* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download colloid osmotic pressures
Countercurrent exchange wikipedia , lookup
Cushing reflex wikipedia , lookup
Intracranial pressure wikipedia , lookup
Homeostasis wikipedia , lookup
Common raven physiology wikipedia , lookup
Circulatory system wikipedia , lookup
Haemodynamic response wikipedia , lookup
Biofluid dynamics wikipedia , lookup
Cardiac output wikipedia , lookup
Hemodynamics wikipedia , lookup
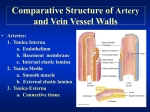
Vascular physiology Introduction • The majority of body cells are not directly contact with the external environment , but these cells must make exchanges with this environment . e.g.O2 pickup and CO2 removal • Blood vessels is passageway of substance transportation and bring about the function of exchanging the substance • All blood pumped by the right side of heart passes through the lungs for O2 pickup and CO2 removal • The blood pumped by the left side of the heart is parceled out in various proportions to the systemic organs through a parallel arrangement of vessels • Advantages: each organ can be independently adjusted without directly influencing blood flow through any other organ Distribution of cardiac output at rest This distribution of CO can be adjusted as needed Reconditioning organ – digestive organs, kidneys and skin Basic organization of the cardiovascular system the arterioles ,capillaries, and venules are collectively referred to as he microcirculation Blood vessels • Arteries : carry blood from heart to tissue, elastic vessels • Arterioles: a small artery reaches the organ, resistance vessels • Capillaries: the smallest vessels , exchange vessels • Venules: Capillaries rejoin to form Venules • Veins : leave the organ and then unite to form larger veins that empty blood into heart, capacitance vessels • Microcirculation: Arterioles, Capillaries and Venules Blood flow • Blood flow through vessels depends on the pressure gradient and vascular resistance Flow rate • Flow rate is the volume of blood passing through per unit of time • Flow rate is directly proportional to the pressure gradient and inversely proportional to vascular resistance: F = △P / R Where F = flow rate of blood through a vessel △P = pressure gradient R = resistance of blood vessels F=△P / R = (P1-P2) / R Flow rate --- Pressure gradient • The difference in pressure between the beginning and end of a vessel – main driving force for the blood flow • The greater the pressure gradient forcing blood through a vessel, the greater the rate of flow through that vessel e.g. Relationship of flow to the pressure gradient in a vessel Flow rate is directly proportional to △P , determined by the △P (difference) between two ends of a vessel, not the absolute pressures Flow rate --- Resistance • Definition : A measure of the hindrance to blood flow through a vessel caused by friction between the moving fluid and the stationary vascular walls • F = △P / R • Resistance increases, the △P must increase to maintain the same flow rate. • i.e. when the vessels offer more resistance to flow , the heart must work harder to maintain adequate circulation Flow rate --- Resistance • Resistance to blood flow depends on three factors: --Viscosity of the blood --Vessel length --Vessel radius (important) resistance --viscosity • Viscosity refers to the friction developed between the molecules of a fluid as they slide over each other during flow of the fluid • The greater the viscosity , the greater the resistance to flow. the thicker a liquid , the more viscous it is. viscosity of blood is determined by two factors: (1) the concentration of plasma proteins (2) the number of circulating red blood cells (important) At the normal situation , these two factors remain constant resistance • The greater the vessels surface area in contact with the blood , the greater the resistance to flow. • Surface area is determined by length and radius of the vessel, (length remains constant , so the major determinant of resistance to flow is the radius of vessel) A given volume of blood comes into contact with much more of the surface area of a small-radius vessel than of a large-radius vessel, resulting in greater resistance Resistance and radius • The resistance is inversely proportional to the fourth power of the radius • R∝1/r 4 double the radius decrease the resistance 16 times and therefore increase flow through the vessel sixteenfold (at the same pressure gradient) Relationship of resistance and