* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Diastolic Heart Failure and Critical Illness
Survey
Document related concepts
Remote ischemic conditioning wikipedia , lookup
Rheumatic fever wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Heart failure wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Transcript
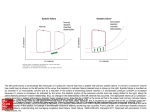
Diastolic Heart Failure and Critical Illness R. Pirracchio and A. Mebazaa z Introduction Diastolic heart failure is a common entity the frequency of which is widely underestimated. Some data available in the literature suggest that nearly half the patients with congestive heart failure (CHF) have preserved left ventricular (LV) ejection fraction (LVEF > 50%) [1±4]. If CHF is clearly defined as a pathophysiological state in which the heart is unable to pump blood at a rate commensurate with metabolic demand or to do so only from an elevated filling pressure, several guidelines have proposed that the diagnosis of CHF should require objective evidence of LV dysfunction, like an echographic measurement of LVEF [5]. As echographic signs of diastolic heart failure are of poor sensibility and specificity, the use of such criteria in the diagnosis of CHF leads to an underestimation of the frequency of diastolic heart failure. Nevertheless, more than a pathophysiological distinction, differences between systolic and diastolic heart failure are of clinical importance since diastolic heart failure is supposed to be associated with a better long-term survival than CHF [6, 7]. Very limited data are actually available concerning the clinical relevance of diastolic heart failure in the critical care setting. We will try to clarify those situations of critical illness where identifying and treating diastolic heart failure could be of clinical importance. z Definitions and Diagnosis Similar to systolic heart failure, diastolic heart failure is described as a chronic disease during which some acute decompensations can occur. These acute events can either be de novo or appear during the evolution of the CHF. Chronic Diastolic Heart Failure Since the early 90s, various guidelines have been published in order to clarify the definition and the diagnosis of diastolic heart failure [7±10]. According to the American College of Cardiology and the American Heart Association, ªthe diagnosis of diastolic heart failure is generally based on the finding of typical symptoms and signs of heart failure in patients with preserved left ventricular ejection fraction and no valvular abnormalities on echocardiographyº [9]. For the Study Group on diastolic heart failure of the European Society of Cardiology, a diagnosis of dia- 198 R. Pirracchio and A. Mebazaa stolic heart failure should be made only in case of ªevidence of abnormal left ventricular relaxation, diastolic distensibility or diastole stiffnessº [7]. Vasan and Levy tried to rationalize the diagnosis with pragmatic criteria which are not yet widely used in the cardiologic literature [8]. They separated three sequential steps for the diagnosis: (1) diagnosis of CHF, (2) preserved systolic LV function (LVEF > 50%), (3) documentation of LV diastolic dysfunction if feasible. Accordingly, the authors proposed to classify subjects suspected of suffering from diastolic heart failure into three groups: 1) `definite diastolic heart failure', for patients with clinical evidence of CHF, objective evidence of preserved LVEF within 72 hours of the CHF event, and documentation of LV diastolic dysfunction 2) `probable diastolic heart failure', for patients having clinical evidence of CHF, preserved LVEF without documentation of LV diastolic dysfunction (after exclusion of valvular diseases or core pulmonale) 3) `possible diastolic heart failure', for patients with clinical evidence of CHF, objective evidence of preserved systolic LV function but not at the time of the CHF event, and no evidence of diastolic LV dysfunction. A clinical setting typical of diastolic heart failure (Table 1) can upgrade a patient from a `possible' to a `probable' diastolic heart failure. Whether the diagnosis of diastolic heart failure requires some objective evidence of diastolic failure still remains controversial. Zile et al. recently provided a prospective comparison of cardiac catheterization and echocardiography in patients suspected of having diastolic heart failure (CHF symptoms and LVEF > 50%) [11]. The authors concluded that ªobjective measurement of LV diastolic function serves to confirm rather than establish the diagnosis of diastolic heart failure. The diagnosis of diastolic heart failure can be made without measurement of parameters that reflect LV diastolic functionº [12]. Finally, from a clinical point of view, diastolic heart failure can be responsible for symptoms that occur at rest, with less than ordinary physical activity, or with ordinary physical activity. Thus, New York Heart Association classification (NYHA) can be used in diastolic heart failure as well as in systolic heart failure. Of note, the global incidence of diastolic heart failure may be underestimated if paraclinical investigations are only made at rest (see below). Table 1. Reasons to upgrade diagnosis from possible diastolic heart failure to probable diastolic heart failure [8] z Markedly elevated blood pressure (systolic BP > 160 mmHg or a