiography to investigate chest pain were invited to participate. Patients with acute coronary syndrome, abnormal systolic function, regional wall motion abnormality, valvular heart disease of worse than moderate severity, atrial fibrillation, permanent pacemaker, history of coronary artery bypass graft surgery, renal impairment (estimated glomerular filtration rate ⬍60 ml/min/1.73 m2), and abnormal QRS complex morphology on electrocardiogram were excluded. This study was undertaken with the approval of the Human Research Ethics Committee of St. Vincent’s Health, and written informed consent was obtained from all subjects. Routine echocardiographic analysis. The following echocardiographic data were acquired at end expiratory apnea: apical 4- and 2-chamber views of the LV; a parasternal long-axis view; and short-axis images at level of mitral valve, the mid-ventricle, and apex. Pulsed wave Doppler of the LV outflow tract and mitral inflow were recorded and stored in raw data format for offline analysis. Three cycles were analyzed, and the results were averaged. To calculate ejection fraction, LV end-diastolic and end systolic volumes were measured with a Simpson’s biplane method. Mitral inflow and tissue Doppler velocities and the isovolumic relaxation time (IVRT) were recorded as previously described (17). Diastolic function was classified as abnormal on the basis of the invasive criteria (18): ⬎48 ms or LV end-diastolic pressure ⬎16 mm Hg or mean LV diastolic pressure ⬎12 mm Hg. Those with abnormal diastolic function were then classified as having impaired relaxation or pseudonormal or restrictive patterns of echocardiographic diastolic filling (19). The LV mass index was calculated with the area-length method and LV hypertrophy was defined according to standard criteria (20): LV mass index ⬎115 g/m2 for men and ⬎95 g/m2 for women. Speckle tracking imaging and torsion analysis. The speckle tracking imaging (STI) algorithm and torsion analysis technique have been described in detail previously (21,22). Briefly, offline analysis of raw ultrasound data was performed with EchoPac PC software (version 4.1, GE Medical Systems, Princeton, New Jersey). Speckle tracking analysis with 2-dimensional images was performed as previously described (23) on high frame rate (50 to 90 Hz) single-focus parasternal short-axis images at the level of the mitral valve (mitral valve leaflets on view) and apex (circular LV cavity with no papillary muscle visible) (21) to generate rotation and rotation rate data. Frame by frame rotation and rotation rate data were exported to Excel (Microsoft Corporation, Seattle, Washington), and temporal data were normalized to the percentage duration of systole and diastole separately as previously de- Burns et al. Untwisting in Diastolic Function JACC: CARDIOVASCULAR IMAGING, VOL. 2, NO. 6, 2009 JUNE 2009:709 –16 Left ventricular torsion = apical rotation - basal rotation Torsion (degrees) 7.5 Tmvo Tpeak Apical rotation Basal rotation Torsion 5.0 2.5 AVC MVO 0.0 Time -2.5 Systole Diastole -5.0 Recoil (%)= Tpeak - Tmvo x 100 Tpeak B Torsion velocity (deg/sec) A Left ventricular torsion velocity= apical rotation rate - basal rotation rate Peak positive torsion velocity 50 25 0 Time -25 -50 Recoil rate (%/sec)= Peak untwisting velocity Recoil Time (Tpeak) - Time (Tmvo) Figure 1. Torsion and Torsion Velocity Versus Time Plot (A) Torsion versus time plot. Left ventricular torsion (black line) was calculated by subtracting basal rotation (red line) from apical rotation (orange line). Positive torsion rate (dashed line) was the slope of the torsion versus time curve from the beginning of systole to peak torsion (Tpeak). Recoil was the percentage decrement from peak torsion to torsion at mitral valve opening (Tmvo), and recoil rate was calculated as recoil divided by the time from Tpeak to Tmvo. (B) Torsion