flow to the vessel radius Same pressure gradient Radius in vessel 2 = 2 times that of vessel 1 Resistance in vessel 2 =1/16 that of vessel 1 flow in vessel 2 = 16 times that of vessel 1 Resistance ∝ 1 / r 4 flow ∝ r 4 Poiseuille’s law • The radius of arterioles is subject to regulate and is the most important factor in the control of resistance to blood flow • The factors that affect the flow rate through a vessel are integrated in Poiseuille’s law: flow rate = π △P r 4 / Where 8η L η = viscosity the flow rate is largely determined by vessel radius Features of blood vessels Vessel type aorta Number one Large arteries arterioles several hundred capillaries half million ten billion Large vein several hundred Thick 2000μm 1000μm 20μm 1μm 500μm Radius 12500μm 2000μm 30μm 3.5μm 5000 μm Area 4.5cm 400 cm2 6000cm2 20cm2 Special Thick, highly elastic wall features larger radius functions Passageway from the heart to the tissues; serve as a pressure reservoir Highly muscular, well-innervated walls; small radius Primary resistance vessels; determine the distribution of CO Vena cava 1500μm 40 cm2 Thin walled; large cross sectional area two 30000μm 18 cm2 Highly distensible; larger radius, thin walled Site of exchange; determine the distribution of ECF between the plasma and interstitial fluid Passageway to the heart from the tissues; serve as a blood reservoir Arteries • Arteries (elastic properties) serve as rapid-transit passageways to the tissues and as a pressure reservoir • Pressure reservoir : providing the driving force for the continued flow of blood to the tissues during cardiac relaxation (elastic properties) Elastin fiber The wall of the aorta in cross section, it is common to all arteries Arteries --- Pressure reservoir • When the heart systole: a greater volume blood enters the artery , only part of them flow into smaller vessels, the left stored in the elastic artery, then storing some of the pressure energy imparted by cardiac contraction in their stretched walls Heart contraction and emptying the elastic arteries distend during cardiac systole as more blood is ejected into them than drains off into the narrow high-resistance arterioles downstream Arteries --- Pressure reservoir • When the heart relaxes: no blood pumping, the stretched arterial walls passively recoil, the recoil pushes the excess blood into the vessels downstream, make the intermittent pump into continuous blood flow Heart relaxing and filling The elastic recoil of arteries during cardiac diastole continues driving the blood forward when the heart is not pumping Arterial blood pressure • Arterial pressure fluctuates during the systole and diastole • Blood pressure : the force exerted by the blood against a vessel wall, depends on the volume of blood contained within the vessel and the vessels’ compliance • compliance:how easily they can be stretched • Unit: K Pa, mm Hg, cm H2O Arterial blood pressure • Systole pressure: 80 - 120mm Hg • during ventricular systole : a stroke volume of blood enters the arteries while 1/3 blood enters the arterioles (the maximum pressure exerted in the arteries) Arterial blood pressure • Diastole pressure: 60 – 80 mm Hg • during ventricular diastole : no blood enters the arteries, while blood continues to leave, driven by elastic recoil (the minimum pressure exerted in the arteries) • The blood pressure does not fall to 0 mm Hg, because the next cardiac contraction occurs and refills before all the blood drains off Measurement of blood pressure Direct measure technique (invasive method) Measurement of blood pressure • Indirectly measurement sphygmomanometry : pressure gauge , cuff stethoscope Indirectly measurement technique (non-invasive) Use of a sphygmomanometer in determining blood pressure . The pressure in the inflatable cuff can be varied to prevent or permit blood flow in the underlying brachial artery Indirectly measurement technique Steps : (1) Cuff is wrapped around the upper arm (2) A stethoscope is placed over the brachial artery at the inside bend of the elbow just below the cuff (3) Inflating air into the cuff, until no sound is heard when cuff pressure is greater than the pressure in the vessel, the vessel is pinched closed so that no blood flows through it. when blood pressure is greater than cuff pressure, the vessel is open and blood flows through (4) Let the air inside the cuff go, during which you can hear the sound caused by blood flow Laminar flow does not create any sound Turbulent flow can be heard