* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
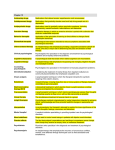
Download There are many reasons for an assessment for your - SPED
History of psychiatric institutions wikipedia , lookup
Separation anxiety disorder wikipedia , lookup
Mental status examination wikipedia , lookup
Pyotr Gannushkin wikipedia , lookup
Mentally ill people in United States jails and prisons wikipedia , lookup
Mental disorder wikipedia , lookup
Factitious disorder imposed on another wikipedia , lookup
Community mental health service wikipedia , lookup
Diagnostic and Statistical Manual of Mental Disorders wikipedia , lookup
Deinstitutionalisation wikipedia , lookup
Controversy surrounding psychiatry wikipedia , lookup
Classification of mental disorders wikipedia , lookup
History of psychiatry wikipedia , lookup
Causes of mental disorders wikipedia , lookup
Child psychopathology wikipedia , lookup
Mental health professional wikipedia , lookup
Depression in childhood and adolescence wikipedia , lookup
History of mental disorders wikipedia , lookup
Assessment Guide compiled by: Jeffrey B. Moore, Ed.S., L.C.S.W. IInnttrroodduuccttiioonn There are many reasons for an assessment for your child. The underlying drive for any assessment is a concern regarding your child’s ability or performance in a given area. Whatever the area may be, you are not alone. This guide is not exhaustive, but instead serves as a starting point to provide the information necessary to assist educators and parents and clarify the assessment process. Included are the most common types of assessments and disorders, a description of appropriate assessment personnel and service providers, as well as preventive care. It is compiled from a variety of sources and includes many links to other relevant resources. Credit to the sources is indicated throughout the text. These may be found already posted on the Sevier County Special Education website (www.sevier.org), along with many others. However, the guide is a collection of those most relevant to assessments and disorders that occur more frequently, as well as a description of the assessment process. If you need further information on a specific problem, please consult the resources provided in the back of the guide. Before beginning the assessment process, it is important to first talk about your concerns with your child’s teachers, counselors, and others with knowledge of your child. After consulting with these key people in your child’s life, an intervention plan may be developed that appropriately addresses the need without needing to proceed further. However, if the problems persist or worsen, an assessment may be indicated. 2 INDEX Page 4: Types of Assessments Page 16: Common Childhood Mental Health Symptoms & Disorders Page 30: Assessment & Service Providers Page 32: Medications & Related Questions For Common Problems Page 35: Preventive Care/Schools Helping Page 47: Warning Signs & Frequently Asked Questions Page 49: National Contact Numbers Page 50: School Psychology Services in Sevier County Schools Page 65: References & Resources 3 Types of Assessments (APA 1-4, 6-11) (NASP 5a. & 5b.) 1. Child Neuropsychological - A neuropsychological assessment is an evaluation of how a child’s brain and nervous system affect his or her thinking and behaviors. Several ways of gathering information such as through interviews with the child and parents, formal observations, and neuropsychological testing are used to assess a child’s physical, social, psychological, and neurocognitive development. 2. Developmental Pediatric - A developmental pediatric assessment is an evaluation of a child’s developmental level and health. Through testing, observations, and interactions with the child and parents, a developmental pediatrician, who has special training in assessing children and adolescents, gathers and provides information about a child’s development and ageappropriate behaviors. 3. Educational - An educational assessment is an evaluation of a child’s skills related to academic success. Typical areas of assessment include language, reading, writing, and math. In addition, educational assessments often include testing of a child’s processing skills and include tests such as auditory memory and visual perception. 3a. Special Education Evaluation (Jeff Moore) If a problem is suspected by family and/or school personnel, begin by consulting with those most familiar with the student. Often it is possible to make the necessary adjustments or accommodations without an evaluation. 4 Allow any modifications or interventions the appropriate amount of time in order to determine their effectiveness. Strategies incorporated within Response-To-Intervention (RTI) typically have predetermined time periods and proceed to the appropriate intervention tier accordingly. If problems persist, an evaluation may be necessary. This begins with an explanation of the area or areas under consideration, signed permission by the parent or guardian, and the provision and explanation of their rights and the evaluation process. From that time, the evaluation is completed within 40 school days. Once an evaluation is completed, the members of the evaluation team reconvene to review the results. In order to be certified as eligible for special education services, the student must meet the appropriate criteria and also have the following factors ruled out as the primary cause of the disability. These include a lack of instruction in reading or mathematics, limited English proficiency, or a disadvantage either environmentally, socially, or culturally. An accompanying requirement is the inability to meet student needs in the general education curriculum without special education services. There must be documentation regarding how the disability adversely affects educational performance in the classroom. If these conditions are met, the student may be certified as eligible for special education services, at which time an IEP would be developed. Members of the evaluation team typically include the parent or guardian, the general education teacher, assessment specialist, special education teacher if appropriate, and also the student when appropriate. 4. Functional Behavioral - A functional behavioral assessment is an evaluation of the underlying cause or reason for a certain behavior and/or set of behaviors. A functional behavioral assessment examines the behavior itself, but also looks at the broader scope, to find out what factors are causing and/or maintaining a behavior. It is especially important to identify the social, affective, cognitive, and environmental factors associated with the occurrence of the behavior. 5 5a. Mental Health Assessment (NASP) A mental health assessment gives your doctor an overall picture of how well you feel emotionally and how well you are able to think, reason, and remember (cognitive functioning). Your doctor will ask you questions and examine you. You might answer some of the doctor's questions in writing. Your doctor will pay attention to how you look and your mood, behavior, thinking, reasoning, memory, and ability to express yourself. Your doctor will also ask questions about how you get along with other people, including your family and friends. Sometimes the assessment includes lab tests, such as blood or urine tests. A mental health assessment may be done by your primary care doctor or by a psychiatrist or psychologist. A mental health assessment for a child is geared to the child's age and stage of development. Purpose (Why it is Done) A mental health assessment is done to: Find out about and check on mental health problems, such as anxiety, depression, schizophrenia, Alzheimer's disease, and anorexia nervosa. Help tell the difference between mental and physical health problems. Evaluate a person who has been referred for mental health treatment because of problems at school, work, or home. For example, a mental health assessment may be used to find out if a child has learning disabilities or behavior disorders such as attention deficit hyperactivity disorder (ADHD), conduct disorder (CD), or obsessivecompulsive disorder (OCD). 6 Check the mental health of a person who has been placed in an institution or arrested for a crime, such as drunken driving or physical abuse. How to Prepare If you are having a mental health assessment because you have specific symptoms, you may be asked to keep a diary or journal for a few days before your appointment. A family member or friend may be able to describe your symptoms better than you can. If possible, bring that person with you to your appointment. If your child is being checked for behavior problems, you may be asked to keep a diary or journal of how he or she acts for a couple of days. Your child's teacher may need to answer questions about how your child acts at school. Many medicines can cause changes in your ability to think, reason, and remember. Be sure to tell your doctor about all the nonprescription and prescription medicines you take. Talk to your doctor about any concerns you have regarding the need for the test, its risks, how it will be done, or what the results will indicate. How it is Done Health professionals often do a brief mental health assessment during regular checkups. If you are having symptoms of a mental health problem, your doctor may do a more complete assessment or refer you to another doctor, such as a psychologist or psychiatrist. A mental health assessment includes an interview with a doctor and may also involve a physical exam and written or verbal tests. Interview During the interview, your doctor pays attention to how you look (for example: Are you standing up straight? Are your shoes tied? Are you neat and clean?), how you move, what type of mood you seem to be in, and how you behave. You will be asked to talk about your symptoms and complaints. Be as 7 detailed as possible. If you have kept a diary or journal of your symptoms, share this with your doctor. Your doctor may ask you questions to check how well you think, reason, and remember (your cognitive functioning). He or she may ask you questions to find out how you think, how you feel about life, and whether you are likely to commit suicide. Physical exam A mental health assessment may include a physical exam. Your doctor will review your past medical history, as well as that of your family members, and the medicines you currently take. Your doctor may test your reflexes, balance, and senses, such as hearing, taste, sight, smell, and touch. Lab tests The mental health assessment sometimes includes lab tests on a blood or urine sample. If a nervous system problem is suspected, tests such as magnetic resonance imaging (MRI), electroencephalogram (EEG), or computed tomography (CT) may be done. Lab tests to detect other problems may include thyroid function tests, electrolyte levels, or toxicology screening (to look for drug or alcohol problems). Written or verbal tests A mental health assessment may include one or more verbal or written tests. You will be asked some questions and will either answer out loud or write your answer on a piece of paper. Your answers are then rated and scored by your doctor. Written questionnaires generally contain 20 to 30 questions that can be answered quickly, often in a "yes" or "no" format. They usually don't take long to finish, and you can do them by yourself at a regular office visit. 8 Many mental health questionnaires are available. They look at: Specific problems. For example, for depression, the Hamilton Rating Scale for Depression, the Beck Depression Inventory, or the Geriatric Depression Scale can be used to evaluate your symptoms. How well you are able to think, reason, and remember (cognitive function). The Mini Mental State Examination can be used to check your cognitive function. How well you are able to carry out routine activities, such as eating, dressing, shopping, or banking. Sometimes a more extensive mental health test, such as the Wechsler Adult Intelligence Scale, may be needed. The test may need to be given by a specialist such as a psychologist. 5b. What is clinical assessment? (NASP) Mental health clinical assessment (sometimes called "whole person assessment") is the process of gaining a better understanding of an individual’s concerns, needs, and strengths. A thorough clinical assessment helps the consumer and his family make more informed decisions. The referral question shapes the goals and methods of clinical assessment. The referral question can come from the consumer, her family, or the referring service provider. It is why assessment is being sought at this time. Here are some examples of referral questions: How can we reduce aggressive behavior towards classmates? OR, How can he interact more positively with his classmates? When this young adult says he hears voices, is it due to concrete thinking associated with his mental retardation, or is he experiencing auditory hallucinations (hearing things that aren’t really there)? Does this teenager’s severe anxiety about going to his new high school have any connection with his cerebral palsy? Can this child understand the material being presented in her current classroom placement? Is this young woman really a neglectful mother, or does she have moderate mental retardation and need homemaking support services? Does my child have autism? 9 As you can see, the referral question and the process of trying to address that question is at the heart of all clinical assessment. How is clinical assessment different than diagnosis? Diagnosis is a shorthand method of providing information about an individual. It describes the person’s current problems in terms of symptoms. However, a diagnosis alone does not provide the unique aspects of the individual that are necessary to plan interventions and supports. For instance, the medical diagnosis of anxiety disorder gives us an idea of the condition the person is struggling with. But it does not tell us many other important things, such as: severity of the mental illness current types of treatment (psychotherapy, medications, Yoga) being used level of impairment from the illness or treatment. (How much does the anxiety impair the person’s daily functioning?) other important life stressors (financial problems, medical illness, recent death in the family, etc.) A diagnosis does not convey the person’s unique personality, strengths, and positive attributes. Diagnoses highlight deficit and do not focus on adaptive abilities, other skills, talents, and interests. All of this information is important for mental health assessment and treatment. How is clinical assessment performed? Comprehensive clinical assessment cannot be completed in one session. It usually takes several visits. Good clinical assessment has four phases: 1. Helping the consumer/family articulate their question(s). 2. Choosing and conducting assessment procedures to obtain the most relevant information. 3. Integrating (combining) all the findings from the past and present clinical assessments. 4. Providing understandable information and practical recommendations to the consumer, family, and relevant professionals and careproviders. 