velocity versus time plot. Left ventricular torsion velocity (yellow line) was calculated by subtracting basal rotation rate from apical rotation rate. Peak positive torsion velocity and peak untwisting velocity are indicated by the arrows. AVC ⫽ aortic valve closure. scribed (24). Because apical and basal rotation data cannot be acquired from the same cardiac cycle and to allow comparison within and between subjects, cubic spline interpolation (Graphpad Prism Plus software, San Diego, California) was undertaken with 300 data points for both systole and diastole. Subtraction of the basal data from the apical data at each of the interpolated time points was undertaken to calculate torsion and torsion velocities (Fig. 1). Three cycles were analyzed, and the results were averaged. Definition of torsion parameters. Peak torsion (Tpeak) was defined from the torsion versus time curve and positive torsion rate as the slope from the start of systole to peak torsion (Fig. 1A). Torsion at the time of mitral valve opening (Tmvo) (Fig. 1) was used to calculate the indexes recoil (Fig. 1A) and recoil rate (recoil rate ⫽ recoil/[timeTpeak ⫺ timeTmvo]) (11). The real time of peak torsion and mitral valve opening was used for the calculation of recoil rate rather than normalized time. Peak positive torsion velocity and peak untwisting velocity were defined from the torsion velocity versus time curve (Fig. 1B). The time to peak untwisting velocity was measured from mitral valve opening. Simultaneous micromanometer LV pressure and echocardiography. Studies were undertaken in the cath- eterization laboratory with the subjects in the supine position. Echocardiography was performed with a VIVID 7 echocardiograph (GE Medical Systems). A single-use 5-F Millar micromanometer catheter (SPC-454D, Millar Instruments, Inc., Houston, Texas) was placed within the LV, and ventricular pressures were recorded with Powerlab/ 4sp recording unit (ADI Instruments, Mountain View, California) connected to an iMac desktop computer (Apple, Cupertino, California). The LV pressure data were acquired with Chart 3.6.3 for MacOS (ADI Instruments) during each of the 4 conditions. Data from 5 cycles at each condition were analyzed and averaged. The dp/dt minimum, (25,26), and minimum LV diastolic pressure (LV minimum pressure) (27) were recorded as invasive measures of diastolic function. Simultaneous echocardiograph and pressure recordings were obtained under 4 conditions: PreGTN ⫽ in the fasting state; GTN ⫽ at nadir of LV pressure after sublingual glyceryl trinitrate (GTN) administration (if the subject’s resting LV pressure was ⬍110 mm Hg [n ⫽5], 300 g of sublingual GTN was administered; for the remainder of patients, 600 g was administered); Pre-fluid ⫽ stable hemodynamic state at least 15 min after GTN administration; and Fluid ⫽ after rapid infusion of 750 ml normal saline (warmed to 37°C). Pressure–volume relations. With simultaneous micromanometer pressure and echocardiographic volume data, a pressure–volume relation was plotted from the coordinates under each of the hemodynamic conditions at minimum diastolic pressure and end-diastolic pressure (Fig. 2). From the micromanometer pressure versus time data, enddiastolic pressure was defined as the pressure at 10% of dp/dt maximum (28). The LV stiffness constant, , was estimated from the slope of the linear regression equation relating the end-diastolic pressure to volume coordinates 711 Burns et al. Untwisting in Diastolic Function JACC: CARDIOVASCULAR IMAGING, VOL. 2, NO. 6, 2009 JUNE 2009:709 –16 LV functional chanber stiffness LV stiffness constant 30 Pressure 712 20 10 Min diast p End diast p 0 0 25 50 75 100 125 Volume Figure 2. Pressure-Volume Loop Derived From Simultaneous Micromanometer Pressure and Echocardiographic Volume Data points for minimum diastolic pressure (squares) and end