Pattern of sounds in relation to cuff pressure compared with blood pressure 1. Cuff pressure > blood pressure . No sound is heard 2. The first sound is heard at peak systolic pressure 3. Intermittent sounds are heard as blood pressure cyclically exceeds cuff pressure Pattern of sounds in relation to cuff pressure compared with blood pressure 4. The last sound is heard at minimum diastolic pressure 5. Blood pressure exceeds cuff pressure through the cardiac cycle. No sound is heard Blood flow through the brachial artery in relation to cuff pressure and sounds When cuff pressure is greater than 120 mm Hg : No blood flows through the vessel. No sound is heard When blood pressure is 120 / 80 mm Hg Blood flow through the brachial artery in relation to cuff pressure and sounds When cuff pressure is between 120 and 80 mm Hg: Blood flow through the vessel is turbulent whenever blood pressure exceeds cuff pressure Intermittent sounds are heard as blood pressure fluctuates throughout the cardiac cycle When blood pressure is 120 / 80 mm Hg Blood flow through the brachial artery in relation to cuff pressure and sounds When cuff pressure is between 120 and 80 mmHg: The first sound can be heard is the indicative of the systolic blood pressure The last sound can be heard is the indicative of the diastole blood pressure When blood pressure is 120 / 80 mm Hg Blood flow through the brachial artery in relation to cuff pressure and sounds When cuff pressure is less than 80 mmHg: Blood flow through the vessel in smooth , laminar fashion No sound is heard The sound is not the heart sound associated with valve closure When blood pressure is 120 / 80 mm Hg • In clinic practice , arterial blood pressure is expressed as systolic pressure over diastolic pressure, with the average blood pressure being 120 / 80 (120 over 80) mm Hg Pulse pressure • The pulse can be felt on the surface of skin is due to the difference systolic and diastolic pressures . This difference is known as the pulse pressure. • When the blood pressure is 120 / 80 mm Hg , pulse pressure is 40 mm Hg (120 mm Hg – 80 mm Hg) Mean arterial pressure (MAP) • Mean arterial pressure is the main driving force for blood flow • MAP is an average pressure, not the halfway value between systolic and diastolic pressure e.g. with a blood pressure of 120 / 80 , MAP is not 100 mm Hg Mean arterial pressure (MAP) • At resting heart rate, about 2 / 3 of the cardiac cycle is diastole and only 1 / 3 is systole. The MAP is closer to diastole pressure. Formula for MAP: • MAP = diastole pressure + 1 / 3 pulse pressure Pressure throughout the systemic circulation Left ventricular pressure swings between a low pressure of 0 mm Hg to 120 mm Hg Arterial blood pressure is of the same magnitude (systole:120 mmHg; diastole:80mm Hg) The pressure in arterioles drop sharply (the high resistance ) The pressure in capillaries, venules and veins decline at a slower rate, it is a nonpulsatile arterioles • Arterioles are the major resistance vessels (reach the organ) • The high degree of arteriolar resistance causes a marked drop in mean pressure. • The advantages of the marked drop pressure : (1) Establishment of pressure gradient (MAP is from 93 to 37 mm Hg) (2) converting the pulsatile systolic-to-diastolic pressure into the nonfluctuating pressure in the capillaries arterioles • The radius (resistance) of arterioles can be adjusted independently , which have two function: (1) To variably distribute the cardiac output , according to the body’s momentary need (intrinsic control) (2) To help regulate arterial blood pressure (extrinsic control) Mechanism of adjustment independently 1. Arteriolar walls structure: (1) very little elastic connective tissue (2) thick layer of smooth muscle is sensitive to local chemical change and a few of circulating hormone (richly innervated by sympathetic nerve) 2. Arteriolar smooth muscle displays a state of vascular tone : (1) myogenic activity (partial constriction) (2) sympathetic fiber supplying the most arterioles continually release NE Normal arteriolar tone Vasodilation Myogenic activity Oxygen decrease Vasoconstriction Caused by Myogenic activity Oxygen increase CO2 decrease Sympathetic stimulation ,vasopressin CO2 increase Sympathetic stimulation Histamine release Heat Intrinsic control (local control ) of arteriolar radius • Local control of arteriolar radius determined the distribution of cardiac output so that blood flow is matched with the tissues’ metabolic needs • The amount of the