10 During this process, the values, knowledge, skills, and experience of the mental health clinician are paramount, because each phase requires careful and complex judgments. The results of the assessment process will heavily depend upon the clinician’s competence. How does the mental health professional gather pertinent information? There are many kinds of information-gathering techniques. But all techniques reflect one of these four formats for obtaining information about the consumer: a. b. c. d. a. Ask the person himself. Ask someone who knows the person. Observe the person as she behaves in her natural environment. Observe the person in a standardized test situation. Ask the person himself. The backbone of clinical assessment is asking a person direct questions and trying to obtain accurate replies. Questions can range from the most obvious (such as name, age, number of siblings) to more abstract (such as feelings, thoughts, preferences, and intentions). The process of asking questions in a systematic way is called an interview. [See Interviews & History module.] Questions can be asked in a face-to-face interview or in written questionnaires. Questionnaires (also called "surveys," "scales," and "self-report instruments") are simple, consistent, and cost-effective. However, human nature leads many of us to alter our answers to present ourselves in the best possible light. Individuals with developmental disabilities and mental illness face an additional hurdle. The consumer with this dual diagnosis has both cognitive and emotional challenges (and perhaps physical as well) that make questionnaires difficult to use. For instance, the mental age of an adult with mental retardation should be considered when using questionnaires. [See Mental Health Assessment Tools module.] 11 b. Ask someone who knows the person. This format is very useful for all individuals, but especially those with communication impairments. Family members are a good source of information, along with other careproviders, Regional Center service coordinators, teachers, physical or occupational therapists, and others. Sometimes friends and neighbors are available to participate in the clinical assessment process. These additional informants should not be overlooked because they can be rich sources of information. They often see the individual over a long period of time and have the perspective to help the mental health clinician understand the difference between the consumer’s typical behavior versus unusual behavior. They can describe the individual’s behavior, personality characteristics, strengths, preferences, and other factors that appear to affect his mood and social behavior. They can also point out factors that may not be obvious to the clinician. For instance, a teacher may notice that time of day or noise level affects a student’s learning and behavior, factors that the clinician may not have considered on his own. Also, by obtaining information from various sources, the clinician can began to identify whether certain difficulties are consistent across settings or not, and if not, what factors contribute to the successes and difficulties. Of course, the clinician may only talk to outside individuals with the specific permission of the adult consumer or parent of a child consumer. c. Observe the person as she behaves in her natural environment. Directly observing a person over the course of a day is one of the best ways to obtain information. However, this is an expensive method (cost of the clinician’s time), it is sometimes impractical (the consumer may live too far away), and it may jeopardize the consumer’s or other individuals’ confidentiality. Despite these obstacles, every effort should be made to observe the consumer at home or school, however briefly. Assessments should be planned to include activities that are successful and comfortable as well as problematic or distressing. 12 Direct observation helps the clinician discover problem factors that might have gone unidentified by other informants. For example, a parent may not realize that her son becomes aggressive because he doesn’t have the language to communicate his feelings. He may have tried to get his mother’s attention by tugging at her sleeve, but she may have interpreted this gesture as "bothering" her instead of being an attempt at communication. The child’s next step might be to hit her to get her attention. Conversely, a child may be extremely anxious but the mother may not note it to the clinician during the interview because she believes that "this is how he has always been" and considers the behavior to be "just his personality." d. Observe the person in a standardized test situation. Despite their limitations, standardized tests, especially in combination with interviewing, remain the major method of assessment for most mental health clinicians. The essential features of tests are: Standard conditions are maintained during testing (that is, the test materials and clinician’s approach are very similar for all consumers taking the test). This reduces subjective bias. They are time-efficient for the clinician. They provide quantitative measures (a score expressed in numbers or percentages, or age-equivalence) to describe various types of functioning or symptoms (such as intelligence, depression, or thought disorder). Scores are convenient for comparing this individual with others. Scores can sometimes provide evidence of the mental illness improving or worsening over time. One of standardized testing’s major limitations is that many of them are inappropriate for individuals with developmental disabilities. When selecting a clinician, it is important to consider his or her competence in selecting the most appropriate tests for such a consumer. Due to time and funding constraints, clinical assessments may be very limited. However "shortcuts" in the assessment phase often cause poor choices in the treatment process. Most mental health professionals recognize that a thorough clinical assessment is essential for effective and efficient mental health intervention. 13 Credits Author Jeannette Curtis Editor Susan Van Houten, RN, BSN, MBA Associate Editor Michele Cronen Primary Medical Reviewer Kathleen Romito, MD - Family Medicine Specialist Medical Reviewer Donald Sproule, MD, CM, CCFP, FCFP - Family Medicine Last Updated December 24, 2007 Author: Medical Review: Jeannette Curtis Last Updated: December 24, 2007 Kathleen Romito, MD - Family Medicine Donald Sproule, MD, CM, CCFP, FCFP - Family Medicine © 1995-2008 Healthwise, Incorporated. Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Healthwise, Incorporated. This information does not replace the advice of a doctor. Healthwise disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. How this information was developed to help you make better health decisions. (6-11, NASP) 6. Occupational - An occupational assessment is an evaluation of a person’s ability to perform everyday tasks. Pediatric occupational therapists assess and compare a child to other children their age in their abilities to perform developmental tasks such as in their skills for play and academics. 7. Pediatric Neurological - A pediatric neurological assessment, conducted by a pediatric neurologist, is an evaluation of a child’s vital signs, reflexes (i.e. eye movements, motor responses), balance and coordination, muscle strength and movement, and level of consciousness (i.e. mental status). The assessment includes a physical exam, an interview, and specific diagnostic tests. This kind of testing can lead to a diagnosis about problems with the structure or functioning of specific parts of the nervous system. 8. Physical Therapy - A physical therapy assessment is an evaluation of a child’s ability to move. An assessment might include an examination of a 14 child’s ability to walk, sit, and run. A pediatric physical therapy assessment might compare a child’s ability to developmental milestones that are typically reached at certain ages. 9. Psychiatric - A psychiatric assessment is an evaluation conducted by a psychiatrist that assesses a child’s mental health and level of functioning. The assessment can include several ways of gathering information such as through interviews and direct observations of a child’s feelings, thoughts, and perceptions. With this information an accurate diagnosis and treatment suggestions, including recommendations for medication, can be made. 10. Psychological - A psychological assessment is an evaluation of a child’s mental health and level of functioning. Assessments can include interviews, testing, and other ways of gathering information. The information that is gathered is used to make accurate diagnoses and make recommendations for improving a child’s situation and/or level of functioning. 11. Speech/Language - A speech and language assessment, conducted by speech and language therapists, is an evaluation of a child’s ability to speak and communicate. Assessments can include formal and informal measures of how a child understands language, uses language, and articulates speech. Speech and language therapists may also examine how a child chews, swallows, and eats in order to better understand any problems with speech. 15 Common Childhood Mental Health Symptoms & Disorders (APA) The following section provides an overview of common childhood disorders and conditions. The information is not intended to serve as a guide for diagnosing children. It is critically important that a comprehensive evaluation by trained professionals be conducted to assess children’s symptoms. Anxiety Mood Disorders Speech/Language Problems Auditory Processing Disorder (APD) Attention Deficit/Hyperactivity Disorders (ADHD) Learning Disabilities Asperger’s Disorder Autism Mental Retardation 1. Anxiety Disorders Anxiety is the most commonly referred problem to child mental health clinics. Symptoms of anxiety in children may include: Excessive worrying and distress Restlessness, tiredness, shakiness, muscle tension Rapid heartbeat, shortness of breath, dizziness, dry mouth, nausea, diarrhea Feeling constantly on edge, concentration difficulties, trouble falling or staying asleep, a general state of irritability Fears that affect other areas of the child’s and the family’s daily life Excessive anxiety or worry due to a parent’s threat of abandonment or friction between parents. 16 Symptoms of anxiety are commonly seen in neuro-developmental disorders. For example, children with Tourette’s Syndrome display chronic motor (e.g., eye blinking, head jerking), and/or vocal (e.g., sniffing, throat clearing) tics also experience obsessions and compulsions, generalized anxiety, hyperactivity, impulsivity, psychological rigidity, and distractibility. Likewise, children with Asperger’s Disorder often display social skills problems (e.g., poor eye contact, lack of social or emotional reciprocity, psychological rigidity, and repetitive motor movements) and anxiety. Some children and adolescents experience persistent anxiety that can occur in the presence or absence of stressful events. It is often expressed in somatic complaints (e.g., inability to relax, muscle tension, stomachaches, headaches) and frequent worries (e.g., school, family, and friends). Children who display more severe levels of anxiety may develop a specific Anxiety Disorder. Examples may include phobias and anxiety disorders such as Social Anxiety, Separation Anxiety, Panic Disorder, Obsessive-Compulsive Disorder, and Generalized Anxiety Disorder. 1a. Phobias - Children and adolescents fear and often avoid specific objects and/or situations. The most common phobias involve animals (e.g., dogs, cats, insects), being alone, taking tests, doctors/dentists, bloodtests, darkness, thunder/lightning and forms of transportation (e.g., cars, buses, trains, planes). 1b. Social Anxiety - Children and adolescents with social anxiety frequently avoid situations in which their actions may be observed by others for fear that they will be embarrassed or humiliated. Commonly avoided situations include speaking in front of others, eating in public places, going to parties and using public bathrooms. 1c. Separation Anxiety - Some children and adolescents experience persistent anxiety when separating from major attachment figures (e.g., parents). Children often worry that their parents will be harmed (e.g., car accident), or that they themselves will be kidnapped or become the victim of an accident. Often children are unable to sleep alone and will avoid being alone at all times. School-related difficulties (e.g., school refusal behavior) may involve fears related to attending school, interacting with teachers, and/or peer-related issues. 17 1d. Panic Disorder - Some children and adolescents experience a sudden rush of intense fear or anxiety in the absence of stressful events (i.e., totally out of the blue). Common physical symptoms include difficulty breathing, palpitations, dizziness, shaking, and the feeling of losing control or going crazy. 1e. Obsessive-Compulsive Disorder - Some children and adolescents experience obsessions and/or compulsions. Obsessions are persistent ideas or images that are intrusive and not useful. Compulsions are repetitive behaviors that are intended to prevent or correct discomfort or some dreaded event. The most common obsessions are repetitive thoughts of violence, contamination, and self-doubt. The most common compulsions are cleaning and checking rituals as well as trichotillomania (i.e., pulling out one’s hair, eyelashes, or eyebrows). 1f. Generalized Anxiety Disorder – Some children and adolescents experience general feelings of fearfulness that affect multiple aspects of their lives including school, home, and daily activities. 2. Mood Disorders Depression is another commonly referred problem to child mental health clinics. Depressed children may experience sadness, irritability, lack of interest in previously enjoyed activities, and changes in sleep or eating habits. Children may display mild and ongoing depressive symptoms, or more severe and acute levels of depression. Children or adolescents who experience more chronic or severe levels of depression may be diagnosed with a Mood Disorder. Symptoms of mild and acute types of depression in children may include: * * * * * * A sad or flat facial expression A preoccupation with the subject of death Suicidal thoughts and/or actions Isolation from family and/or peers Refusal to communicate openly Use of street drugs to alleviate mood * Poor eye contact * Irritability * Changes in appetite * A drop in grades * Changes in sleep patterns * Low energy level 18 * * * * * Low self-esteem (i.e. telling self “I’m not good enough” or “I’m not worth it”) Feelings of hopelessness (i.e. telling self “Things will never get better”) Poor concentration and difficulties in decision making A lack of interest in previously enjoyed activities Feeling excessive guilt or unresolved grief. What is Depression? (NASP) (Principal Leadership Magazine, Vol. 4, Number 2, October 2003) Counseling 101 Column, When It Hurts to Be a Teenager Depression is not a personal weakness, a character flaw, or the result of poor parenting. It is a mental illness that affects the entire person, changing the way he or she feels, thinks, and acts. A depressive disorder, sometimes referred to as clinical depression, is generally defined as a persistent sad or irritable mood as well as "anhedonia," a loss of the ability to experience pleasure in nearly all activities. It is more than just feeling down or having a bad day, and it is different from normal, healthy feelings of grief that usually follow a significant loss, such as a divorce, a break up with a boyfriend or girlfriend, or the death of a loved one. How Does It Differ From Moodiness? Depressed teens can experience a range of symptoms including change in appetite, disrupted sleep patterns, increased or diminished activity level, impaired concentration, and decreased feelings of self-worth. Adolescents are often more defiant and oppositional than depressed adults. Symptoms can manifest themselves in school as behavior problems, lack of attention in class, an unexplained drop in grades, cutting class, dropping out of activities, or fights with or withdrawal from friends. These behaviors are distinguished from normal teenage behavior by their duration, intensity, and the degree of dysfunction they cause. Symptoms or behaviors that last longer than two weeks, are markedly out of proportion to an event or situation, and impair a student's academic or social performance are cause for professional evaluation. Although episodes of clinical depression are sometimes self-limiting (meaning that a student may appear to get better), depressed teens cannot just "snap out of it" on their own and are likely to experience further episodes in the future. 