diastolic pressure (triangles) are shown under each of the 4 conditions. The linear functional chamber stiffness (orange line) and left ventricular (LV) stiffness constant (yellow line) are shown. under each of the conditions (Fig. 2). The functional LV chamber stiffness, b, under each condition was the linear slope of the pressure-volume curve from minimum diastolic pressure to enddiastolic pressure (Fig. 2) (29,30). Statistics. Normality of data was assessed with the Kolmogorov-Smironov statistic. Where data were not normally distributed, log transformation was applied, and tests were performed on the log transformed data. Repeated-measures linear regression was performed to quantify the relationship between torsion and invasive indexes of diastolic function as previously described (11). The commercially available statistics software SPSS (SPSS Inc., Chicago, Illinois) was used. Data are presented as mean ⫾ SD unless otherwise specified, and p ⬍ 0.05 was considered significant. RESULTS Patient characteristics. The demographic data of the 18 patients included in the study are summaTable 1. Patient Characteristics (n ⴝ 18) Male, n (%) 10 (56%) Age (yrs), mean ⫾ SD (range) 65.7 ⫾ 7.6 (47–77) Body mass index, kg/m2, mean ⫾ SD (range) 28.0 ⫾ 3.9 (22.2–36.7) Hypertension, n (%) Type 2 diabetes mellitus, n (%) Heart failure Current smoker Hyperlipidemia, n (%) 11 (61%) 3 (17%) 0 0 9 (50%) rized in Table 1. According to invasive criteria, 9 patients had normal diastolic function and 9 patients had abnormal diastolic function. Of the 9 patients with abnormal diastolic function by invasive criteria, 3 had an impaired relaxation pattern, 6 had a pseudonormal pattern, and none had a restrictive pattern of diastolic filling by echocardiographic criteria. Mean LV mass index was 89.2 ⫾ 3.6 g/m2 (range 58.3 to 120.8 g/m2), and 3 patients had LV hypertrophy. Of the eleven hypertensive patients, 8 required 1 antihypertensive and 3 required 2 antihypertensive medications. Nine patients had angiographically smooth coronary arteries, 3 had minor diffuse disease, 4 had single-vessel stenosis of ⬎70%, and 2 had multivessel stenoses of ⬎70%. A pre-fluid dataset was not collected in 3 subjects, and poor image quality meant that torsion analysis could not be performed on 2 subjects in the GTN dataset. Effect of LV mass and preload on measures of diastolic function. As LV mass increased, was prolonged (r ⫽ 0.34, p ⬍ 0.002), and there were reductions in peak untwisting velocity (r ⫽ 0.57, p ⬍ 0.007) but not recoil (r ⫽ ⫺0.26, p ⫽ NS) or recoil rate (r ⫽ 0.32, p ⫽ NS). As preload increased (increased end-diastolic volume and pressure), was prolonged, but no consistent effect on untwisting parameters was observed (Table 2). Correlation between measures of diastolic function. As was prolonged, the time to peak untwisting velocity was delayed (r ⫽ 0.34, p ⬍ 0.01). There were nonsignificant associations between reduced recoil and longer values of and lower dp/dt minimum (Fig. 3). No relationship was observed between the echocardiographic IVRT and or between IVRT and untwisting parameters. The LV minimum diastolic pressure increased as was longer (Fig. 4A) (r ⫽ 0.67, p ⬍ 0.001) and recoil decreased (Fig. 4B) (r ⫽ ⫺0.30, p ⬍ 0.034). No relationship was observed between LV minimum diastolic pressure and peak untwisting velocity or recoil rate. Relationships were observed between the magnitude of peak untwisting velocity and that of the systolic torsion parameters peak torsion (r ⫽ ⫺0.75, p ⬍ 0.001), positive torsion rate (r ⫽ ⫺0.60, p ⬍ 0.001), and peak positive torsion velocity (r ⫽ ⫺0.42, p ⬍ 0.002). Relation between LV stiffness and untwisting indexes. No relation was observed between measures of stiffness, the LV stiffness constant, , and the functional LV chamber stiffness, b, and the untwisting indexes recoil, recoil rate, and peak