CO received by each organ is determined by the number and caliber of the arterioles supplying that area Local control caliber of the arterioles The distribution of CO Constant pressure in pipe (MAP) From pump No flow Moderate flow large flow Distribution of the cardiac output at rest and during moderate exercise Total cardiac output is 5000 Total cardiac output is 12500 Extrinsic control of arteriolar radius • Extrinsic control of arteriolar radius is primarily important in the regulation of arterial blood pressure • Two types : -- neural influences (sympathetic nerve is the most important) sympathetic nerve supply arteriolar smooth muscle everywhere in the systemic circulation except in the brain -- humoral influences Extrinsic control of arteriolar radius Changes in arteriolar resistance bring about changes in MAP F = △P / R F: flow of the blood is equal to the cardiac output (Looking at the circulatory system as a whole ) △P : the pressure gradient for the entire systemic circulation is the MAP (for systemic circulation is 93 mm Hg,pulmonary circulation is 15) R: total peripheral resistance is caused by arteriolar resistance (arterioles are the primary resistance vessels) △P = F x R ------- MAP = cardiac output x total peripheral resistance Pressure at end of systemic circulation = 0 mm Hg Pressure at beginning of systemic circulation = MAP (93 mm Hg) The pressure gradient in the systemic circulation Extrinsic control of arteriolar radius △P = F x R MAP = cardiac output x total peripheral resistance So the total peripheral resistance influences the MAP immensely Local control and extrinsic control for arterioles’ radius Local control is more important than extrinsic control when maintaining the blood flow. (e.g. active heart or skeletal muscle) Extrinsic control (sympathetic role) is maintenance the driving force for blood flow note: Brain is an exception (blood vessels have no α receptor), entirely controlled by local mechanism Parasympathetic nerve supply to the arterioles of the penis and clitoris--erection Arteriolar smooth muscle adrenergic receptors Receptor type characteristic Location of the receptor Chemical mediator that binds with the receptor α β2 All arteriolar smooth muscle except in the brain Arteriolar smooth muscle in the heart and skeletal muscle Norepinephrine from sympathetic fibers and the adrenal medulla Epinephrine from the adrenal medulla (greater affinity of this receptor) Epinephrine from the adrenal medulla (less affinity of this receptor) Arteriolar smooth muscle response vasoconstriction vasodilation Total peripheral resistance Blood viscosity Arteriolar radius Number of RBC Local control Local metabolic changes in O2, CO2 (matching blood flow with metabolic needs) Concentration of plasma proteins Extrinsic control Sympathetic activity (exert vasoconstrictor effect) Major factor affecting arteriolar radius Factors affecting total peripheral resistance Capillaries • Capillaries are ideally suited to serve as sites of exchange • Structure : one layer of endothelial cell • no smooth muscle or connective tissue • Function : transfer the substances between blood and tissue (diffusion and no carrier-mediated process) Capillary anatomy Photograph of a capillary bed. The capillaries are so narrow that the RBC must pass through single file 7um A cross section of a capillary (the capillary wall consists of a single layer of endothelial cells) 1um No smooth muscle cell and connective tissue features in capillary bed They minimize diffusion distances while maximizing surface area and time available for exchange 1. Short distance : the rate of exchange increase Thin capillary wall :1μm (the diameter of human hair 100μm) small capillary diameter :7μm no tissue cell is farther than 100μm from a capillary 2. Large area : the rate of exchange increase number :10 -14 billion d area: 600 m2 The structure determined the capillary are ideally suited to enhance diffusion in accordance with Fick’s law of diffusion factor Concentration gradient of substance (ΔC) Permeability (P) Surface area of membrane (A) Molecular weight of substance (MW) Distance (thickness) (ΔX) Rate of diffusion features in capillary bed 3. Slow blood flows : adequate time for exchange , the rate of exchange increase speed of flow is inversely proportional to the total cross-sectional area (6000 cm2 ) velocity of flow ≠ flow rate Flow rate:refers to the volume of blood flowing through a given segment of the circulatory system per unit of time