diastolic BP > 100 mmHg) during the episode of heart failure z Echocardiographic concentric LV hypertrophy without wall-motion abnormalities z A tachyarrhythmia with a shortened diastolic filling period z Precipitation of event by the infusion of a small amount of intravenous fluid z Clinical improvement in response to therapy directed at the cause of diastolic dysfunction (such as lowering blood pressure, reducing heart rate, or restoring the atrial booster mechanism) Diastolic Heart Failure and Critical Illness Acute Decompensation of Diastolic Heart Failure In critical illness, limited data are available in the literature. Diastolic heart failure definition in critical illness is basically the same as in CHF and the diagnosis is also based on the association of heart failure symptoms and a preserved LVEF. The factors that promote fluid overload and precipitate heart failure are similar in diastolic heart failure and systolic heart failure [13]. If we consider acute diastolic heart failure as a pathological situation leading to an impairment in LV diastolic filling, numerous clinical situations could be considered as acute diastolic dysfunction. For example, acute tamponade, acute right heart failure, or acute mitral regurgitation may lead to LV filling abnormalities [14]. Acute settings discussed below are those in which LV diastolic properties are truly impaired. This includes acute exacerbation of chronic diastolic heart failure, hypertensive crisis, severe sepsis, and myocardial ischemia. z Epidemiology It seems clear that the prevalence and the prognosis of diastolic heart failure are highly dependant on age, gender, and above all the method used to diagnose diastolic heart failure. Masoudi et al. [15] published in 2003 an epidemiological study in which 19 710 patients suffering from heart failure were analyzed. Thirty five percent had preserved LVEF. Among them, 79% were women, whereas only 49 of the 65% suffering from systolic heart failure were women. Patients with diastolic heart failure were 1.5 years older than those with impaired ejection fraction. Zile and Brutsaert [16] reviewed the data published during the last decade and found that: in patients < 50 years, diastolic heart failure represented < 15% of the cause of CHF; 50±70 years, the proportion rose to 33%, and > 70 years, up to 70% of the CHF were due to diastolic heart failure. The morbidity from diastolic heart failure remains very high, with a 1-year readmission rate approaching 50%. The morbidity varies according to age and underlying diseases [16, 17]. Data published in the early 90s reported less annual mortality in diastolic heart failure than in systolic heart failure: 5 to 8% in diastolic heart failure versus 10 to 15% in systolic heart failure [18, 19]. More recent studies have reported higher mortality rates. Chen and colleagues [20] analyzed all inhabitants of Olmsted County, Minnesota, between 1996 and 1997 with a new diagnosis of diastolic heart failure. They reported mortality rates as high as 29% at 1 year, 39% at 2 years, and 60% at 3 years. Again, it appears that age and the criteria chosen for the diagnosis of diastolic heart failure can strongly affect the mortality rates. z Pathophysiology of Diastolic Heart Failure Left Ventricular Pressure/volume Relationship Systolic, diastolic, and combined heart failure are commonly described using the plotting of LV pressure-volume (P/V) loops. In case of diastolic dysfunction (Fig. 1), the LV chamber is unable to fill at low left-atrial pressures resulting in abnormalities in the P/V relationship during diastole. The diastolic P/V curve (compliance curve) is displaced upward and to the 199 200 R. Pirracchio and A. Mebazaa Fig. 1. Modification of the pressure/volume loop in heart failure with normal ejection fraction (HFNEF) also named diastolic heart failure, associating a shift in the end-diastolic pressure-volume relationship (EDPVR) without any change in the endsystolic pressure-volume relationship (ESPVR). From [46] with permission Fig. 2. Pressure/volume (P/V) loops in two patients with diastolic heart failure before (dashed line) and after (dark solid line) sustained isometric handgrip. From [21] with permission left. Thus, for a given end-diastolic volume, end-diastolic pressures (also assessed by the pulmonary artery occlusion pressure [PAOP]) are increased. Kawaguchi et al. [21] recently demonstrated that although normal at baseline, P/V loops can be altered during effort. Maneuvers like sustained isometric handgrips can uncover a NYHA stade 2 diastolic heart failure (Fig. 2). Diastolic Heart Failure and Critical Illness Fig. 3. Left ventricular (LV) pressure/volume loops in combined systolo-diastolic heart failure. LVEDP: left ventricular enddiastolic pressure In case of systolic dysfunction (Fig. 3), LV contractility is depressed resulting in abnormalities in the P/V relationship during systole. The end-systolic P/V slope (LV systolic elastance slope) is shifted downward and to the right. In addition, the LV end-systolic and end-diastolic volumes are increased. The P/V loop is shifted upward and to the right but remains on the same diastolic P/V curve (LV compliance curve). Some patients may have combined systolic and diastolic dysfunction (Fig. 3): a modest increase in end-diastolic volume may result in a large increase in end-diastolic