19 What Characterizes Depression and Other Mood Disorders? Children or adolescents who experience more chronic or severe levels of depression may be diagnosed with a Mood Disorder, such as one of the following: Depression, like adolescents themselves, comes in all shapes and sizes. Teens can suffer from a variety of depressive disorders, sometimes called mood disorders. These can include: 2a. Adjustment disorder – an extremely intense reaction to life stressors that is in excess of what would ordinarily be expected and can be dangerous, but usually does not become chronic; dysthymic disorder or mild, chronic depression-a few or milder symptoms occurring either continuously or most of the time for a year or more, but with relatively good functioning 2b. Major depressive disorder - a severe, serious condition characterized by extreme depressive symptoms including hopelessness, lethargy, feelings of worthlessness or unrealistic guilt, and recurrent thoughts of death suicidal plans or suicidal attempts 2c. Bipolar disorder - severe moods swings from depressive depths to unrealistic and uncharacteristic elation, grandiosity, behavioral excesses, verbosity, or belligerence. 2d. Dysthymia – when children and adolescents experience more ongoing (i.e., every other day), yet less severe symptoms of depression. Teens who exhibit symptoms of a depressive disorder should be referred for a mental health evaluation. They should not be left alone if they are suspected of being suicidal. Depression in teens may also be masked by other problems or behaviors, such as anxiety disorder, frustration over learning problems, sexual promiscuity, and substance abuse. Depressed adolescents often self-medicate or seek thrills to alleviate their pain. Some seek relief through self-injury, such as cutting or extreme physical risk-taking. Students who are identified as engaging in these behaviors should be referred for depression screening at once. 20 What Are the Risk Factors? Depression does not discriminate, but there are certain risk factors that predispose adolescents to depressive disorders. Clinical depression usually has a genetic component, and those who have a family history of depression, particularly among close relatives, are more vulnerable. More than half the teens who are diagnosed with a depressive disorder have one or more coexisting mental disorders, so those who already have emotional or behavior problems are at greater risk. Other risk factors include poverty; being female; low self-esteem; uncertainty about sexual orientation; poor academic functioning; poor physical health; ineffective coping skills; substance abuse; and frequent conflicts with family, friends, and teachers. In addition, students who have experienced significant trauma or abuse, are bullied, or do not feel welcome or accepted at school are much more susceptible to depression. Facts About Depression Depression is a treatable medical illness, not just a bad mood or an inevitable part of life’s ups and downs. Depression affects 8-10% of adolescents and is the most common cause of disability in the United States. Depression in teens differs from depression in young children or adults. Teens are more affected by their social environment, more irritable than sad, and more chronically depressed. Depression affects people of all ages and backgrounds. However, postpubescent girls are twice as likely to suffer from serious depression than boys, and certain populations, such as gay and bisexual youths and American Indians, suffer higher rates of depression. Untreated depression is the leading risk for suicide among adolescents. Suicide is the third leading cause of death among adolescents ages 1524 and the fourth leading cause of death among children ages 10-14. Nearly 2,000 young people die of suicide every year; nearly 400,000 attempt suicide; nearly 2 million make a suicide plan. Girls are twice as likely to attempt suicide but boys are 10 times more likely to succeed because they tend to choose more lethal methods of attempting suicide (e.g. guns). 21 Depression can be linked to poor academic performance, poor social relationships, school absenteeism, dropping out, disruptive behavior, and school violence. Depressive episodes can resolve themselves but, if ignored, are likely to reoccur within a year. Talking to friends or family is an important source of support but on its own is not enough to treat depression. Nearly 70% of children and youth with serious mental health problems do not get treatment. Eighty percent of people treated for depression respond to treatment, which usually includes a combination of medication, psychotherapy, and support groups. Identifying Depression Distinguishing depression from adolescents’ normal mood swings can be difficult. School staff members should contact a mental health professional if a student exhibits symptoms that: Are new or changed in intensity, frequency, or manifestation Continue for a two or more weeks Interfere with the student’s social and academic function Cause disruptive or uncontrolled behavior Reflect thoughts of hurting oneself or others Warning Signs of Depression in Adolescents Sadness, depressed mood, or irritability Lack of pleasure in daily activities Withdrawal or crying Unexplained physical complaints Lethargy or chronic boredom Poor concentration or inability to make decisions Poor academic performance Negative thoughts about self, the world, and the future Self-blame, guilt, and failure to recognize one’s success Change in appetite or weight gain or loss Excessive sleeping 22 Increased-risk behaviors (e.g., sexual risk-taking or abuse of drugs and alcohol) Suicide ideation or attempts Risk Factors for Depression Existing or history of mental health problems Poor academic functioning Poor physical health Poor coping skills or social skills Low self-esteem Behavior problems Problems with friends or family Poor school and family connectedness Major life stressors Substance abuse Family history of depression or suicide Warning Signs of Suicide Risk Untreated depression is the leading risk for suicide in adolescents. Four out of five youths who attempt suicide give clear indications of their intentions. Warning signs include: Suicide notes, threats, and references either verbal or expressed in writing or creative work Previous attempts Obsession with death Depression or other disturbed mood or behavior Risk-taking behaviors, such as aggression, reckless driving, gunplay, and alcohol or substance abuse Efforts to hurt oneself (e.g., cutting oneself or jumping from heights) Inability to concentrate or think rationally Changes in physical habits (e.g., sleeping or eating) and appearance (e.g., hygiene and dress) Sudden changes in personality (e.g., sadness or irritability), friends (e.g., withdrawal or isolation), or behaviors (e.g., loss of interest, absenteeism, or drop in grades) Making final arrangements (e.g., a will) or giving away belongings 23 Suicide plan (i.e., specific talk or allusions to timing and method) and access to method (e.g., guns or prescription drugs) Copyright 2003 National Association of Secondary School Principals. Produced in cooperation with the NASP. 3. Health Related (APA) 3a. Asperger's Disorder Children and adolescents with Asperger’s Disorder commonly display impairments in social functioning, repetitive behaviors or body movements (e.g., hand or finger flapping), and a tendency to focus on a narrow range of interests. If these disturbances cause significant impairment in important areas of functioning, such as in school or with friends and family, the child may be diagnosed as having Asperger’s Disorder. Symptoms of Asperger’s Disorder may include: An inability to use more than one nonverbal behavior (e.g., eye contact, facial expression, body postures and gestures) to communicate and interact with others A tendency to develop relationships that are age-inappropriate (i.e. with younger children) A consistent failure to show or point out objects they find interesting A lack of participation in play with others, preferring to play alone, or involving others in activities only as tools Starting conversation topics regardless of others’ reactions. 3b. Autism Autistic Disorder is characterized by abnormal development in the areas of social interaction and communication, and by having a restricted range of activities and interests. Autistic children and adolescents experience a pervasive lack of interest in or responsiveness to other people. Other symptoms of Autistic Disorder may include: A tendency to develop relationships that are age-inappropriate (i.e. with younger children) 24 A lack of spontaneity and emotional or social reciprocity Significant delays in or total lack of spoken language development Impairment in sustaining or initiating conversation Oddities in speech and language (i.e. repeating phrases made by another person, using "you" instead of "I" or "me" when referring to one's self, or using metaphors to create a sublanguage) Having strict routines or rituals (e.g., taking exactly the same route to school every day) An extreme resistance to or overreaction to minor changes in routine or environment Repetitive hand movements (e.g., clapping, finger flicking) or body motions (e.g., rocking, head rolling, swaying) Unusual body postures or movements (e.g., walking on tiptoe, not swinging hands properly when walking) A preoccupation with objects and/or narrow areas of interest (e.g., pieces of string, body parts, weather reports, certain numbers) Having a narrow range of emotions and facial expressions Uneven intellectual and cognitive functioning (i.e., can do some things better than most people; cannot do other things at all) Engaging in self-injurious behaviors (e.g., head banging and biting oneself). 3c. Attention Deficit/Hyperactivity Disorders (ADHD) ADHD, a neuro-developmental disorder takes the form of developmentally inappropriate inattention, impulsivity, and/or hyperactivity. There are three types of ADHD: (1) ADHD Predominately Inattentive Type, (2) ADHD Predominately Hyperactive-Impulsive Type, and (3) ADHD Combined Type. Children with ADHD disorder tend to exhibit: Inattention and distractibility A tendency to complete schoolwork and/or homework inconsistently 25 Consistent failure to follow through on instructions or chores in a timely manner Forgetfulness Restlessness Difficulties taking turns in group situations Excessive talking, blurting out answers, and intruding into other people’s business A tendency to engage in aggressive attention-seeking behaviors Participation in careless or likely dangerous activities Failure to learn from experience and often blaming others for problems Low self-esteem and poor social skills. 4. Speech/Language Problems Speech and language problems are also common developmental problems in children. An indication of this type of problem can be when the child’s speech and/or language is developing substantially below the expected level for the child’s age, level of intelligence, and education. Examples of speech problems include difficulties producing sounds in syllables. Children and adolescents may mispronounce words, making it hard for others to understand them. Other speech problems include stuttering (i.e., abnormal stoppages, repeated sounds, or prolonged sounds and syllables), and pitch, volume, or voice quality issues. Two common language problems are expressive and receptive difficulties. 4a. Expressive Language Difficulties Examples of expressive language problems include difficulties using language to convey messages to others. Children and adolescents may have trouble recalling words and producing sentences that are considered developmentally appropriate in length and structure. They may have limited vocabulary and may use incorrect tenses (e.g., “I go to school yesterday” versus “I went to school yesterday”). 4b. Receptive Language Difficulties Examples of receptive language problems in children include difficulties understanding language in messages being conveyed to them. Children and 26 adolescents may have difficulties understanding words or sentences of varying types and complexities. Children and adolescents who have speech and/or language problems often have emotional, social and behavioral difficulties. For example, children may withdraw socially or isolate themselves from peers and school or social events where speaking is required. Speech/language difficulties might also cause acting-out or attention-seeking behaviors. Overall, children and adolescents with speech/language problems are more susceptible to social and academic difficulties. 4c. Auditory Processing Disorder (APD) Some children and adolescents have trouble processing information that they hear in the same way as others do because their ears and brain lack proper coordination. Background noise may be particularly disturbing to them when they are trying to pay attention. They may have difficulty remembering things like lists, directions and other items in the immediate future and/or in the near to distant future. Other problems that children or adolescents may manifest include difficulty differentiating sounds or words that rhyme or have similar beginning sounds. These problems can affect many academic areas such as reading, spelling, and writing. Children with APD may have difficulty maintaining focus for long periods of time and may have difficulties with higher-level listening tasks, such as understanding riddles, grasping verbal math problems, or understanding subtlety in conversations. 5. Educational 5a. Learning Disabilities (APA) 5b. Mental Retardation 5a. Learning Disabilities Learning Disabilities (LD) are diagnosed when a child’s achievement on individually administered, standardized tests in reading, mathematics, or 27 written expression is substantially below that expected for age, schooling, and level of intelligence. These learning problems significantly interfere with academic achievement or activities of daily living that require reading, mathematical, or writing skills. The three subtypes are Reading Disorder, Mathematics Disorder, and Disorder of Written Expression. Symptoms of Learning Disabilities may include: A consistent failure to complete homework assignments on time Poor organization or study skills A tendency to procrastinate or postpone doing homework assignments in favor of playing A family history of academic problems Feelings of depression, insecurity, and low self-esteem that interfere with learning and academic progress A tendency to act out and disrupt class when encountering difficulty or frustration in learning Heightened anxiety that interferes with client’s performance during tests or examinations Excessive or unrealistic pressure placed on the client by his/her parents to the degree that it negatively affects his/her academic performance A decline in academic performance that occurs in response to environmental factors or stress (e.g., parents’ divorce, death of a loved one, relocation, or move). Nonverbal Learning Disorder (NLD) is a type of Learning Disability that affects children’s visual, spatial, motor, and language skills. For example, children and adolescents with NLD commonly have difficulties interpreting social cues, paying attention to visual stimuli and shifting focus from one task to another. 