Velocity of flow:refers to the linear speed with which blood flows forward through a given segment of the circulatroy system. Relationship between total cross-sectional area and velocity of flow flow rate is the same at all levels of the circulatory system Three dark area represent equal volume of water Comparison of blood flow and velocity of flow in relation to total cross-sectional area The blood flow rate is the same at all level of the vessel The velocity of flow is inversely proportional to the total cross-sectional area velocity of flow flow rate _____ = total cross-sectional area of vessels at that level Why isn’t capillaries the resistance vessels , even which have smaller radius than arterioles? 1. capillaries’ tremendous total cross-sectional area 2. Capillary caliber cannot be adjusted substances exchanges across the capillary wall Lipid-soluble substance, such as O2 and CO2 , can pass through the endothelial cells by dissolving This pore permit passage of water-soluble substances . e.g. ions ,glucose and amino acid The large, non - lipid - soluble substances are exclude from passage of the pore . e.g. proteins brain:pores are nonexistent liver:big enough for protein though Structure of capillary bed Metarteriole : surround by wisps of smooth muscle cell (SMC) ; thoroughfare channel Precapillary sphincters: SMC no nerve innervated high myogenic tone sensitive to local metabolic changes control the blood flow (like arterioles)-stopcock Capillaries : no SMC , no the function of regulating of blood flow Capillary bed • Many capillaries are not open under resting conditions. (determined by the metabolic activity) • e.g. 10% of the capillaries in resting muscle are open at any moment . When the metabolic activity is changed , the extent of the capillaries opening is more ,result in more blood flow to muscles • Blood flow through a particular tissue (a constant blood pressure ) is regulated by • (1) the degree of resistance offered by the arterioles in the organ (controlled by sympathetic nerve and local factor) • (2) the number of open capillaries (controlled by action of local metabolic factors on precapillary sphincters) Complementary action of precapillary sphincters and arterioles in adjusting blood flow through a tissue in response to changing metabolic needs The function of capillary bed – substance exchange The substance exchange across the capillary walls Exchange between blood and the tissue cells are not made directly. Interstitial fluid acts as the go-between Interstitial fluid acting as an intermediary between blood and cells step1:Diffusion between cell and interstitial fluid: • Passive transport: simple diffusion facilitated diffusion Active transport: carrier-mediated transport vesicular transport step2:Diffusion between capillary and interstitial fluid: • largely passive transport: simple diffusion facilitated diffusion active transport: limited vesicular transport substances exchanges across the capillary wall Lipid-soluble substance, such as O2 and CO2 , can pass through the endothelial cells by dissolving This pore permit passage of water-soluble substances . e.g. ions ,glucose and amino acid The large, non - lipid - soluble substances are exclude from passage of the pore . e.g. proteins The substances exchanges of capillaries The large non-soluble molecules must be exchange in endocytotic-exocytotic vesicles The substance exchange across the capillary walls • The means for the exchanges between blood and surrounding tissues across the capillary walls • (1) passive diffusion down concentration gradients (for exchange of individual solutes) • (2) bulk flow, a volume of protein - free plasma actually filters out of the capillary , mixes with the surrounding interstitial fluid ,and is subsequently reabsorbed. (in contrast to the discrete diffusion of individual solutes down concentration gradients) The substance exchange --- diffusion • Diffusion : individual solute cross primarily by diffusion down concentration gradients (glucose , amino acid , ion). This process repeat itself continuously Independent exchange of individual solutes down their own concentration gradients across the capillary wall The substance exchange --- bulk flow • Bulk flow:determining the distribution of the ECF volume between the vascular and interstitial fluid compartments • Ultrafiltration : when pressure inside the capillary exceeds pressure outside, fluid is pushed out through the pores. • Reabsorption : when inward driving pressures