pressure if ventricular chamber compliance is markedly altered. Diastole: New Concepts According to Zile and Brutsaert [16], diastole can be defined as ªthe time period during which the myocardium loses its ability to generate force and shorten and returns to an unstressed length and forceº. Basically, this period represents the part of heart revolution during which the ventricles are filling. Thus diastolic heart failure occurs when the ventricular chamber is unable to accept a volume of blood sufficient to maintain cardiac output at normal diastolic pressures. The diastole process can be divided into two phases: the first represents LV pressure decline at constant volume, so called isovolumic relaxation; the second is LV chamber filling so called auxotonic relaxation. From a cellular point of view, relaxation is a high energy-consuming process. Release of calcium from troponin C, detachment of the actin-myosin cross-bridge, phosphorylation of phospholamban necessary to activate the ATPase-induced calcium sequestration into the sarcoplasmic reticulum, sodium/calcium exchanger-induced extrusion of calcium from the cytoplasm, and return of the sarcomere to its rest length are all energy consumers. Zile et al. recently performed a multicenter, prospective study using cardiac catheterization and echocardigraphy to assess the diastolic properties of the left ventricle in 47 patients suffering from diastolic heart failure and 10 normal controls [22]. The authors concluded that diastolic heart failure is characterized by alteration of both LV active relaxation and passive stiffness that could be assessed by the following measures (Fig. 4): 201 202 R. Pirracchio and A. Mebazaa Fig. 4. Diagram of the method used to correct the measured value of left ventricular minimal diastolic pressure for slow relaxation rate. Assuming the physiological concept that active relaxation could be completed after 3.5 s [47], it is possible to plot the decrease in the left ventricular pressure from the point of aortic valve closure to the theoretical time at which ventricular pressure would approach zero in the absence of filling. By measuring the time from the closure of the aortic valve to Pmin, it is possible to determine the contribution of active relaxation to the left ventricular minimal pressure (Pmin). Thereafter, by subtracting the pressure contribution of slowed relaxation from Pmin, it is possible to obtain a corrected pressure tracing and Pmin, which are used to calculate the corrected passive-stiffness constant. From [22] with permission z z z z s is the time constant of the isovolumic relaxation Pmin is the LV minimal pressure after the opening of the mitral valve PPre-A is the LV pressure just before atrial contraction EDP is the end-diastolic pressure just after the atrial contraction. Zile and colleagues [22] showed that in diastolic heart failure, in contrast to normal subjects, relaxation was incomplete at the time of Pmin. Thus, s was abnormal and Pmin increased with a positive correlation between s and Pmin. In their study, incomplete relaxation accounted for 7 Ô 1 mmHg of the measured Pmin. The authors also reported increased EDP and decreased end diastolic volume (EDV), suggesting increased ventricular stiffness in diastolic heart failure patients. These data suggest that patients with heart failure and preserved ejection fraction have significant abnormalities in both active relaxation and passive stiffness. Diastolic Heart Failure and Critical Illness Antithesis: More than a Specific Alteration of Diastole? Some authors recently emphasized that while diastolic parameters are often abnormal in heart failure with normal ejection fraction, they are not necessarily the major component of the dysfunction, nor do they necessarily explain the clinical features. Leite-Moreira et al. remind us that any rise in LV afterload can affect diastole by prolonging relaxation, compromising filling and elevating end-diastolic pressures [23]. Kawaguchi et al. measured LV P/V relations in 10 patients supposedly suffering from diastolic heart failure, 9 asymptomatic normotensive age-matched subjects, 14 asymptomatic normotensive young subjects, and 25 age- and blood-pressurematched controls [21]. The authors reported a significant increase in both arterial and end-systolic elastance (Ees, Ea) in diastolic heart failure patients and a positive correlation between these two parameters. End-diastolic P/V relations were shifted upward in diastolic heart failure patients but this study clearly emphasizes the fact that end-diastolic P/V relation shift depends on the loading conditions. On the basis of such results, the authors discussed the following hypothesis: diastolic heart failure is essentially due to a combined increase in Ees and Ea. This can influence heart function in several ways: limitation of contractile reserve, high systolic pressure sensitivity to cardiac loading leading to huge hypertensive responses during exertion, increase in myocardial energy consumption, and delay in ventricular chamber relaxation. According to Kawaguchi et al., diastolic dysfunction is present in CHF with normal ejection fractions, but the nature of end-diastolic P/V relations are highly dependent on loading conditions and not merely due to diastolic dysfunction. z Clinical Presentations Chronic Diastolic Heart Failure