untwisting velocity (Table 3). Burns et al. Untwisting in Diastolic Function JACC: CARDIOVASCULAR IMAGING, VOL. 2, NO. 6, 2009 JUNE 2009:709 –16 DISCUSSION Table 2. Correlation Coefficients Between Measures of Preload and Diastolic Parameters We have shown in human subjects with invasive measures of LV pressure that indexes of untwisting are related to parameters of early diastolic filling but not events happening later in diastole. Reductions in the rate and magnitude of untwisting were associated with worsening of diastolic relaxation and reduced early diastolic suction. These findings lend further weight to the hypothesis that untwisting is important in generating early diastolic LV suction, an important component of early diastolic filling. There was a close relationship observed between systolic and diastolic torsion parameters, suggesting that torsion might be an important mechanistic link between the phases of the cardiac cycle. Our data are in keeping with earlier findings in a canine model where, with cardiac magnetic resonance, Dong et al. (11) described a close relation between recoil rate and invasively measured . Wang et al. (12) found that the untwisting rate correlated with a time constant of isovolumic relaxation in patients with systolic LV dysfunction, but this correlation was not maintained in patients with preserved LV ejection fraction. This inconsistency might be due to a failure to interpolate temporally normalized STI data or an artefact of the method used to derive from echocardiographic and right heart catheterization data (13) rather than direct invasive measurement, as we have used in this patient group with normal ejection fraction. The correlations between invasive and untwisting parameters in our study were weaker than those A Peak Untwisting Velocity Recoil End-diastolic r ⫽ 0.36 r ⫽ 0.11 r ⫽ 0.09 r ⫽ 0.05 volume p ⬍ 0.01 p ⫽ NS p ⫽ NS p ⫽ NS Recoil Rate End-diastolic r ⫽ 0.41 r ⫽ 0.17 r ⫽ 0.08 r ⫽ 0.15 pressure p ⬍ 0.003 p ⫽ NS p ⫽ NS p ⫽ NS reported with published animal data (11) but are still consistent with an important role for untwisting in early diastolic function. In our study, the method of Weiss (25) was used, which assumes that the LV pressure decays to a zero asymptote, whereas in the study by Dong et al. (11), a zero pressure asymptote was not assumed. There is some controversy about the use of a zero pressure asymptote (31); however, it has been the most commonly used method in human studies and has established reference values (26). In addition, Dong et al. (11) calculated recoil with torsion at 64 ms after mitral valve opening as a proportion of maximal torsion. This differs slightly from the definition of recoil used in contemporary studies employing STI (24,32). The arbitrary time point of 64 ms does not completely account for isovolumic relaxation, the load independent period of negative torsion. To reflect the changes in torsion during the isovolumic period, an argument could be made that the torsion at end systole should be used rather than the peak torsion. However, in some patients, maximal tor- B τ Figure 3. Recoil Versus and Recoil Versus dp/dt Minimum Eighteen subjects underwent simultaneous Millar catheter micromanometry and echocardiography under 4 conditions: at rest (Pre-GTN) (brown squares); after 600-g sublingual GTN (GTN) (red triangles); after a period of re-equilibration (Pre-fluid) (orange circles), and after 750-ml intravenous saline bolus (Fluid) (yellow diamonds). Torsion parameters were measured with speckle tracking imaging, and repeated measures linear regression was used to quantify relations between invasive and torsion indexes. We observed nonsignificant associations between reduced untwisting and longer values of the time constant of isovolumic relaxation, (A), and a lower rate of the rise of left ventricular pressure (dp/dt) minimum (B) in keeping with previous work in animal models. This supports an important role for untwisting in early diastolic function. 