5b. Mental Retardation Children with mental retardation may have different levels of impairment in their adaptive functioning (e.g., communication, self care, problem solving, social skills, and vocational skills). The level of adaptive impairment generally falls under four classifications: (1) mild, (2) moderate, (3) severe, and (4) profound. 28 Children with severe cognitive impairment may also exhibit mental health issues that warrant assessment and treatment. For example, children with mental retardation may suffer from anxiety, depression, and problems with social adjustment. It is critically important that children with mental retardation be thoroughly evaluated for mental health issues as well as strengths (personal assets) by trained professionals. 6. Special Education Concepts 6a. The Individuals with Disabilities Education Act (IDEA) is a federal program that provides funds to school districts to help support the education of children with disabilities. IDEA outlines the disabilities that are covered under the program (such as mental retardation and autism), and provides guidelines for educating and providing services to children with disabilities in order to protect and guarantee their right to a free and appropriate education. 6b. An Individualized Education Plan (IEP) is a unique program that is developed by parents, teachers, administrators, and others to address the educational needs of a particular child. A child who is eligible for a special education and additional services may have an IEP that includes information such as his or her current level of functioning, goals, special services, and any other information that is relevant to providing him or her with an appropriate education. IEP’s are typically reviewed once a year and are modified as necessary to help the child reach his or her goals. 6c. A 504 Plan is a legal document that is a part of the Rehabilitation Act of 1973. It serves to assist students with special needs who are in a regular education environment, but who still have a disability that negatively impacts a major life function. 29 Service Provider Definition and Qualifications (APA) 1. Social Worker – A counselor who helps people function well in their environments (e.g., home, school, work, etc) and helps people manage their relationships with others. They can be trained to help in several areas such as children, families, and schools; mental health and substance abuse; and medical and public health. Qualifications: A master’s degree in social work has become standard for many positions and is often required for positions in health settings and for clinical work. A state license is also required. 2. School Psychologist – A psychologist who provides psychological services such as counseling and testing to children in elementary schools, secondary public schools, or state-approved nonpublic school settings. Qualifications: Graduate level training in school psychology (i.e., 60 graduate level credits) or a doctoral degree (Ph.D. or Psy.D.) in school psychology and state certification and/or licensure. 3. Clinical Psychologist – A doctoral level psychologist who is trained to diagnose mental disorders and provide therapy to persons with mental, emotional, and/or social problems. Qualifications: A doctoral degree (Ph.D. or Psy.D.) in clinical psychology and state licensure. 4. Neuropsychologist - A doctoral level psychologist who specializes in the diagnosis and treatment of neuropsychological brain disorders. 30 Qualifications: A doctoral degree (Ph.D. or Psy.D.) in psychology with post-graduate training in neuropsychology. 5. Child and Adolescent Board Certified Psychiatrist – A medical doctor who specializes in diagnosing and treating children with emotional and behavioral disorders. These professionals are qualified to prescribe medication. Qualifications: A medical degree, state licensure, and board eligibility/certification by the American Board of Psychiatry and Neurology. 6. Occupational Therapist – A therapist who assists people with mental, physical, developmental, and/or emotional disabilities by helping them improve in abilities to perform daily living skills and work related tasks. Qualifications: A master’s degree in occupational therapy and state licensure. 7. Physical Therapist – A therapist who provides services to people suffering from injury or illness to help restore functioning, improve mobility, relieve pain, and/or prevent or limit permanent physical disabilities. Qualifications: Graduation from an accredited physical therapist educational program and state licensure. 8. Speech and Language Specialist/Pathologist – A professional who is trained to assist people who cannot or have difficulties with producing speech sounds or using language in general. Qualifications: A master’s degree in speech and language and state licensure. 9. Pediatric Neurologist – A medical doctor who specializes in diagnosing and treating children with neurological disorders. Qualifications: A medical degree (M.D.) and specialized training in pediatric neurology. 31 Medications for Common Problems (APA) Attention Deficit/Hyperactivity Disorder Medications The medications that are approved for use in the treatment of attention (ADHD), the most common behavioral disorder of childhood, have all been extensively studied and specifically labeled for pediatric use. Stimulant medications should be prescribed only after a careful and comprehensive evaluation has established the ADHD diagnosis. Adderall, Ritalin, Concerta, Metadate, Dexedrine, Focalin are examples of stimulant medications prescribed for children with ADHD subtypes (i.e., primarily inattentive, combined, or hyperactive-impulsive). In 2002, the FDA approved Strattera, a non-stimulant medication prescribed for child with ADHD. Antidepressant and Antianxiety Medications These medications follow the stimulant medications in prevalence among children and adolescents. They are used for depression (a disorder recognized only in the last 20 years as a problem for children), anxiety disorders, including obsessive-compulsive disorder (OCD). In your child’s brain, there are many “neurotransmitters” that impact the way he/she thinks, feels, and acts. Three of these neurotransmitters that antidepressants and antianxiety medications influence are serotonin, dopamine, and norepinephrine. The medications most widely prescribed for these disorders are the selective serotonin reuptake inhibitors (the SSRIs). SSRIs affect mainly serotonin and have been found to be effective in treating depression and anxiety without as many side effects as other antidepressants. Examples of SSRIs that are prescribed to children include Luvox (Fluvoxetine), Prozac (Fluoxetine), Citalopram (Celexa), and Zoloft (Sertraline). 32 Anti-anxiety medications such as Klonopin, Xanax, Buspar, and Ativan decrease anxiety by diminishing activity in brain arousal systems. They reduce agitation and over-activity, and help promote sleep. Antipsychotic Mediations These mediations are used to treat children with schizophrenia, bipolar disorder, autism, Tourette syndrome, and severe conduct disorders. Some of the older antipsychotic medications have specific indications and dose guidelines for children. Some of the newer “atypical” antipsychotics, which have fewer side effects, are also being used for children. These medications require close monitoring by your physician for side effects. Examples of antipsychotic medications include Risperdal, Zyprexa, Seroquel, Aripiprazole, and Abilify. Mood Stabilizing Medications These medications are used to treat bipolar disorder (manic-depressive illness). However, because there is very limited data on the safety and efficacy of most mood stabilizers in youth, treatment of children and adolescents is based mainly on experience with adults. The most typically used mood stabilizers are lithium, and the anticonvulsant, valproate (Depakote), which are effective for controlling mania and preventing recurrences of manic and depressive episodes. Effective treatment depends on appropriate diagnosis of bipolar disorder in children and adolescents. There is some evidence that using antidepressant mediation to treat depression in a child who as bipolar disorder may induce manic symptoms if it taken without a mood stabilizer. In addition, using stimulant medications to treat co-occurring ADHD or ADHD-like symptoms in a child with bipolar disorder may worsen manic symptoms. While it can be hard to determine which youngster may become manic, there is a greater likelihood among children and adolescents who have a family history of bipolar disorder. If manic symptoms develop or markedly worsen during antidepressant or stimulant use, a physician should be consulted immediately. 33 Frequently Asked Medication Questions Q1: Does medication affect young children differently from older children or adults? A: Yes. Young children’s bodies handle medications differently than older individuals and this has implications for dosage. The brains of young children are in a state of very rapid development, and animal studies have shown that the developing neurotransmitter systems can be very sensitive to medications. A great deal of research is still needed to determine the effects and benefits of medications in children of all ages. Yet it is important to remember that serious untreated mental disorders also negatively impact brain development. Q2: If my preschool child receives a diagnosis of a mental disorder, does this mean that medications have to be used? A: No. Medications are not generally the first option for a preschool child with a mental disorder. The first goal is to understand the factors that may be contributing to the condition. The child’s own physical and emotional states are key,but many factors such as parental stress or a changing family environment may influence the child’s symptoms. Certain therapies may be as effective as medication. Q3: How should medication be included in an overall treatment plan? A: When medication is used, it should not be the only strategy. There are other services that you may want to consider. These include family support services, educational classes, behavior management techniques, as well as family therapy and other approaches should be considered. Any prescribed medication should be monitored and evaluated regularly. Q4: What medications are used for which kinds of childhood mental disorders? A: There are several major categories of psychotropic medications: stimulants, antidepressants, antianxiety agents, antipsychotics, and mood stabilizers. For medications approved by the Food and Drug Administration (FDA) for use in children, dosages depend on body weight and age. 34 Preventive Care/Schools Helping Reaching Out to Students (NASP) Students who are depressed may not ask for help because they believe no one cares or that nothing can be done. Students may not want to be labeled as having a problem, particularly if they already believe they are to blame for being unpopular, unworthy, or a failure. It is never wrong to ask a student who seems troubled if she or he is OK, but a depressed student may dismiss overtures of concern as misplaced or intrusive. Depending on the severity of the student's symptoms and behavior, staff members can respect this type of response but should continue to observe the student and confer with other staff members. Positive connection between an at-risk student and a trusted adult is important. However, teachers are not trained mental health professionals and should not take on responsibility for treating a student. Staff members should never promise to keep a student's feelings a secret but should assure the student that they will only share their concerns with other appropriate adults (including parents) who can and will help. Contact parents and the school psychologist or other mental health professional immediately. Do not leave the student alone at any time if they are suspected of being suicidal. 35 Schools Can Help Create a caring, supportive school environment that promotes connectedness and prevents alienation. Educate students, staff members, and parents on the realities and signs of depression. Help distinguish between depression and normal adolescent emotions (being upset by a bad grade or a fight with a friend). Destigmatize attitudes and openness about the illness. Build trust between school personnel and students. Ensure that each student has at least one adult in the building who takes a special interest in him or her. Develop and disseminate a protocol for reaching out and responding to students who may be depressed. Train staff members and parents in appropriate ways to observe students and to increase their comfort level and ability to intervene and refer students. Know the signs of suicide and have a suicide prevention and intervention plan in place. Emphasize the responsibility of all students and staff members to report any threat of suicide or violence. Use school mental health professionals (e.g., school psychologists and social workers) to develop prevention and intervention plans, provide intervention, and train others. Be familiar with community mental health resources. Supporting Children’s Mental Health: Parent/Educator Tips Create a sense of belonging. Feeling connected and welcomed is essential to children’s positive adjustment, selfidentification, and sense of trust in others and themselves. Building strong, positive relationships among students, school staff, and parents is important to promoting mental wellness. Promote resilience. Adversity is a natural part of life and being resilient is important to overcoming challenges and good mental health. 