Diastolic heart failure generally occurs in women, in the elderly (50% after 70 years of age), and in those with a history of hypertension. Apart from this, the clinical presentation of diastolic heart failure has no other specificity and the diagnosis is made based on the presence of symptoms of heart failure with preserved systolic function. Table 2 summarizes the prevalence of specific symptoms of CHF in systolic versus diastolic heart failure [16]. The most frequent causes of diastolic heart failure are listed in Table 3 [24]. Diastolic Heart Failure in Acute Situations Acute Hypertensive Crisis: Ghandi and colleagues [25], recently performed a prospective observational study focusing on echocardiographic profiles at H0, H24 and H72 in patients presenting with acute pulmonary edema and severe arterial hypertension. They wanted to test the hypothesis that such patients suffer from a transient LV systolic dysfunction due to the hypertensive crisis. By contrast to their initial hypothesis, they found that the LVEF and the regional wall motion were similar during the acute episode and after 24 and 72 h of adequate treatment. Moreover 50% of their patients had preserved ejection fraction (LVEF > 50%) and 89% of the patients who had a preserved ejection fraction after treatment also had no sign of 203 204 R. Pirracchio and A. Mebazaa Table 2. Prevalence of specific symptoms and signs in systolic (SHF) vs diastolic (DHF) heart failure [16]. Data are expressed as percent of patients in each group presenting with the specified symptom or sign Symptoms z Dyspnea on exertion z Paroxysmal nocturnal dyspnea z Orthopnea Physical examination z Jugular venous distension z Rales z Displaced apical impulse z S3 z S4 z Hepatomegaly z Edema Chest radiograph z Cardiomegaly z Pulmonary venous hypertension DHF (EF > 50%) SHF (EF < 50%) 85 55 60 96 50 73 35 72 50 45 45 15 30 46 70 60 65 66 16 40 90 75 96 80 EF: ejection fraction Table 3. Major causes of diastolic heart failure [24] Myocardial z Impaired relaxation ± Epicardial or microvascular ischemia ± Myocyte hypertrophy ± Cardiomyopathies ± Aging ± Hypothyroidism z Increased passive stiffness ± Diffuse fibrosis ± Post-infarct scarring ± Myocyte hypertrophy ± Infiltrative (e.g., amyloidosis, hemochromatosis, Fabry's disease) Endocardial z Fibroelastosis z Mitral or tricuspid stenosis Epicardial/Pericardia z Pericardial constriction z Pericardial tamponade Coronary microcirculation z Capillary compression z Venous engorgement Other z Volume overload of the contralateral ventricle z Extrinsic compression by tumor Diastolic Heart Failure and Critical Illness systolic dysfunction during the acute episode. Similarly, in patients with an impaired ejection fraction, no differences were found between H0, H24 and H72, suggesting that acute diastolic failure may play a major role also in patients with baseline systolic dysfunction. The pathophysiology of transient diastolic heart failure in hypertensive crisis remains poorly understood but it seems like diastolic heart failure could be uncovered by an acute hypertensive crisis. In case of diastolic heart failure at rest, it is clear that a small increase in LV end-diastolic volume (LVEDV) will lead to a marked elevation in LV end-diastolic pressure (LVEDP). But the explanation is less clear in patients without any diastolic dysfunction at rest. Some authors proposed that hypertensive crisis would lead to a huge increase in coronary perfusion pressure and thus in coronary turgor [26]. Nevertheless, it is unlikely that an increase in coronary blood volume can cause by itself a significant increase in wall thickness. Myocardial Ischemia: Pennock and colleagues [27] analyzed by echocardiographic and Doppler studies early and late hemodynamic consequences of a circumflex artery ligation in a rabbit model. One hour after the experimental infarct, the rabbits exhibited significant alteration of the LV filling pattern: decrease in E and A waves, A wave reversal velocities, and increase in the mean pulmonary venous systolic-todiastolic ratio. Three weeks after the coronary ligation, the rabbits still exhibited significant abnormalities in filling pattern. Stugaard and colleagues [28] assessed LV diastolic function in 20 patients during coronary angioplasty and in 8 anesthetized dogs during an experimental coronary occlusion. Diastolic function was explored using a recent Doppler technology, called M-mode Doppler, which allows determination of the time difference between the occurrence of the peak velocity in the apical region and in the mitral tip. The authors reported, in their patients, a significant increase in time difference in comparison with normal values. Coronary artery occlusion in dogs resulted in the same increase in time difference. Moreover, the evolution in time difference was significantly correlated with the variation in time constant of isovolumetric relaxation. Interestingly, the authors tried to investigate whether the changes in filling patterns were associated with ischemic induced tachycardia, increase in intracavitary pressures, or reduction in stroke volume rather than with the ischemic process itself. To answer this question, they performed successively pacing tachycardia, volume loading and caval restriction. None of these procedures significantly altered the time difference. Sepsis: The role