713 Burns et al. Untwisting in Diastolic Function JACC: CARDIOVASCULAR IMAGING, VOL. 2, NO. 6, 2009 JUNE 2009:709 –16 A B PreGTN GTN Prefluid Fluid 60 55 50 125 Recoil (%) 65 τ (ms) 714 45 r = -0.32, p < 0.005 100 75 50 40 25 35 -5 r = 0.67, p < 0.001 0 5 10 15 20 LV minimum diastolic pressure (mmHg) -5 0 5 10 15 20 LV minimum diastolic pressure (mmHg) Figure 4. Versus LV Minimum Diastolic Pressure and Recoil Versus LV Minimum Diastolic Pressure Left ventricular (LV) suction is an important component of early diastolic function that allows LV filling without excessive increases in left atrial pressure. Lower LV minimum diastolic pressure increases suction. We found that impaired suction was associated with slower isovolumic relaxation (A). As untwisting decreased, suction was also impaired (B), further evidence for an important role for untwisting in early diastolic function. sion occurs after end systole, and this would lead to an inconsistency in the measurement (16). Therefore, we calculated recoil and recoil rate as the decrement in torsion from peak to mitral valve opening (Fig. 1). We have shown that suction was reduced in subjects with decreased recoil. Although LV minimum diastolic pressure is an accepted index of suction in clinical studies (27), the gold standard assessment involves the measurement of intraventricular pressure gradients with a triple sensor micromanometer catheter placed across the mitral valve to record LA, basal LV, and apical LV pressures. This technique is limited to animal models (1) and the clinical open heart surgery setting (2). More recently, the mitral inflow propagation velocity derived from color M-mode Doppler has been validated as a noninvasive index of intraventricular pressure gradient (4,33). With this technique and tissue Doppler-derived measurement of torsion, Notomi et al. (10) suggested that untwisting velocity is an important determinant of early diastolic LV suction. Our study provides invasive data to support this hypothesis. The observed effect of increased LV mass on untwisting velocity is consistent with the findings of Table 3. Correlation Coefficients Between Invasive Measures of Stiffness and Diastolic Torsion Parameters Recoil Recoil Rate Peak Untwisting Velocity LV stiffness constant 0.11 ⫺0.023 ⫺0.015 Functional LV stiffness 0.11 ⫺0.10 ⫺0.049 LV ⫽ left ventricular. clinical studies involving patients with LV hypertrophy (14 –16). No relation was observed between untwisting parameters and the LV stiffness constant or the functional LV chamber stiffness. Untwisting begins before aortic valve closure (7,10), and a lack of correlation with late diastolic parameters of stiffness is not unexpected. Although invasive pressure-volume loop analysis with conductance catheters is the gold standard to measure stiffness, pressure-volume loops derived from simultaneous micromanometer pressure and echocardiographic volume are well-validated (26). The end-diastolic pressure-volume relation is generally modeled from conductance catheter data with nonlinear equations (34); however, the ranges of diastolic pressure and volume coordinates produced by the hemodynamic manipulations in the current study could be accurately modeled with linear regression as previously described (30,35). The observation of close relations between systolic and diastolic torsion indexes lends weight to the hypothesis that torsional motion results from the buildup and release of elastic energy (10,36), possibly in the molecule of the large elastic cardiomyocyte protein titin, which acts as a bidirectional spring (37). Titin itself has been shown to be a major determinant of early diastolic function (38,39), and changes in titin isoforms have been documented in the