36 Connectedness, competency, helping others, and successfully facing difficult situations can foster resilience. Develop competencies. Children need to know that they can overcome challenges and accomplish goals through their actions. Achieving academic success and developing individual talents and interests helps children feel competent and more able to deal with stress positively. Social competency is also important. Having friends and staying connected to friends and loved ones can enhance mental wellness. Ensure a positive, safe school environment. Feeling safe is critical to students’ learning and mental health. Promote positive behaviors such as respect, responsibility, and kindness. Prevent negative behaviors such as bullying and harassment. Provide easily understood rules of conduct and fair discipline practices and ensure an adult presence in common areas, such as hallways, cafeterias, locker rooms, and playgrounds. Teach children to work together to stand up to a bully, encourage them to reach out to lonely or excluded peers, celebrate acts of kindness, and reinforce the availability of adult support. Teach and reinforce positive behaviors and decision making. Provide consistent expectations and support. Teach children social skills, problem solving, and conflict resolution supports good mental health. “Catch” them being successful. Positive feedback validates and reinforces behaviors or accomplishments that are valued by others. Encourage helping others. Children need to know that they can make a difference. Pro-social behaviors build self-esteem, foster connectedness, reinforce personal responsibility, and present opportunities for positive recognition. Helping others and getting involved in reinforces being part of the community. Encourage good physical health. Good physical health supports good mental health. Healthy eating habits, regular exercise and adequate sleep protect kids against the stress of tough situations. Regular exercise also decreases negative emotions such as anxiety, anger, and depression. Educate staff, parents and students on symptoms of and help for mental health problems. Information 37 helps break down the stigma surrounding mental health and enables adults and students recognize when to seek help. School mental health professionals can provide useful information on symptoms of problems like depression or suicide risk. These can include a change in habits, withdrawal, decreased social and academic functioning, erratic or changed behavior, and increased physical complaints. Ensure access to school-based mental health supports. School psychologists, counselors, and social workers can provide a continuum of mental health services for students ranging from universal mental wellness promotion and behavior supports to staff and parent training, identification and assessment, early interventions, individual and group counseling, crisis intervention, and referral for community services. Provide a continuum of mental health services. School mental health services are part of a continuum of mental health care for children and youth. Build relationships with community mental health resources. Be able to provide names and numbers to parents. Establish a crisis response team. Being prepared to respond to a crisis is important to safeguarding students’ physical and mental well-being. School crisis teams should include relevant administrators, security personnel and mental health professionals who collaborate with community resources. In addition to safety, the team provides mental health prevention, intervention, and post-intervention services. Mentally healthy children are more successful in school and life. (NASP) Good mental health is critical to children’s success in school and life. Research demonstrates that students who receive social-emotional and mental health support achieve better academically. School climate, classroom behavior, on-task learning, and students’ sense of connectedness and well-being all improve as well. Mental health is not simply the absence of mental illness but also encompasses social, emotional, and behavioral health and the ability to cope with life’s challenges. 38 Schools are an ideal place to provide mental health services to children and youth. (NASP) Unfortunately, too many children and youth with mental health problems are not getting the help they need and, when left unmet, mental health problems are linked to costly negative outcomes such as academic and behavior problems, dropping out, and delinquency. Schools, however, are ideal settings to provide mental health services. School-based professionals like school psychologists know the students, parents, and other staff. The learning environment provides the right context for prevention and intervention. And, importantly, school is where children spend most of their day. School mental health services focus on the child within the school setting and on collaboration with families. (NASP) School-based mental health services range from prevention and skills development to intervention and evaluation, referral and collaboration, and consultation and counseling. School psychologists are trained to link mental health to learning and behavior in terms of prevention, intervention and outcomes evaluation. They team with parents, other school-based mental health professionals, and community service providers to help create a continuum of services that meet the needs of the individual child. Principal Leadership Magazine, Vol. 4, Number 2, October 2003 Counseling 101 Column When It Hurts to Be a Teenager Depression in students is more than mere teenage angst and requires more than patience and understanding to cure. By Ralph E. Cash, NCSP Ralph E. Cash is a school psychologist in Orlando, FL, and a co-chair of the National Association of School Psychologists' Government and Professional Relations Committee and Health Care Initiative. 39 "There is a tide in the affairs of men which, taken at the flood, leads on to fortune. Omitted, all the voyage of their lives is bound in sorrow and in misery. On such a full sea are we now afloat, and we must take the current when it serves or lose our ventures." -William Shakespeare Depression, particularly in teenagers, is often described as the invisible illness. Its symptoms can easily masquerade as part of the normal tumult of adolescence, a time not noted for level moods or stable behavior. Rapid changes in hormonal balance, physical and cognitive development, response to peer pressure, and perceptions of the world, combined with conflicting desires to be independent but free of responsibilities, make adolescence a time of emotional turmoil and behavioral extremes. Most middle level and high school students experience brief, sometimes intense episodes of the blues, irritability, or rebellion. Even common adolescent behavior-slavish adherence to fads, body piercing, erratic sleep habits, and cyber socializingcan seem pathological to adults. How, then, can parents and educators differentiate between adolescent characteristics that, no matter how outrageous, are "just being a teenager" and those that suggest serious clinical depression? What is the responsibility of schools to do so? The answers to these questions are not just academic. Depression is the most common mental illness among adolescents. Statistically, in a school of 1,000 students, as many as 100 may be experiencing depression or mood swings severe enough to warrant a psychiatric diagnosis. Approximately 13 of those students will attempt suicide in a single year, making suicide the third leading cause of death among teens. Fortunately, most will not succeed, but 15 of the 100 are likely to die by their own hands eventually. Approximately 90% of those who commit suicide have a treatable mental disorder at the time they die. Depression is at the top of this list, but about 70 of those 100 depressed teens will never see a mental health professional. Of the 30 who do, 20 or so will only have that contact in school. If the school has a higher than average proportion of students living in poverty, the picture will be even worse. 40 Schools are an essential first line of defense in combating mental health problems, such as depression, because adolescents spend much of their time in school with skilled and caring professionals who have the opportunity to observe and intervene when a student exhibits signs of a problem. Principals can work with staff members to strengthen protective factors in the school and to educate students, staff members, and parents about depression and the hope offered by effective treatment. Schools can also provide early identification, intervention, and referral services. Failure to do so has serious consequences besides suicide-depression's most tragic and irreversible outcome. Without treatment, depressed teens are at increased risk for school failure, social isolation, unsafe sexual behavior, drug and alcohol abuse, and long-term life problems. Conversely, virtually everyone who receives proper, timely intervention can be helped, but early diagnosis and treatment are necessary. How Can Schools Help? The best intervention is prevention and early intervention. Schools can provide a number of supports to help decrease the occurrence of severe depressive reactions and prompt appropriate early treatment. 1. Destigmatize and shed light on the illness. Perhaps the most important thing schools can do to combat depression is to make the illness easier to identify. Principals can work with their school psychologists and other mental health staff members to educate students, staff members, and parents on the realities, risks, and signs of depression. This should include helping students recognize the difference between their normal feelings of sadness, confusion, or disconnection and depression. Students should be encouraged to talk openly about the illness and other mental health problems with friends and trusted adults. 2. Train staff members, students, and parents in appropriate interventions. Schools that have effective training programs for teachers and other staff members (e.g., bus drivers, school safety officers, coaches, and office workers), parents, and students are much better at intervening early and appropriately on behalf of depressed teens. This should include developing a protocol for reaching out and responding to students who may be depressed and providing appropriate ways to observe and to refer students to mental health services. However, teachers are not trained mental health professionals and should not "counsel" depressed students. Students should be included in the training 41 programs so they can begin not only to recognize signs of depression in themselves but also to help break the code of silence that often prevents teenagers from telling responsible adults when they or their friends are depressed and contemplating suicide or violence. 3. Create a caring, supportive school environment. An impersonal, alienating school culture can contribute to students' risk of depression. Effective interventions must involve collaboration among schools, parents, and communities to counter conditions that produce the frustration, apathy, alienation, and hopelessness experienced by many of our youth. All students and parents should feel welcome in the building. Central to this is to build trust between school personnel and students and to ensure that each student has at least one adult at school who takes a special interest in him or her. Knowing individual students personally is particularly important in recognizing significant changes in behavior, which is one of the key indicators of depression. Bullying prevention is also necessary. 4. Develop a suicide prevention and intervention plan. Depression and suicide prevention programs are intertwined. It is important to educate the school community about the warning signs of suicide and to have a clear intervention plan in place that includes a trained crisis intervention team. All staff members should know what to do if they think a student is suicidal. Students must be partners in suicide prevention efforts because they are most likely to be aware of classmates' plans to hurt themselves or others. In the vast majority of cases, students who attempt suicide or perpetrate violent acts have warned someone beforehand, and that person is usually another student who keeps the information to him- or herself. Emphasize that all students and staff members have a responsibility to report any threat of suicide or violence. Have a well-defined, confidential procedure established for doing so. 5. Be mindful of at-risk students. These students should be monitored, particularly during periods of high stress, either on an individual level or in the school community. Examples of high-stress situations can include exams, the death of a family member, the suicide of another student, or a major event such as September 11, 2001. 6. Use school mental health professionals. School psychologists, social workers, and counselors are excellent resources for designing and implementing training programs for all groups. They can also be invaluable in developing suicide prevention and violence prevention programs as well as in providing direct intervention and ongoing counseling to students. 42 Intervention plans must include mechanisms for connecting students and parents with appropriate and affordable community resources for treatment and monitoring. 7. Provide students with appropriate supports. These should be recommended by your school psychologist or the student's private clinician, but they may include individual or group counseling, continued observation, academic accommodations, opportunities for creative expression, medication, and self-monitoring strategies and steps for seeking help. It may also be appropriate-if given permission-to reach out to the student's social network to generate social support. It should be made very clear, however, that students should not take on responsibility for managing or fixing a friend's depression and should seek adult help if a friend seems to be deteriorating. Encourage cooperation with parents. Educate parents and open up lines of communication. Some parents of depressed teens will want significant help from the school; others who can afford to do so will prefer to keep their child's illness and treatment separate from school. In such cases, the school should make every effort to establish some coordination with the student's private clinician either directly or through the parents. This will make it easier to provide appropriate supports in school and to be aware of the student's progress. However, be sensitive to parents' concerns for privacy and what information may or may not go into their child's school record. Take the Current When It Serves In Shakespeare's words, we are "on such a full sea" of knowledge about depression, from identification to treatment, that there is no excuse for depression to remain invisible or untreated. There are tremendous volumes of research and numerous successful programs designed for schools. Schools that destigmatize depression, educate and engage stakeholders, and provide appropriate interventions can help ensure that students are not "bound in sorrow and in misery" but "lead on to fortune." PL Copyright 2003 National Association of Secondary School Principals. Produced in cooperation with the NASP. 43 RECOGNITION (NASP) All children need recognition. Positive feedback validates behaviors or accomplishments that are valued by others. School staffs recognize academic achievement through grades, sharing a child’s work in class, and awards. They can also use recognition to help children develop mentally healthy behaviors, such as praising a child who exhibits self-control when angry, raises their hand instead of calling out, or shows compassion for a peer. The key is to focus on positive behaviors, even as a way of stopping negative ones. For instance, if a child is misbehaving, try to acknowledge at least three children doing something right before attending to the child who is not. In some cases, it may be necessary to devise situations where a child can do the right thing, such as completing a task (collecting the pencils), and praising them for it. Principals often have students in their office when they are at their lowest point. Try to start the interaction with something positive about the child before addressing the problem behavior. Acknowledge the validity of the feelings that may be underlying their actions. Help the child identify something they do well and if possible link that