of diastolic dysfunction in septic patients has been questioned since the late 1980s. Stahl et al. showed in 1990 that, in a canine model of hyperdynamic sepsis, myocardial compliance was significantly altered [29]. Jafri et al. published, in the same year, a transmitral Doppler analysis of 13 patients in septic shock, 10 with sepsis without shock, and 33 controls. They reported that, in septic shock as well as in sepsis without shock, the LV filling pattern was significantly altered in comparison with controls [30]. More recently, Poelaert and colleagues [31] characterized systolic and diastolic function in 25 consecutive patients in vasopressor dependant septic shock, using transesophageal echocardiography (TEE) and pulmonary artery catheters. They found that 8 of the 25 patients had no regional wall motion abnormality and a normal LV filling pattern (transmitral E/A wave ratio > 1; pulmonary vein S/D wave ratio > 1); 11 had evidence of abnormal left auricular filling (S/D < 1) but with a preserved systolic function and E/A wave ratio. According to the investigators, transmitral flow in this group could be considered as 205 206 R. Pirracchio and A. Mebazaa `pseudo-normalized'. Finally, 6 of the 25 patients exhibited both systolic and diastolic dysfunction. The authors concluded ªcardiac effects of septic shock can be expressed in various degrees, ranging from a normal pattern, through diastolic dysfunction up to both poor LV systolic and diastolic function resulting in combined cardiogenic-septic shockº [31]. It should also be emphasized that impairment of diastolic properties could be an independent predictor of mortality in severe sepsis [32]. z Supplementary Investigations Cardiac Catheterization The gold standard for the diagnosis of diastolic heart failure is still cardiac catheterization with the assessment of increased ventricular filling pressures at normal chamber volumes and preserved systolic function. With the use of a high-fidelity micromanometer catheter, it is possible to acquire various data including LV pressure, rate of LV pressure decline (dP/dt), and the time constant of isovolumic relaxation (s). Diastolic heart failure is characterized by a rise in LVEDP. Zile et al. found a LVEDP above 16 mmHg in 92% of patients with heart failure and normal ejection fraction [12]. Relaxation abnormality is characterized by an increase in the time constant of isovolumic relaxation. In the series of Zile et al., s was abnormal (³ 48 ms) in 79% of the patients. Chamber stiffness can be assessed by analyzing the diastolic P/V relationship; the stiffness is represented by the slope of the tangent drawn to the curve at any point. Thus, operating stiffness changes throughout filling: lower at the beginning, higher at the end. If LV stiffness increases, the P/V curve is shifted upward and to the left, so that at any point the slope of the tangent becomes steeper. Echocardiography Echocardiography provides some fundamental information, such as the normality of LVEF (LVEF > 50%). As demonstrated by Gandhi et al., measurements of ejection fraction even performed several days after an episode of acute exacerbation of CHF correlate with acute measurements [25]. Several echographic criteria have been studied in order to provide a non-invasive assessment of LV diastolic function. The first is the mitral inflow profile. This flow usually has two components: the E wave, which reflects early diastolic filling, and the A wave, which represents the subsequent contribution from atrial systole. These waves are influenced by LV relaxation, LV compliance, and atrial pressure. Normal diastole is characterized by a predominant E wave, showing that most of the LV filling occurs during the early phase of diastole. Mitral inflow abnormalities are of three types: z in mild diastolic dysfunction, relaxation is impaired, and atrial contraction contributes relatively more to ventricular filling: A wave > E wave, with prolonged E wave deceleration time (usually > 240 ms) z in moderate diastolic dysfunction, relaxation is impaired, LV compliance is decreased, and atrial pressure increased: pseudonormal pattern with an E wave again predominant, but the E wave deceleration time is shorter Diastolic Heart Failure and Critical Illness z in severe diastolic dysfunction, LV compliance is extremely low: restrictive pattern with high E wave velocity, usually more than twice the A wave velocity. Zile et al. reported a lack of sensitivity of the mitral inflow analysis for the diagnosis of diastolic heart failure. In their study [12], the E/A ratio was abnormal in only 48% of the patients presenting signs of CHF with a normal ejection fraction. The E wave deceleration time was found to be more sensitive (abnormal in 64% of the patients). Pulmonary vein flow can also be measured. There are two waves of pulmonary vein flow, one during systole, the other during diastole. The elevation of the left atrial pressure impairs atrial filling and the pulmonary vein diastolic wave becomes predominant. Nevertheless, pulmonary vein flow abnormalities poorly discriminate systolic and diastolic heart failure. New, promising modalities like Doppler tissue imaging or color M-mode mitral flow propagation wave need to be validated [33, 34]. Other: Neuroendocrine Profile B-type natriuretic peptide (BNP) is now recognized as a specific