context of ventricular dysfunction (40). In an animal heart failure model, rapid ventricular pacing induced a change to stiffer titin isoforms, resulting in reduced systolic twist and diastolic untwisting associated with reduced suction gradients (41). Further work is required to elucidate Burns et al. Untwisting in Diastolic Function JACC: CARDIOVASCULAR IMAGING, VOL. 2, NO. 6, 2009 JUNE 2009:709 –16 the role of titin in untwisting and diastolic suction in humans. Study limitations. Eighteen patients with normal systolic function were assessed in this study, of whom one-half had diastolic dysfunction on invasive criteria. The failure to reproduce the strong correlations between invasive and torsion indexes of diastolic function might relate to the small sample size in our cohort and the relatively narrow dynamic range through which the invasive parameters were manipulated in our experiment relative to what can be achieved in the animal model with varying pacing modes, dobutamine, and esmolol. Although GTN and fluid administration have some effect on afterload, their predominant effect is on preload. Maneuvers to specifically manipulate afterload, such as vasopressor administration, would be of great interest but were felt to be unwarranted in this experiment. To elucidate the clinical utility of measuring torsion parameters to characterize diastolic function, a larger group of systolic and diastolic heart failure patients with more severe diastolic dysfunction would need to be studied. The advent of echocardiographic STI has enabled reproducible noninvasive quantification of twisting motion (22,42,43). Cubic spline interpolation and normalization are mandatory to allow accurate subtraction of apical and basal data at the same time points (44), which makes the technique REFERENCES 1. Courtois M, Kovacs SJ Jr., Ludbrook PA. Transmitral pressure-flow velocity relation. Importance of regional pressure gradients in the left ventricle during diastole. Circulation 1988;78:661–71. 2. Firstenberg MS, Smedira NG, Greenberg NL, et al. Relationship between early diastolic intraventricular pressure gradients, an index of elastic recoil, and improvements in systolic and diastolic function. Circulation 2001; 104:I330 –5. 3. Cheng C, Igarashi Y, Little W. Mechanism of augmented rate of left ventricular filling during exercise. Circ Res 1992;70:9 –19. 4. Rovner A, Greenberg NL, Thomas JD, Garcia MJ. Relationship of diastolic intraventricular pressure gradients and aerobic capacity in patients with diastolic heart failure. Am J Physiol Heart Circ Physiol 2005;289:H2081– 8. 5. Streeter DD Jr., Spotnitz HM, Patel DP, Ross J Jr., Sonnenblick EH. Fiber orientation in the canine left ventricle for torsion analysis in the present study labor intensive. Automated analysis of torsion has recently been described (45) that will facilitate the translation of these parameters to clinical practice. CONCLUSIONS Untwisting is an important component of early diastolic function. Reduced untwisting in patients with abnormal diastolic function might attenuate suction gradients necessary for normal LV diastolic filling. Measurement of untwisting might provide a useful means to identify and quantify abnormal diastolic function in patients with normal ejection fraction. Acknowledgments The authors gratefully acknowledge Mr. Don Mooney for the acquisition of high-quality echocardiographic images. The authors thank Drs. Andrew McCann, Georg Leitl, and Anthony White for their assistance with cardiac catheterization in this study and Mr. Graham Hepworth, University of Melbourne Statistical Consulting Centre, for statistical advice. Reprint requests and correspondence: Dr. Andrew T. Burns, Cardiac Investigation Unit, St. Vincent’s Hospital, Melbourne, PO Box 2900, Fitzroy, Victoria, Australia, 3065. E-mail: [email protected]. during diastole and systole. Circ Res 1969;24:339 – 47. 