skill to an appropriate achievable task that they can do in the office or other supervised setting until they are ready to return to class. Be prepared. Establish with your school psychologist or counselor in advance activities that are effective in various situations. MAKING A DIFFERENCE (NASP) Children need to know that they can make a difference. We see this in their eagerness to do classroom chores or read the morning announcements. Such prosocial behaviors build self-esteem, foster connectedness; reinforce personal responsibility, and present opportunities for positive recognition. It is important to create a variety of developmentally appropriate opportunities to contribute, such as putting homework in the take-home folders, helping create a bulletin board, and being a “4th Grade Buddy.” Children can contribute outside of school through activities like the “Gran Club,” a group of students who visit residents at a local nursing home once a week. 44 Activities like this reinforce being part of the community and also give children who do not easily step forward in school the chance to make a difference in the larger context of neighborhood. RESILIENCY (NASP) Resiliency is an essential ingredient to success. It refers to the ability to bounce back from defeat by resetting one’s compass, redefining goals, and continuing on course. Research shows that children with similar risk factors may have different outcomes based on their resiliency. This comes not from blind determination but in a renewed sense of determination. Educators can help children develop resiliency by taking on the role of the “Encourager,” someone who acknowledges the significance of the defeat but does not allow it to result in a sense of personal failure. The key is to help the child see the big picture and refocus on their ability to try again or, if necessary, find alternative means to accomplish their goal. This process allows the child to accept the responsibility for their effort but also be reassured of their own worth. ACCOMPLISHMENT (NASP) Children need to know that they can accomplish goals through their actions. This is often referred to as self-efficacy or self-determination. Children who lack this ability may be overly dependent or tend not to accept responsibility for their actions because they do not believe they are in control. We can build on children’s ability to complete a task (e.g., organizing blocks by color) by helping them learn to set their own goals. Steps in this process include helping the child define the goal (reading better), identifying strategies (reading ten minutes before bed), establishing a method of assessment (able to read book X), and determining the time period in which it will be accomplished. 45 Although it takes considerably longer, this method also works for problem solving and conflict resolution. The goal is to enable a child to recognize a problem, define a desired outcome, identify the resources they have to solve the problem, assess progress towards the goal, and judge when they need help. It is appropriate for children to seek help once they have exhausted their own capacity or recognize that the situation is beyond the scope of their competency. ADAPTING TO CHANGE (NASP) Routine is important to young children. They are introduced to the concept in kindergarten and first grade with habits such as coming in quietly, putting belongings in a cubby, checking in, ordering lunch, etc. Such regular activities lend structure to the child’s environment and help establish their sense of competence and belonging. Equally important, though, is the ability to adapt to change. This is a critical capacity throughout life that begins to develop at a young age. Some children react negatively to change, particularly if they are experiencing emotional stress. They may need help adjusting even to small changes at school (substitute teacher, new seating arrangement) or at home (new sibling, different bed). Principals and teachers should encourage parents to inform them of any unsettling changes at home. Adults can minimize anxiety associated with change by giving students advance warning and allowing them to take part in the change, such as discussing the possibilities for rearranging the classroom. It is also important to help children develop coping strategies. Identifying the things that have not changed and focusing on their competencies (switching tasks independently during center time) can help children maintain a sense of control and stability. 46 Warning Signs/Early Detection (APA) Efforts to identify early warning signs for mental health problems in children are important for curbing the onset of mental health issues and remediating existing mental health problems. Early detection in children is especially critical for making timely and effective intervention decisions. Screening for mental health issues is equally important as a means of forestalling the onset of a disorder and preventing mental health issues from becoming firmly established as children move into adulthood. Frequently Asked Questions (APA) Q: What should I do if I am concerned about mental, behavioral, or emotional symptoms in my child? A: Talk to your child’s doctor first. Ask questions and find out everything you can about the behavior or symptoms that worry you. Every child is different and even normal development varies from child to child. Sensory processing, language, and motor skills are developing during early childhood, as well as the ability to relate to parents and to socialize with caregivers and other children. If your child is in daycare or preschool, ask the caretaker or teacher if your child has been showing any worrisome changes in behavior, and discuss this with your child’s doctor. Q: How do I know if my child’s problems are serious? A: Many everyday stresses cause changes in behavior. The birth of a sibling may cause a child to temporarily act much younger. It is important to recognize such behavior changes, but also to differentiate them from signs of more serious problems. Problems deserve attention when they are severe, persistent, and impact on daily activities. Seek help for your child if you observe problems such as changes in appetite or sleep, social withdrawal, or fearfulness; behavior that seems to slip back to an earlier phase such as bed-wetting; signs of distress such as sadness or tearfulness; self-destructive behavior such as head banging; or a tendency to have frequent injuries. In addition, it is essential to review the development of your child, any important medical problem he/she might have had, family history of mental disorders, as well as physical and psychological traumas or situations that may cause stress. 47 Q: Whom should I consult to help my child? A: First, consult your child’s doctor. Ask for a complete health examination of your child. Describe the behaviors that worry you. Ask whether your child needs further evaluation by a specialist in child behavioral problems (see Basic Definitions Section - Professionals). Q: How are mental disorders diagnosed in children? A: Similar to adults, disorders are diagnosed by observing signs and symptoms. A skilled professional will consider these signs and symptoms in the context of the child’s developmental level, social and physical environment, and reports from parents and other caretakers or teachers, and an assessment will be made according to criteria established by experts (See Basic Definitions Section - Professionals). Very young children often cannot express their thoughts and feelings, which makes diagnosis a challenging task. The signs of a mental disorder in a young child may be quite different from those of an older child or an adult. Q: Won’t my child get better with time? A: Sometimes yes, but in other cases children need professional help. Problems that are severe, persistent, and impact on daily activities should be brought to the attention of the child’s doctor. Great care should be taken to help a child who is suffering, because mental, behavioral, or emotional disorders can affect the way the child grows up. Crisis Intervention There are times when families face difficult situations that require immediate professional assistance. Examples of crisis situations may include, but are not limited to, someone threatening and/or hurting oneself (suicidal thoughts), major property destruction (e.g., setting fires, breaking windows), and/or hurting others (child abuse, domestic violence). There are many places, local and national hotlines, and people to turn to for help. Below you will find contact numbers to call during crisis situations. 48 NATIONAL CONTACT NUMBERS CHILD ABUSE ChildHelp USA National Child Abuse Hotline 800-4-A-CHILD or 800-412-4453; 222.4453 (TDD) Multilingual crisis intervention and professional counseling on child abuse Call 24 hours a day, 7 days a week National Child Abuse Hotline 800-25-ABUSE or 800-252-2873 CRISIS INTERVENTION/SUICIDE Girls and Boys Town Suicide and Crisis Line 800-448-3000 or 800-448-1833 (TDD) Can provide aid for parent-child conflicts, marital and family issues, suicide 49 What School Psychologists Offer to the Sevier County School System (Sevier County Website) An Overview School psychologists are an integral and important part of the special education team in Sevier County, as well as of the district’s organizational structure. School psychologists provide a wide variety of both educational and clinical services to districts, school staff, students, and their families. School psychologists: • have an understanding and knowledge of educational policies and issues that stem from working within the educational system • have an understanding of schools as a result of maintaining regular and direct contact with students, teachers, parents, and the community • have long-term contact with chronic situations (i.e. disruptive behavior disorders, learning disabilities) within the school system and are regularly exposed to how these situations affect the classroom on a day-to-day basis • bring a psychological approach to the analysis of students’ behavior problems; that is, a scientific, research-based and measurable approach to the study of human behavior and learning • have the tools to systematically measure change in behavior over time • have the training to carry out psychological assessment of students’ cognitive and learning styles for the purpose of educational planning • have the training to recognize, diagnose, and intervene with various childhood behavior and learning disorders • consult with others involved with students to make achievable and appropriate recommendations and plans for students • support the parents and teachers in the implementation of recommendations and plans • maintain liaisons with other agencies in the community to ensure comprehensive service-delivery to students, parents, and teachers with whom they work • develop, consult, and participate in programs designed to intervene in crisis and emergency situations in schools • act as a psychological resource to the educational system 50 The Client Population of School Psychologists School psychologists provide services and interventions to all students in the school system by following a primary prevention, intervention, and postintervention service-delivery model. School psychologists enhance the ability of all students to have opportunities for success in school, develop the skills to perform well in school, and receive recognition for their efforts. These are the three components which Furlong, et al (2000), cite as the bedrocks of connectedness to school. School psychologists intervene with the whole school population through primary prevention measures such as anti-violence awareness programs, wellness promotion, personal safety and safe-school programs (counseling SDC students and staff), and family support initiatives. There are some students in a school who will require more direct intervention. This might take the form of assessment for learning, behavioral, developmental and emotional problems and subsequent program development to address the specific needs identified by the school and through the assessment results. In addition, there may be need for referral to and liaison with community professionals and agencies who might be appropriate to meet the students’ medical and counseling needs. There may also be need for parental support. Some students have need of specialized and immediate assistance. Students at risk of leaving or removal from school (i.e. those with severe disruptive behavior disorders) have clearly passed the place where the usual interventions can be expected to be helpful. They require what might be termed post-intervention or services for acute and chronic problems. They need more intensive supports in the form of alternative education programs, on-going counseling services, dropout recovery and follow-up support, and possible family preservation interventions. While these would not likely be delivered directly by the school psychologist, they would be done in direct consultation with the school psychologist. School psychologists serve the total school population by drawing on the full content of their training and directing their skills differentially. This breadth of preparation and service-delivery is the key contribution of school psychologists to their clients. Roles and Responsibilities of School Psychologists Because they work directly in the educational setting, school psychologists are familiar with the unique characteristics, delivery systems, and current 51 educational policies of the school system. School psychologists work with school, district, and community-based teams, and bring a unique perspective on child development, combined with a research-based system for problem solving. School psychologists complement the different training and approaches of other team members in providing the most effective and comprehensive service to children and adolescents in our schools. School psychologists support students and teachers in a variety of ways that have an impact on a student’s learning and behavior in the classroom. Five Levels of Intervention for School Psychologists A. Student-Focused Indirect Intervention Focus – To work with parents and teachers in planning educational and behavioral interventions for individual students. Consultation – School psychologists consult with teachers and administrators in discussing concerns related to individual student or class behavior and learning difficulties. Program planning – School psychologists participate in program planning and case reviews for individual students. Psychologists provide advice on adapting the curriculum and making accommodations to meet a student’s learning style, cognitive profile, and developmental/behavioral needs. Parent contact – School psychologists consult with parents of students with behavior, socio-emotional, and learning difficulties regarding concerns and intervention strategies, and provide information to improve understanding. Goal setting – School psychologists interpret their assessment findings and use them to help to establish realistic goals based on a student’s strengths and needs. Teacher assistance – School psychologists consult with teachers and suggest teaching strategies based on the specific nature of the student’s learning or behavioral difficulty. Interagency networking – School psychologists collaborate and coordinate with other agencies to provide comprehensive services to the child. Referrals – School psychologists facilitate referrals to other agencies and professionals, as needed. 