marker of heart failure in patients presenting with acute dyspnea [35]. This peptide also seems to be of interest for the distinction of diastolic heart failure and lung disease in emergency settings. In a study by Maisel et al., when patients with diastolic heart failure were compared with patients without CHF, a BNP value of 100 pg/ml had a sensitivity of 86%, a negative predictive value of 96%, and an accuracy of 75% for detecting abnormal diastolic dysfunction [36]. In this series, patients with diastolic heart failure had significantly lower BNP levels than those with systolic heart failure (413 pg/ml vs 821 pg/ml, p < 0.001). Nevertheless, the authors concluded that BNP adds a modest discriminatory value in differentiating diastolic from systolic heart failure. z Treatment Very few data are currently available concerning the therapeutic strategy for diastolic heart failure. The guidelines are essentially based on pathophysiological concepts and on a small number of prospective clinical trials. General Treatment The general treatment of diastolic heart failure has two major goals: to limit the consequences of the cardiac filling abnormalities and to control the factors responsible for the diastolic dysfunction. Symptom-targeted therapy should focus on the reduction of pulmonary congestion at rest and during exercise. The two ways of reducing pulmonary capillary pressure are to optimize blood volume and to improve LV filling. LV diastolic pressures can be substantially decreased by the reduction in LV diastolic volumes. Indeed, because of the steep diastolic P/V relation, a small decrease in diastolic volume can lead to a great decrease in diastolic pressure. Thus, diuretics to reduce global blood volume and nitrates to decrease central blood volume could be considered as a first step of symptomatic treatment. The second step of symptom-tar- 207 208 R. Pirracchio and A. Mebazaa geted therapy should focus on improving diastolic filling. Therefore, heart rate control should be considered as a major issue. In fact, tachycardia and non-sinus rhythms are poorly tolerated in patients with diastolic heart failure. First, rapid heart rates induce an increase in myocardial oxygen consumption, and a decrease in coronary perfusion time, both promoting myocardial ischemia even in the absence of underlying coronary disease. Second, tachycardia may shorten diastolic time and thus lead to an incomplete filling. Third, recent data suggest that, in diastolic heart failure, relaxation velocity does not increase in response to tachycardia and may even decrease. This may contribute to the elevation of the end diastolic pressures. Furthermore, the loss of sinus rhythm and thus atrial systole is usually poorly tolerated. Beta-blockers, nondihydropyridine calcium-channel blockers like verapamil can be prescribed in order to prevent tachycardia and to improve filling [37, 38]. Finally, it is still not clear whether digitalis may be of interest in the treatment of diastolic heart failure. In the Digitalis Investigation Group trial, the subgroup of patients with normal ejection exhibited fewer symptoms and lower hospitalization rates under digitalis treatment. As long as the pathophysiological interest of digitalis drugs remains unclear in diastolic heart failure, more evidence is needed of their effects before extending their use to these patients. Specific Treatment The renin-angiotensin-aldosterone system seems to play a great role in the development of diastolic heart failure and particularly in myocardial remodeling and in fluid retention. Naturally, ACE inhibitors, angiotensin receptor antagonists, and aldosterone antagonists have been proposed in the treatment of diastolic heart failure. A small short-term study performed by Aronow and colleagues focused on the effect of enalapril on diastolic heart failure in elderly patients with prior myocardial infarction [39] and reported a benefit in terms of exercise capacity. The CHARMpreserved study was a multicenter, randomized, double blinded study comparing, in diastolic heart failure, the effects of a selective angiotensin-receptor blocking agent (candesartan) versus a placebo [40]. Between 1999 and 2000, 3023 patients NYHA class II to IV, with a LVEF higher than 40% were enrolled in the study (1514 in the candesartan group, 1509 in the placebo group). After 36 months of follow-up, the authors could only conclude that candesartan significantly reduced the rate of hospitalization. No other differences were observed between the two groups. Losartan, another angiotensin-receptor blocker has been shown to increase exercise tolerance [41]. New agents targeting intracellular calcium homeostasis are currently under evaluation. MCC-135 is one of these drugs, which is supposed to improve calcium reuptake by the sarcoplasmic reticulum. MCC-135 is currently under evaluation in a phase II, double-blind, placebo-controlled study in patients suffering from CHF NYHA II and III and either systolic or diastolic heart failure [42]. Levosimendan is a calcium sensitizer modulating the interaction between troponin and calcium. This inotropic drug has recently been proposed to improve cardiac performance after an acute episode of myocardial ischemia [43]. Twenty-four patients were randomized after percutaneous angioplasty to receive either placebo or levosimendan. In the