6. Ingels NB Jr., Hansen DE, Daughters GT II, Stinson EB, Alderman EL, Miller DC. Relation between longitudinal, circumferential, and oblique shortening and torsional deformation in the left ventricle of the transplanted human heart. Circ Res 1989;64:915–27. 7. Rademakers FE, Buchalter MB, Rogers WJ, et al. Dissociation between left ventricular untwisting and filling. Accentuation by catecholamines. Circulation 1992;85:1572– 81. 8. Lester SJ, Tajik AJ, Nishimura RA, Oh JK, Khandheria BK, Seward JB. Unlocking the mysteries of diastolic function deciphering the Rosetta Stone 10 years later. J Am Coll Cardiol 2008;51:679 – 89. 9. Sengupta PP, Tajik AJ, Chandrasekaran K, Khandheria B. Twist mechanics of the left ventricle: principles and application. J Am Coll Cardiol Img 2008;1:366 –76. 10. Notomi Y, Martin-Miklovic MG, Oryszak SJ, et al. Enhanced ventricu- lar untwisting during exercise. A mechanistic manifestation of elastic recoil described by Doppler tissue imaging. Circulation 2006;113:2524 –33. 11. Dong SJ, Hees PS, Siu CO, Weiss JL, Shapiro EP. MRI assessment of LV relaxation by untwisting rate: a new isovolumic phase measure of tau. Am J Physiol Heart Circ Physiol 2001;281: H2002–9. 12. Wang J, Khoury DS, Yue Y, TorreAmione G, Nagueh SF. Left ventricular untwisting rate by speckle tracking echocardiography. Circulation 2007;116:2580 – 6. 13. Scalia GM, Greenberg NL, McCarthy PM, Thomas JD, Vandervoort PM. Noninvasive assessment of the ventricular relaxation time constant (tau) in humans by Doppler echocardiography. Circulation 1997;95:151–5. 14. Stuber M, Scheidegger MB, Fischer SE, et al. Alterations in the local myocardial motion pattern in patients suffering from pressure overload due to aortic stenosis. Circulation 1999; 100:361– 8. 715 716 Burns et al. Untwisting in Diastolic Function 15. Maier SE, Fischer SE, McKinnon GC, Hess OM, Krayenbuehl HP, Boesiger P. Evaluation of left ventricular segmental wall motion in hypertrophic cardiomyopathy with myocardial tagging. Circulation 1992;86:1919 –28. 16. Takeuchi M, Borden WB, Nakai H, et al. Reduced and delayed untwisting of the left ventricle in patients with hypertension and left ventricular hypertrophy: a study using two-dimensional speckle tracking imaging. Eur Heart J 2007;28:2756 – 62. 17. Appleton CP, Hatle LK, Popp RL. Demonstration of restrictive ventricular physiology by Doppler echocardiography. J Am Coll Cardiol 1988;11: 757– 68. 18. Paulus WJ, Tschope C, Sanderson JE, et al. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J 2007;28: 2539 –50. 19. Appleton CP, Hatle LK, Popp RL. Relation of transmitral flow velocity patterns to left ventricular diastolic function: new insights from a combined hemodynamic and Doppler echocardiographic study. J Am Coll Cardiol 1988;12:426 – 40. 20. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005;18:1440 – 63. 21. Notomi Y, Lysyansky P, Setser RM, et al. Measurement of ventricular torsion by two-dimensional ultrasound speckle tracking imaging. J Am Coll Cardiol 2005;45:2034 – 41. 22. Burns AT, La Gerche A, MacIsaac AI, Prior DL. Augmentation of left ventricular torsion with exercise is attenuated with age. J Am Soc Echocardiogr 2008;21:315–20. 23. Leitman M, Lysyansky P, Sidenko S, et al. Two-dimensional strain—a novel software for real-time quantitative echocardiographic assessment of myocardial function. J Am Soc Echocardiogr 2004;17:1021–9. 24. Nakai H, Takeuchi M, Nishikage T, Kokumai M, Otani S, Lang RM. JACC: CARDIOVASCULAR IMAGING, VOL. 2, NO. 6, 2009 JUNE 2009:709 –16 Effect of aging on twist-displacement loop by 2-dimensional speckle tracking imaging. J Am Soc Echocardiogr 2006;19:880 –5. 25. Weiss JL, Frederiksen JW, Weisfeldt ML. Hemodynamic determinants of the time-course of fall in canine left ventricular pressure. J Clin Invest 1976;58:751– 60. 