* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download PDF - Circulation: Heart Failure
Quantium Medical Cardiac Output wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Echocardiography wikipedia , lookup
Pericardial heart valves wikipedia , lookup
Cardiac surgery wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Electrocardiography wikipedia , lookup
Aortic stenosis wikipedia , lookup
Atrial septal defect wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
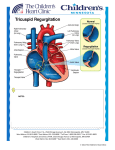
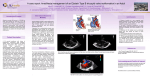
Images and Case Reports in Heart Failure Pacemaker Lead-Induced Severe Tricuspid Valve Stenosis Ruben Uijlings, MD; Jolanda Kluin, MD, PhD; Remy Salomonsz, MD, PhD; Mark Burgmans, MD; Maarten-Jan Cramer, MD, PhD A Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 10, 2017 73-year-old man had a DDD pacemaker implanted in 1991 for symptomatic high-degree atrioventricular block. Because of atrial lead dysfunction, a new atrial lead was implanted in 1998. Ten years later, the patient experienced unexplained ascites and edema with progressive exertional dyspnea, for which he was referred. Chest radiography showed a loop of the ventricular lead at the level of the tricuspid valve (Figure 1). Transthoracic echocardiography demonstrated an enlarged right atrium. The mean diastolic gradient across the tricuspid valve was 15 mm Hg with a peak pressure drop of 29 mm Hg without tricuspid regurgitation (Figure 2). No other abnormalities were found. Transesophageal echocardiogram revealed looping of one of atrial leads at the level of the tricuspid valve but could not visualize the exact anatomic position of the leads and the cause of the tricuspid valve stenosis (Figure 3). A cardiac computed tomography (CT) revealed 2 atrial leads in the right atrial free wall. However, the ventricular Figure 1. Chest radiography showed a loop of the ventricular lead at the level of the tricuspid valve. Received December 1, 2009; accepted February 16, 2010. From the Departments of Cardiology (R.U., M.J.C.), Cardiothoracic Surgery (J.K.), and Radiology (M.B.), University Medical Centre, Utrecht, The Netherlands; and Department of Cardiology (R.S.), Ruwaard van Putten Hospital, Spijkenisse, The Netherlands. Correspondence to Ruben Uijlings, MD, Department of Cardiology, University medical Center, Heidelberglaan 100, 3584 CX Utrecht, The Netherlands. E-mail [email protected] (Circ Heart Fail. 2010;3:465-467.) © 2010 American Heart Association, Inc. Circ Heart Fail is available at http://circheartfailure.ahajournals.org 465 DOI: 10.1161/CIRCHEARTFAILURE.109.928168 466 Circ Heart Fail May 2010 Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 10, 2017 Figure 2. Transthoracic echocardiography demonstrated severe tricuspid stenosis with a mean diastolic gradient across the tricuspid valve of 15 mm Hg with a peak pressure drop of 29 mm Hg. lead entered the ventricle through the tricuspid orifice, looped back into the atrium, surrounded the atrial leads, and ended in the apex of the right ventricle (Figure 4). The CT images showed that the right ventricular lead finally traversed the tricuspid level near the interventricular septum. Therefore, we suspected tricuspid valve perforation with secondary fibrosis. Pacemaker lead-induced severe tricuspid valve stenosis was diagnosed. At surgery, severe fibrosis with involvement of the valve leaflets was seen. As shown by CT, the right ventricular lead looped back from the ventricle into the atrium, then encircled one atrial lead against the septal leaflet (Figure 5). It was not sure whether the lead had perforated the septal cusp or the abundant fibrosis surrounding the lead and tricuspid valve mimicked valve perforation. The pacemaker leads and the tricuspid valve were excised, and a porcine bioprosthetic Figure 3. Transesophageal echocardiogram revealed looping of one of atrial leads at the level of the tricuspid valve. Uijlings et al Lead-Induced Severe Tricuspid Valve Stenosis 467 Figure 4. Cardiac CT revealed two atrial leads in the right atrial free wall. The ventricular lead entered the ventricle, looped back into the atrium, surrounded the atrial leads, and ended in the apex of the right ventricle. Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 10, 2017 Figure 5. Perioperative photography and illustrative picture of the surgical view showing the proximal right ventricular lead (blue) entering the right ventricle through the stenosed tricuspid ostium. The distal right ventricular lead looped back into the atrium outside the tricuspid ostium and encircled one atrial lead before re-entering the right ventricle outside the ostium. tricuspid valve was implanted. Additionally, epicardial leads were placed. Histology showed fibrosis without signs of active endocarditis. Postoperative echocardiography showed a mean gradient of 4 mm Hg across the bioprothesis without regurgitation. The patient’s recovery was uneventful; and within 2 weeks, he had better exercise tolerance. Severe tricuspid valve stenosis due to pacemaker leads is uncommon. We present a case of iatrogenic tricuspid valve stenosis with fibrosis. Tricuspid valve stenoses secondary to transvenous leads are reported to be treated with surgical replacement,1,2 surgical valvuloplasty,1 or percutaneous balloon valvuloplasty.3 Cardiac CT can provide supportive evidence of the anatomic mechanism of valve dysfunction and planning of treatment strategy. Acknowledgments We thank Ingrid Janssen for her technical assistance. Disclosures None. References 1. Heaven DJ, Henein MY, Sutton R. Pacemaker lead related tricuspid stenosis: a report of two cases. Heart. 2000;83:351–352. 2. Krisnan A, Moulick A, Sinha P, Kuehl K, Kanter J, Slack M, Kaltman J, Mercader M, Moak JP. Severe tricuspid valve stenosis secondary to pacemaker leads presenting as ascites and liver dysfunction: a complex problem requiring a multidisciplinary therapeutic approach. J Interv Card Electrophysiol. 2009;24:71–75. 3. Hussain T, Knight WB, McLeod KA. Lead-induced tricuspid stenosissuccessful management by balloon angioplasty. Pacing Clin Electrophysiol. 2009;32:140–142. Pacemaker Lead-Induced Severe Tricuspid Valve Stenosis Ruben Uijlings, Jolanda Kluin, Remy Salomonsz, Mark Burgmans and Maarten-Jan Cramer Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 10, 2017 Circ Heart Fail. 2010;3:465-467 doi: 10.1161/CIRCHEARTFAILURE.109.928168 Circulation: Heart Failure is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 2010 American Heart Association, Inc. All rights reserved. Print ISSN: 1941-3289. Online ISSN: 1941-3297 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://circheartfailure.ahajournals.org/content/3/3/465 Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Circulation: Heart Failure can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Circulation: Heart Failure is online at: http://circheartfailure.ahajournals.org//subscriptions/