treated group, LVEDV and the time constant of isovolumic LV pressure fall significantly decreased, indicating an obvious improvement in the diastolic function. Diastolic Heart Failure and Critical Illness Finally, nitric oxide (NO)-donor effects have also been investigated. Paulus et al. [44] performed intracoronary injections of sodium nitroprusside in normal hearts. The authors showed that NO-donors caused an earlier onset of LV relaxation, a fall in LV minimum and end-diastolic pressures, an increase in LVEDV and a down and rightward displacement of the LV diastolic P/V relation. These results are consistent with a direct NO-induced improvement in diastolic function. Interestingly, the stimulation of endogenous NO release from the coronary endothelium, by intracoronary infusion of a substance P agonist, produced similar results [45]. z Conclusion In summary, diastolic heart failure is a very common pathology, the incidence of which is frequently underestimated. While diastolic heart failure is recognized as the mechanism involved in CHF with a preserved LV function, it seems that diastolic dysfunction can also account for acute heart failure occurring in critical care situations. Hypertensive crisis, sepsis, and myocardial ischemia are frequently associated with acute diastolic heart failure. The diastolic dysfunction can affect either active relaxation, passive stiffness, or both. With a better understanding of cardiomyocyte function, intracellular calcium metabolism impairment appears to be involved frequently in the development of diastolic failure. Symptomatic treatment focuses on the reduction of pulmonary congestion and the improvement of LV filling. Specific treatments are lacking, but encouraging data are emerging concerning the use of renin-angiotensin-aldosterone axis blockers, NO donors, or new agents such as levosimendan. References 1. Kupari M, Lindroos M, Iivanainen AM, Heikkila J, Tilvis R (1997) Congestive heart failure in old age: prevalence, mechanisms and 4-year prognosis in the Helsinki Ageing Study. J Intern Med 241:387±394 2. Senni M, Tribouilloy CM, Rodeheffer RJ, et al (1998) Congestive heart failure in the community: a study of all incident cases in Olmsted County, Minnesota, in 1991. Circulation 98:2282±2289 3. Mosterd A, Hoes AW, de Bruyne MC, et al (1999) Prevalence of heart failure and left ventricular dysfunction in the general population; The Rotterdam Study. Eur Heart J 20:447±455 4. Vasan RS, Larson MG, Benjamin EJ, Evans JC, Reiss CK, Levy D (1999) Congestive heart failure in subjects with normal versus reduced left ventricular ejection fraction: prevalence and mortality in a population-based cohort. J Am Coll Cardiol 33:1948±1955 5. Remes J, Miettinen H, Reunanen A, Pyorala K (1991) Validity of clinical diagnosis of heart failure in primary health care. Eur Heart J 12:315±321 6. Vasan RS, Benjamin EJ, Levy D (1995) Prevalence, clinical features and prognosis of diastolic heart failure: an epidemiologic perspective. J Am Coll Cardiol 26:1565±1574 7. European Study Group on Diastolic Heart Failure (1998) How to diagnose diastolic heart failure. Eur Heart J 19:990±1003 8. Vasan RS, Levy D (2000) Defining diastolic heart failure: a call for standardized diagnostic criteria. Circulation 101:2118±2121 9. Hunt SA, Baker DW, Chin MH, et al (2001) ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to revise the 1995 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol 38:2101±2113 209 210 R. Pirracchio and A. Mebazaa 10. Remme WJ, Swedberg K (2001) Guidelines for the diagnosis and treatment of chronic heart failure. Eur Heart J 22:1527±1560 11. Zile MR (2003) Diastolic heart failure. Diagnosis, prognosis, treatment. Minerva Cardioangiol 51:131±142 12. Zile MR, Gaasch WH, Carroll JD, et al (2001) Heart failure with a normal ejection fraction: is measurement of diastolic function necessary to make the diagnosis of diastolic heart failure? Circulation 104:779±782 13. Tsuyuki RT, McKelvie RS, Arnold JM, et al (2001) Acute precipitants of congestive heart failure exacerbations. Arch Intern Med 161:2337±2342 14. Pierard LA, Lancellotti P (2004) The role of ischemic mitral regurgitation in the pathogenesis of acute pulmonary edema. N Engl J Med 351:1627±1634 15. Masoudi FA, Havranek EP, Smith G, et al (2003) Gender, age, and heart failure with preserved left ventricular systolic function. J Am Coll Cardiol 41:217±223 16. Zile MR, Brutsaert DL (2002) New concepts in diastolic dysfunction and diastolic heart failure: Part I: diagnosis, prognosis, and measurements of diastolic function. Circulation 105:1387±1393 17. Aurigemma GP, Gaasch WH (2004) Clinical practice. Diastolic heart failure. N Engl J Med 351:1097±1105 18. Setaro JF, Soufer R, Remetz MS, Perlmutter RA, Zaret BL (1992) Long-term outcome in patients with congestive heart failure and intact systolic left ventricular performance. Am J Cardiol 69:1212±1216 19. Judge KW, Pawitan Y, Caldwell J, Gersh BJ, Kennedy JW (1991) Congestive heart failure symptoms in patients with preserved left ventricular systolic function: analysis of the CASS registry. J Am Coll Cardiol 18:377±382 20. Chen HH, Lainchbury JG, Senni M, Bailey KR, Redfield MM (2002) Diastolic heart failure in the community: clinical profile, natural history, therapy, and impact of proposed diagnostic criteria. J Card Fail 8:279±287 21. Kawaguchi