26. Zile MR, Baicu CF, Gaasch WH. Diastolic heart failure—abnormalities in active relaxation and passive stiffness of the left ventricle. N Engl J Med 2004;350:1953–9. 27. Udelson JE, Bacharach SL, Cannon RO III, Bonow RO. Minimum left ventricular pressure during betaadrenergic stimulation in human subjects. Evidence for elastic recoil and diastolic “suction” in the normal heart. Circulation 1990;82:1174 – 82. 28. Senzaki H, Fetics B, Chen CH, Kass DA. Comparison of ventricular pressure relaxation assessments in human heart failure: quantitative influence on load and drug sensitivity analysis. J Am Coll Cardiol 1999;34:1529 –36. 29. Kasner M, Westermann D, Steendijk P, et al. Utility of Doppler echocardiography and tissue Doppler imaging in the estimation of diastolic function in heart failure with normal ejection fraction: a comparative Dopplerconductance catheterization study. Circulation 2007;116:637– 47. 30. Garcia MJ, Firstenberg MS, Greenberg NL, et al. Estimation of left ventricular operating stiffness from Doppler early filling deceleration time in humans. Am J Physiol Heart Circ Physiol 2001;280:H554 – 61. 31. Langer SF, Habazettl H, Kuebler WM, Pries AR. Estimation of the left ventricular relaxation time constant tau requires consideration of the pressure asymptote. Physiol Res 2005;54: 601–10. 32. Takeuchi M, Nishikage T, Nakai H, Kokumai M, Otani S, Lang RM. The assessment of left ventricular twist in anterior wall myocardial infarction using two-dimensional speckle tracking imaging. J Am Soc Echocardiogr 2007;20:36 – 44. 33. Garcia MJ, Thomas JD, Klein AL. New Doppler echocardiographic applications for the study of diastolic function. J Am Coll Cardiol 1998;32: 865–75. 34. Burkhoff D, Mirsky I, Suga H. Assessment of systolic and diastolic ventricular properties via pressure-volume analysis: a guide for clinical, translational, and basic researchers. Am J Physiol Heart Circ Physiol 2005;289: H501–12. 35. Marino P, Little WC, Rossi A, et al. Can left ventricular diastolic stiffness be measured noninvasively? J Am Soc Echocardiogr 2002;15:935– 43. 36. Kim HK, Sohn DW, Lee SE, et al. Assessment of left ventricular rotation and torsion with two-dimensional speckle tracking echocardiography. J Am Soc Echocardiogr 2007;20:45– 53. 37. Kass DA, Bronzwaer JG, Paulus WJ. What mechanisms underlie diastolic dysfunction in heart failure? Circ Res 2004;94:1533– 42. 38. Helmes M, Lim CC, Liao R, Bharti A, Cui L, Sawyer DB. Titin determines the Frank-Starling relation in early diastole. J Gen Physiol 2003; 121:97–110. 39. Helmes M, Trombitas K, Granzier H. Titin develops restoring force in rat cardiac myocytes. Circ Res 1996;79: 619 –26. 40. Bronzwaer JG, Paulus WJ. Matrix, cytoskeleton, or myofilaments: which one to blame for diastolic left ventricular dysfunction? Prog Cardiovasc Dis 2005;47:276 – 84. 41. Bell SP, Nyland L, Tischler MD, McNabb M, Granzier H, LeWinter MM. Alterations in the determinants of diastolic suction during pacing tachycardia. Circ Res 2000;87:235– 40. 42. Ashraf M, Li XK, Young MT, et al. Delineation of cardiac twist by a sonographically based 2-dimensional strain analysis method: an in vitro validation study. J Ultrasound Med 2006;25: 1193– 8. 43. Helle-Valle T, Crosby J, Edvardsen T, et al. New noninvasive method for assessment of left ventricular rotation: speckle tracking echocardiography. Circulation 2005;112:3149 –56. 44. Burns AT, La Gerche A, Prior DL, Macisaac AI. Re: Reduced and delayed untwisting of the left ventricle in patients with hypertension and left ventricular hypertrophy: a study using two-dimensional speckle tracking imaging. Eur Heart J 2008;29:825. 45. Borg AN, Harrison JL, Argyle RA, Ray SG. Left ventricular torsion in primary chronic mitral regurgitation. Heart 2008;94:597– 603. Key Words: diastole y echocardiography y speckle tracking imaging y torsion y untwisting.