52 B. Student-Focused Direct Intervention Focus – To work directly with the student either via a psychological assessment and/or in a therapeutic or counseling relationship. Individual counseling and therapy – School psychologists use techniques such as cognitive behavioral therapy, relaxation therapy, rational emotive therapy, and social skills training that have a research-based efficacy. Individual counseling and therapy also involve psychoeducational techniques designed to help the student and others have a better understanding of the problem. These may also include counseling focused on personal issues, prevention, and planning for the future. Group behavior skills development – School psychologists often meet the needs of a number of students by organizing small groups which focus on social skills training, anger management training, stress management, and the effects of divorce on children, for example. These may or may not be conducted in SDC programs depending upon the structure of the school or the presence of an SDC. Individual psychological assessment – Individual psychological assessment includes the administration and interpretation of standardized psychological tests (i.e, .cognitive development, memory, language, executive functioning, visual perception, auditory perception, language development, visual motor skills, academic attainment, social-emotional and behavior adjustment). Assessment also includes classroom observations, file review, gathering case history information through interviews and checklists, and reviewing other professional assessments of the child. The data from a psychological assessment serve as the basis for recommendations concerning intervention strategies for parents and teachers. C. School-Wide Intervention Focus – To work with a school toward improving the delivery of services in meeting students’ mental health and learning needs. Liaison – The school psychologist acts as a liaison with, and/or serves on school-based IEP teams. 53 Collaboration – The school psychologist collaborates with teachers and administrators to support inclusion of exceptional students within the school. In-service education – The school psychologist provides school-based inservice training to teachers and administrators in such areas as behavior management strategies, collateral assessment methods, understanding exceptionalities, and stress management. Prevention – The school psychologist advises on school-wide prevention and intervention programs that facilitate the development of a positive school environment. Consultation – The school psychologist consults with teachers and administrators in the provision of information about learning styles and behaviors commonly associated with various identified learning, socialemotional, and behavioral problems. Best practices – The school psychologist provides information related to current research on interventions in the area of children’s mental health and various exceptionalities. Planning – The school psychologist participates in planning and implementing school-wide screening and assessment programs. Post-Intervention – The school psychologist coordinates debriefing and defusing of students and staff following a tragic event, which affects the school as a whole. Teaching – The school psychologist facilitates parenting programs. D. System-Wide Intervention Focus – To improve the system as a whole in its effectiveness in dealing with students’ mental health and learning difficulties. In-service education – The school psychologist provides district-wide inservice training for educational staff on child development, behavior management, exceptionalities, and assessment. Screening – The school psychologist develops and carries out early screening programs in the schools. Evaluation – The school psychologist assists with data collection and evaluation of system-wide special education interventions. Best practices – The school psychologist reviews current educational and psychological research on topics of relevance to educators. 54 Intervention programs – The school psychologist assists in developing, implementing, or consulting with system-wide intervention programs (i.e. conflict resolution, social skills, bullying programs, drop-out prevention, violence prevention, crisis intervention, alternative education programs). Outreach – The school psychologist develops and implements parenting programs. Networking – The school psychologist serves on multi-agency committees and programs, and collaborates with various agencies in program planning. Advocacy – The school psychologist advocates for children with learning, social-emotional and behavioral exceptionalities. E. Research The training of a psychologist stresses the use of a scientific researchbased approach to the study of human behavior. As a result, psychologists are in a position to serve in both an advisory capacity or to have direct responsibility for carrying out research projects in the educational setting. More specifically, psychologists can advise on or carry out planning, data collection, data analysis, interpretation of results, and translation of findings into practical applications. Psychologists have training in statistical analysis and techniques, and social sciences research design. They are, therefore, in a unique position within the educational setting to design and implement research projects for a variety of purposes. In particular, psychologists can evaluate the effectiveness of various types of behavioral and educational interventions, as well as the effectiveness and validity of various group and individual assessment tools. There are numerous educational psychology journals devoted to the publication of this research, and psychologists have an ethical responsibility to keep their knowledge of the discipline up to date. 55 Psychological Assessment in Sevier County Schools The Sevier County School System’s inclusionary practices frame the focus of a psychological assessment in meeting the needs of the individual student. A psychological assessment is an objective measure of samples of behavior. It may include the evaluation of: • • • • • • • • • • • social adjustment emotional status personality cognitive functioning language processing information processing visual-motor development executive functioning (attention, impulse control) aptitude academic achievement motivation Information obtained in an assessment is used to plan specific instructional and behavioral interventions for the student, as well as to set realistic, attainable goals. The psychological assessment, along with information from numerous sources and other professionals, contributes to a further understanding of the whole child. A psychological assessment involves the use of formal, psychodiagnostic procedures requiring a considerable degree of training, expertise, and continual upgrading of knowledge. Psychological tests and procedures utilized in an assessment are scientific and researchbased tools. In the hands of inexperienced, unsupervised, or unqualified individuals, there is potential for serious consequences such as misdiagnosis and improper interpretation of assessment data. This could lead to either ineffective interventions or possibly harmful interventions. As part of both their university training and their licensing residency, psychologists practicing in Sevier County Schools undergo considerable supervised experience in the application of a variety of psychological techniques, including assessment. 56 There are a number of excellent academic tests that can be comfortably and competently administered by resource teachers and guidance counselors. Results of these tests offer teachers valuable direction for immediate interventions with students, as well as providing substantial collateral information for a psychological assessment. School psychologists, with their specialized training in psychometrics, can be helpful on a consultative basis, assisting resource teachers and guidance counselors in interpreting scores on various standardized academic tests. The provision of in-service training in the areas of statistics, test construction, validity, reliability, and the meaning of various scores (e.g. standardized scores, percentile ranks, grade equivalency) is another service that can be provided by school psychologists. When Should A Psychological Assessment Be Requested? A service-delivery model that requires an initial consultation with the school psychologist prior to an assessment referral is recommended. This process allows for a more timely response, as several consultations can occur in the time it takes to do one assessment. This process also allows the psychologist to have input into establishing the need for, and the goals of, the assessment, as well as assisting the school in determining assessment priorities. In other cases, a review of the student’s file, assistance with interpretation of school-based educational assessments, and consultation may be adequate to address the concerns. In all cases, a consultation allows for some immediate intervention to take place, even if the student has to be placed on a waiting list for an assessment. School psychology is an educationally based support service. Requests for school psychological services, including assessments, should go through school Support-teams (S-Teams). The S-team is in the best position to establish school referral priorities and the team should screen all requests for formal assessment. School psychologists do not accept direct referrals for assessment from professionals outside of the school system, although preliminary consultation is welcome. 57 Situations that might warrant a referral to a school psychologist include the following: 1. The classroom and resource teachers have worked with the student and have carried out some individual educational assessments. The student is not responding to the strategies outlined in the IEP and teachers do not know why. School personnel believe that they require more information regarding the student’s learning style, and cognitive and developmental profile in order to enhance the student’s special education program. 2. Teachers are uncertain about the student’s developmental level and need assistance in developing realistic long-term expectations for the student. 3. Teachers suspect that the student may have a neurologically based disorder (e.g. Autism, Attention Deficit Hyperactivity Disorder, Tourette’s Syndrome, Mood Disorder) that is having a significant impact on the student’s adjustment. Diagnostic confirmation, advice on needed referrals to other professionals, and intervention strategies are required. 4. There is a conflict between the teachers’ and the parents’ expectations and perceptions of a student’s learning and/or behavioral needs. In some of these cases, a psychological evaluation is believed to be required to provide objective and standardized information to further clarify the student’s needs and to assist in resolving the conflict. 5. Teachers believe that the parents are having difficulty understanding or accepting their child’s needs. Involving a school psychologist in such discussions can assist the parents to develop a better understanding of their child’s strengths and needs and the value that special programming can provide. 6. A student has serious behavioral and/or emotional problems, and the teachers want to know what (neurological, social-emotional, environmental, and personality) factors might be affecting the student’s behavior. An assessment in this case may lead to referral to other specialties, suggestions of specific types of intervention strategies, or identification of the most appropriate therapeutic (Parkway, SDC) or counseling interventions. 58 Access to School Psychological Services In Sevier County, psychologists working primarily in the schools are employed by the Sevier County Board of Education under the Department of Special Education’s supervision and administration. System personnel (school administrators and counselors) help determine the services they require from the psychologists serving their schools. The types of services provided by a school psychologist will depend on a number of factors, including the training, experience, and the interests of the psychologist, as well as the priorities established by the Department of Special Education and schools served by the psychologist. Student-Focused Consultation Access to school psychological services for consultation, assessment, or other service normally follows a referral process. Teachers are usually the first observers of learning, social-emotional, or behavioral difficulties in the school setting. When a teacher has a concern about a student, a referral form is completed which outlines areas of concern and interventions attempted to address the need. School-based S-team meetings, which usually involve an administrator, resource teacher, guidance counselor, classroom teacher(s), and perhaps a system representative, afford an opportunity to address these concerns. As a result of this collaborative process, a formal referral for school psychological services may be initiated. Psychologists may be available for informal consultation and classroom observation throughout this process. Referrals for service from school psychologists are usually forwarded to the Department’s office. Informed written parental consent must be obtained for students under 16 prior to any direct service ( i.e. formal assessment, counseling, and therapy). The exception would be intervention with a student presenting an immediate risk of harming himself / herself. 59 Ethical Obligations of School Psychologists Professionalism and Psychological Assessments A psychological assessment involves much more than mere administration and scoring of tests. Observations of important aspects of test behavior such as anxiety, fatigue, attentional and motivational factors are very important. The psychologist must be sensitive to the effects of the assessment procedures on the student. Special techniques are often required to elicit optimal performance from some children. The interpretation of the student’s performance has to take into consideration a variety of factors that influence performance and integrate these factors into a larger context of knowledge concerning test construction, theoretical knowledge of child development, learning theory, psychological processes and child exceptionality. An experienced and well-trained psychologist can do this best. A thorough understanding of statistics and psychometrics (test construction) is required to interpret psychological tests accurately. In order to interpret various types of scores, it is necessary to have an understanding of how they are derived, what they mean and how they compare to other types of statistical measures. In addition, the examiner must be capable of reviewing the technical merits of selected instruments in terms of such characteristics as validity, reliability, standardization and test construction. As new instruments come on the market, this particular capability becomes even more essential. It is incumbent on psychologists to be able to demonstrate that the tests and procedures used to arrive at diagnosis and interpretation are valid. Appropriate interpretation of psychological assessments requires familiarity with new developments and with current independent studies of assessment instruments. Accurately making psychological diagnosis is a very challenging task, even for an experienced clinician. The diagnosis of many disorders may result in some very specific prescriptions for therapy, prognosis for outcome and treatment. Non-psychologists, including teachers, should be very careful about making suggestions that a child may have some specific type of psychological disorder. The Diagnostic and Statistical Manual of Mental Disorders (DSM IV) recognizes over 40 psychiatric disorders usually first diagnosed in childhood. In addition, there are also a number of psychological disorders that may be diagnosed in both adults and children. 