M, Hay I, Fetics B, Kass DA (2003) Combined ventricular systolic and arterial stiffening in patients with heart failure and preserved ejection fraction: implications for systolic and diastolic reserve limitations. Circulation 107:714±720 22. Zile MR, Baicu CF, Gaasch WH (2004) Diastolic heart failure ± abnormalities in active relaxation and passive stiffness of the left ventricle. N Engl J Med 350:1953±1959 23. Leite-Moreira AF, Correia-Pinto J, Gillebert TC (1999) Afterload induced changes in myocardial relaxation: a mechanism for diastolic dysfunction. Cardiovasc Res 43:344±353 24. Angeja BG, Grossman W (2003) Evaluation and management of diastolic heart failure. Circulation 107:659±663 25. Gandhi SK, Powers JC, Nomeir AM, et al (2001) The pathogenesis of acute pulmonary edema associated with hypertension. N Engl J Med 344:17±22 26. Wexler LF, Grice WN, Huntington M, Plehn JF, Apstein CS (1989) Coronary hypertension and diastolic compliance in isolated rabbit hearts. Hypertension 13:598±606 27. Pennock GD, Yun DD, Agarwal PG, Spooner PH, Goldman S (1997) Echocardiographic changes after myocardial infarction in a model of left ventricular diastolic dysfunction. Am J Physiol 273:H2018±2029 28. Stugaard M, Smiseth OA, Risoe C, Ihlen H (1993) Intraventricular early diastolic filling during acute myocardial ischemia, assessment by multigated color m-mode Doppler echocardiography. Circulation 88:2705±2713 29. Stahl TJ, Alden PB, Ring WS, Madoff RC, Cerra FB (1990) Sepsis-induced diastolic dysfunction in chronic canine peritonitis. Am J Physiol 258:H625±633 30. Jafri SM, Lavine S, Field BE, Bahorozian MT, Carlson RW (1990) Left ventricular diastolic function in sepsis. Crit Care Med 18:709±714 31. Poelaert J, Declerck C, Vogelaers D, Colardyn F, Visser CA (1997) Left ventricular systolic and diastolic function in septic shock. Intensive Care Med 23:553±560 32. Munt B, Jue J, Gin K, Fenwick J, Tweeddale M (1998) Diastolic filling in human severe sepsis: an echocardiographic study. Crit Care Med 26:1829±1833 33. Garcia MJ, Thomas JD, Klein AL (1998) New Doppler echocardiographic applications for the study of diastolic function. J Am Coll Cardiol 32:865±875 Diastolic Heart Failure and Critical Illness 34. Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quinones MA (1997) Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 30:1527±1533 35. Morrison LK, Harrison A, Krishnaswamy P, Kazanegra R, Clopton P, Maisel A (2002) Utility of a rapid B-natriuretic peptide assay in differentiating congestive heart failure from lung disease in patients presenting with dyspnea. J Am Coll Cardiol 39:202±209 36. Maisel AS, McCord J, Nowak RM, et al (2003) Bedside B-Type natriuretic peptide in the emergency diagnosis of heart failure with reduced or preserved ejection fraction. Results from the Breathing Not Properly Multinational Study. J Am Coll Cardiol 41:2010±2017 37. Aronow WS, Ahn C, Kronzon I (1997) Effect of propranolol versus no propranolol on total mortality plus nonfatal myocardial infarction in older patients with prior myocardial infarction, congestive heart failure, and left ventricular ejection fraction > or = 40% treated with diuretics plus angiotensin-converting enzyme inhibitors. Am J Cardiol 80:207±209 38. Setaro JF, Zaret BL, Schulman DS, Black HR, Soufer R (1990) Usefulness of verapamil for congestive heart failure associated with abnormal left ventricular diastolic filling and normal left ventricular systolic performance. Am J Cardiol 66:981±986 39. Aronow WS, Kronzon I (1993) Effect of enalapril on congestive heart failure treated with diuretics in elderly patients with prior myocardial infarction and normal left ventricular ejection fraction. Am J Cardiol 71:602±604 40. Yusuf S, Pfeffer MA, Swedberg K, et al (2003) Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet 362:777±781 41. Warner JG Jr, Metzger DC, Kitzman DW, Wesley DJ, Little WC (1999) Losartan improves exercise tolerance in patients with diastolic dysfunction and a hypertensive response to exercise. J Am Coll Cardiol 33:1567±1572 42. Zile M, Gaasch W, Little W, et al (2004) A phase II, double-blind, randomized, placebo-controlled, dose comparative study of the efficacy, tolerability, and safety of MCC-135 in subjects with chronic heart failure, NYHA class II/III (MCC-135-GO1 study): rationale and design. J Card Fail 10:193±199 43. Sonntag S, Sundberg S, Lehtonen LA, Kleber FX (2004) The calcium sensitizer levosimendan improves the function of stunned myocardium after percutaneous transluminal coronary angioplasty in acute myocardial ischemia. J Am Coll Cardiol 43:2177±2182 44. Paulus WJ, Vantrimpont PJ, Shah AM (1994) Acute effects of nitric oxide on left ventricular relaxation and diastolic distensibility in humans. Assessment by bicoronary sodium nitroprusside infusion. Circulation 89:2070±2078 45. Paulus WJ, Vantrimpont PJ, Shah AM (1995) Paracrine coronary endothelial control of left ventricular function in humans. Circulation 92:2119±2126 46. Burkhoff D, Maurer MS, Packer M (2003) Heart failure with a normal ejection fraction: is it really a disorder of diastolic function? Circulation 107:656±658 47. Weisfeldt ML, Weiss JL, Frederiksen JT, Yin FC (1980) Quantification of incomplete left ventricular relaxation: relationship to the time constant for isovolumic pressure fall. Eur Heart J (Suppl):119±129 211