60 Those engaged in psychological assessments must take into consideration ethical standards, confidentiality and protection of the student’s rights. Informed consent from a student of legal age or from a parent or legal guardian of a younger student is absolutely essential. Information obtained from assessments should only be shared with those persons involved with the teaching and learning process of the student. Reports or test protocols should not be transferred to other agencies or professionals without informed consent. Psychological reports are the property of the school system, and should be kept in secure areas. Once a student is no longer in school, there are clear policies regarding the length of time a psychological report and/or file is kept. (Refer to specific guidelines within Sevier County and Tennessee.) Individuals, including psychologists, administering psychological assessments may find themselves required to defend or explain their assessment in a court of law. School personnel will find that they are on much safer ground if the individuals that they employ to carry out or to supervise psychological assessments are qualified to do so. No court will challenge the right of a licensed psychologist to carry out the accepted tasks of his/her profession. However, individuals performing tasks of a psychological nature who are not licensed or qualified to do so, may find themselves in a very vulnerable position. Controlling Access to Psychological Tests and Procedures A specific responsibility of school psychologists involves the ethical requirement to protect test security and to ensure that access to psychological tests is restricted to licensed psychologists or residents in psychology. All distributors of psychological tests have restrictions on the purchase of different types of instruments. Sevier County takes reasonable steps to ensure that the purchase and distribution of psychological tests are for the use of psychologists or residents in psychology only. Conclusion This document reflects best practices in school psychology. Those practices stem from a primary prevention model of service delivery and a philosophy that the school psychologist works with the total population of the school and the system. Best practices in school psychology are consistent with, and supportive of, the educational practices of the Sevier County School System. School psychologists are mindful of the special and integral role they play in 61 collaborating with, and supporting, the work of teachers and parents in the education of all students and in contributing to resource development and wellness initiatives within the system. I. PROFESSIONAL COMPETENCY The practice of school psychology requires skills in both education and psychology. SCHOOL PSYCHOLOGISTS - Strive to maintain high standards of competence, recognizing the strengths and limitations of their training and experience, and providing service only in areas of competence. - Enlist the assistance of other specialists in supervisory, consultative or referral roles as appropriate. -Take responsibility for their own continuing professional development and pursue opportunities to learn new procedures, become familiar with new research and technology, and implement changes that benefit students. II. PROFESSIONAL RELATIONSHIPS AND RESPONSIBILITIES - Respect those with whom they work, dealing justly with each regardless of physical, mental, emotional, political, social, cultural, racial, or religious characteristics. - Do not exploit their professional relationships. They do not engage in nor condone psychological or physical abuse. STUDENTS - Consider that their primary responsibility is to students. They act as advocates of student’s welfare, taking into account the maturity of the student, the rights of the student and parents, and the responsibility of school personnel. - Recognize the student’s right to participate in services voluntarily. - Inform the student of the outcomes of assessments, counseling or other services in terms appropriate to the age and understanding of the student. PARENTS - Communicate with parents in a manner that ensures their understanding and participation. - Ensure that there is informed consent of parent or guardian for their involvement on an individual basis with any student below the age of consent. 62 - Discuss their findings and recommendations with parents of students below the age of consent. - Inform parents about confidentiality and rights of access to information. PROFESSIONALS - Cooperate with other professionals, in recognition of the student’s need for multidisciplinary services. -Explain their competencies, roles and working relationships to other professionals within and outside the system. - Attempt to resolve on an informal level concerns about a possible ethical violation by another professional. If informal efforts are unsuccessful, they follow the steps for filing an ethical complaint outlined by the appropriate professional association. - Work cooperatively with any other psychologist involved with a referred student, to ensure that the best interests of the student are served. III. PROFESSIONAL PRACTICES IN SCHOOL SETTINGS - Maintain an understanding of the goals, processes and legal requirements of the educational system, as it relates to their practice. - Become familiar with school organization, instructional materials and teaching strategies in order to contribute to the common goal of each student. - Relate to others as staff members of the schools in which they work. ASSESSMENT - Combine observations, background information, multidisciplinary consultation and other pertinent data to present the most comprehensive and valid picture possible of the student. - Choose assessment instruments, which are valid and reliable and are appropriate for the student, recognizing the differences in age and in socioeconomic and ethnic background. - Do not condone the use of psychological assessment techniques by unqualified persons. INTERVENTIONS - Recommend interventions that are appropriate to the needs of the student and consistent with the data collected during assessment. - Refer students to another professional when needs are identified which are outside their competency or scope. - Monitor the effectiveness of recommended interventions. 63 REPORTING - Ensure that student information reaches authorized persons and is adequately interpreted for their use. - Communicate relevant findings and recommendations in language understood by staff, emphasizing interpretations and recommendations rather than test scores. Reports reflect the degree of reliance and confidence which can be placed on the information. - Ensure the accuracy of their reports, letters and other written documents through reviewing and signing them. - Comply with laws, regulations and policies pertaining to storage and disposal of their records. USE OF MATERIALS AND COMPUTERS - Maintain security of psychological tests. - Observe copyright laws regarding reproduction of tests and obtain permission from authors to use non-copyrighted published instruments. - Maintain full responsibility for any technological services they use for diagnostic, consultative or information-management purposes. - Do not promote or encourage inappropriate use of computer generated test analysis or reports. IV. PROFESSIONAL PRACTICE IN PRIVATE SETTINGS - School psychologists do not place themselves in a conflict of interest. Those who provide services both privately and through the Sevier County School System do not accept remuneration for professional work and with clients who are entitled to such service from the school psychologist free of charge. In cases where the school system has mandated additional standards, school psychologists adhere to those standards. - School psychologists in private practice maintain such practice outside their hours of employment. - School psychologists engaged in private practice do not use tests, materials or services belonging to the school system without authorization. 64 References & Resources 1. SECTION ONE-(CTRL + click to follow links) These may also be found at the site of the National Association of School Psychologists. www.nasponline.org National Association of School Psychologists, 4340 East West Highway, Suite 402, Bethesda, MD 20814 Phone: (301) 657-0270 | Toll Free: (866) 331-NASP | Fax: (301) 657-0275 | TTY: (301) 657-4155 Principal Leadership magazine articles, written by NASP members on issues relevant to adolescent mental health and academic achievement. Information About School Psychology What Is a School Psychologist? School Psychologists: Providing Mental Health Services to Improve the Lives and Learning of Children and Youth School Psychology: A Career That Makes a Difference Success in School/Skills for Life Toolkit Register to download a collection of NASP resources for your school's website. Assessment and Instruction NASP Position Statement on Assessment Problem-Solving Model for Improving Student Achievement Psychological Evaluations 65 Behavior Bullies and Victims Bullying Prevention and Intervention Defusing Violent Behavior in Young Children: An Ounce of Prevention Sexual Abuse of Children and Adolescents Sexual Harassment (NASP handout) Zero Tolerance and Alternative Strategies: A Fact Sheet for Educators and Policymakers Crisis and Safety Preventing Youth Suicide: Tips for Parents and Educators Coping With Crisis - Helping Children With Special Needs Dealing With Death at School Helping Children Cope With Loss, Death, and Grief: Tips for Parents and Teachers How to Handle the Media During a Crisis Identifying Seriously Traumatized Children: Tips for Parents and Educators Memorials/Activities: A List of Do's and Don'ts Memorials/Activities/Rituals Following Traumatic Events: Suggestions for Schools Responding to a Death: Tips for Administrators Suggested School Safety "Teachable Moment" Lesson Threat Assessment: Predicting and Preventing School Violence Understanding Cultural Issues in Death: Information for Schools and Crisis Response Teams Diversity Culturally Competent Schools English Language Learners: An Introductory Guide for Educators Making Schools Safe for Sexual Minority Youth Safe and Affirmative Schools for Sexual Minority Youth Health and Wellness Collaborating With Physicians: A Guide for School Leaders Mood Disorders: What Parents and Teachers Should Know Obesity Prevention in Children: Strategies for Parents and School Personnel Otitis Media (Ear Infections): Information for Parents and Teachers Sleep and Sleep Disorders in Children and Adolescents: Information for Parents and Educators 66 Home and School Motivating Learning in Young Children Instruction and Curriculum Grade Retention and Promotion: Information and Strategies for Educators Mental Health Children's Mental Health Depression in Children and Adolescents Depression: When It Hurts to Be a Teenager School-Based Mental Health Services and School Psychologists Supporting Children's Mental Health: Tips for Parents and Educators Understanding and Responding to Students Who Self-Mutilate Social/Emotional Development ABC's of Children's Mental Health Depression in Children and Adolescents: Information for Families and Educators Special Populations An ADHD Primer Asperger Syndrome: A Guide for Secondary School Principals Autism Spectrum Disorders Helping Homeless Students Helping the Student With ADHD in the Classroom Transitioning High School Students With Learning Disabilities Into Postsecondary Education: Assessment and Accommodations Suicide After a Suicide: Answering Questions From Students Save a Friend: Tips for Teens to Prevent Suicide Useful Links National Association of School Psychology State School Psychology Association Links American Association of Suicidology http://www.suicidology.org (202) 237-2280 67 Depression and Bipolar Support Alliance (DBSA) http://www.dbsalliance.org (800) 826-3632 Dougy Center for Grieving Children and Teens http://www.dougy.org (503) 775-5683 Gay, Lesbian, and Straight Education Network (GLSEN) http://www.glsen.org Gay-Straight Alliance Network http://www.gsanetwork.org Healthy Lesbian, Gay, & Bisexual Students Project http://www.apa.org/ed/hlgb National Center for Post-Traumatic Stress Disorder http://www.ncptsd.org National Organization for Victim Assistance (NOVA) http://www.try-nova.org (800) TRY-NOVA SAFE Alternatives http://www.selfinjury.com SOS High School Suicide Prevention Program http://www.mentalhealthscreening.org Links for Resilience http://www.surgeongeneral.gov/library/youthviolence/chapter4/sec4.html http://smhp.psych.ucla.edu/qf/resilience.html http://resilnet.uiuc.edu/library/grotb95b.html http://resilnet.uiuc.edu/library/benard95.html http://www.nccp.org/pub_cwr00h.html http://www.apahelpcenter.org/featuredtopics/feature.php?id=60&ch=2 http://www.familytlc.net/resilient_children_preteen.html http://ohioline.osu.edu/b875/index.html http://cecp.air.org/familybriefs/default.asp Links for Child Development & Wellness http://www.kidshealth.org http://www.nlm.nih.gov/medlineplus/childrenshealth.html 68 http://www.aap.org http://www.americanheart.org/presenter.jhtml?identifier=3033987 http://www.chsd.org/1744.cfm http://www.nhlbi.nih.gov/health/public/sleep/starslp/parents/tips.htm http://www.chop.edu/consumer/news/index.jsp?type=6 http://www.cfw.tufts.edu/ http://www.cdc.gov/ncbddd/ http://www.lpch.org/DiseaseHealthInfo/HealthLibrary/growth/index.html http://www.lpch.org/DiseaseHealthInfo/HealthLibrary/growth/hpc.html http://www.jhbmc.jhu.edu/cardiology/partnership/kids/kids.topics.html http://www.brightfutures.org/ http://www.healthiergeneration.org/kids http://www.cdc.gov/ncbddd/autism/actearly/default.htm 69 2. SECTION TWO- (CTRL + click to follow links) Other Useful Resources: The following sites provide an extensive array of links for all major disorders and topics to assist your research and exploration. American Psychological Association (APA), 750 First Street, N.E., Washington, DC 20002; (202) 336-5500; w w w.apa.org American Psychiatric Association, 1400 K Street, N.W., Washington, DC 20005; (202) 682-6000; w w w.psych.org Child and Adolescent Mental Health Consumer Website: American Psychological Association (APA) http://ucoll.fdu.edu/apa/index.html Educational Psychology Topics http://www.mhhe.com/socscience/education/edpsych/edpsytop.html National Institute of Mental Health (NIMH), National Mental Health Association, 1021 Prince Street, Alexandria, VA 22314; (800) 969-NMHA; w w w.nmha.org http://www.nimh.nih.gov/health/topics/child-and-adolescent-mental-health/index.shtml Open Directory: Mental Health http://www.dmoz.org/Health/Mental_Health/Disorders/Child_and_Adolescent/ United Department of Health and Human Services: Substance Abuse and Mental Health Services Administration http://mentalhealth.samhsa.gov/publications/allpubs/CA-0004/default.asp 70