exceed outward pressures across the capillary wall, the fluid will move into the capillaries through the pores. • bulk flow occurs because of differences in the hydrostatic and colloid osmotic pressures between the plasma and interstitial fluid. • (pressure differences exist elsewhere in the circulatory system, only the capillaries have pores that allow fluids to pass ) The substance exchange --- bulk flow • Review • Osmosis: water diffuse down its own concentration gradient from the area of higher water concentration (lower solute concentration) to the area of lower water concentration (higher solute concentration). This net diffusion of water is known as osmosis The substance exchange --- bulk flow • Hydrostatic (fluid) pressure Water moves from side 1 to 2 solute unable to move from side 2 to 1 Water concentration not equal and solute concentration not equal Tendency for water to diffuse by osmosis into side 2 is exactly balanced by opposing tendency for hydrostatic pressure difference to push water into side 1 Osmosis ceases Opposing pressure necessary to completely stop osmosis is equal to osmotic pressure of solution The substance exchange --- bulk flow • The osmotic pressure related directly to the concentration of nonpenetrating solute (plasma protein). The higher solute concentration , the greater osmotic pressure of solution • colloid osmotic pressure • crystal osmotic pressure bulk flow • Bulk flow is responsible for the formation of interstitial fluid. • Four forces influence fluid movement across the capillary wall: • (1) capillary blood pressure (Pc) : definition : the hydrostatic pressure exerted on the inside of the capillary walls by the blood. direction of the force : force fluid out of the capillaries into the interstitial fluid. value: at the arteriolar end is 37 mm Hg , at the venular end is 17 mmHg bulk flow • (2) Plasma-colloid osmotic pressure (πp) definition: a force cause by the colloidal dispersion of plasma protein direction of force : encourage fluid movement into the capillaries (protein concentration gradients ) value : 25 mmHg bulk flow (3) interstitial fluid hydrostatic pressure (Pif) definition: the pressure exerted on the outside of the capillary wall by the interstitial fluid direction of force : force fluid movement into the capillaries value : 1 mmHg bulk flow • (4) interstitial fluid-colloid osmotic pressure (πif) • definition: a force cause by the colloidal dispersion of plasma protein in the interstitial fluid • direction : encourage fluid movement out of the capillaries • value : 0 mm Hg • note:normally the πif does not contribute significantly to bulk flow) bulk flow • The net exchange at a given point across the capillary wall can be calculated using the following equation: • net exchange pressure = (Pc +πif) - (πp + Pif) • outward pressure inward pressure • A positive net exchange pressure (when the outward pressure exceeds the inward pressure) represent an ultrafiltration pressure (11 mm Hg) • A negative net exchange pressure (when the inward pressure exceeds the outward pressure) represent a reabsorption pressure (9 mm Hg) Force at arteriolar end Ultrafiltration occurs at the beginning of the capillary Force at venular end of capillary Reabsorption occurs at the end of the capillary Bulk flow across the capillary wall (ultrafiltration and reabsorption ) Schematic representation of ultrafiltration and reabsorption as a result of imbalances in the forces acting across the capillary wall Net filtration and net reabsorption along the vessel length The inward pressure remains constant throughout the length of the capillary whereas the outward pressure progressively declines In the first half of the vessel, progressively diminishing quantities of fluid are filtered out In the last half of the vessel, progressively increasing quantities of fluid are reabsorbed Bulk flow • The significance of bulk flow: the amount of substance exchange across the capillary wall by bulk flow is extremely small compared to the much larger transfer of solutes by diffusion significance: regulating the distribution of ECF between the plasma and interstitial fluid. (temporary mechanism) e.g. by hemorrhage the plasma volume is reduced and the blood pressure falls. Now the filtration reduced and reabsorption increased. Where is the extra filtered fluid ? On average, the net ultrafiltration pressure starts at 11mmHg at the beginning of the capillary, whereas the net reabsorption pressure only reaches 9mmHg by the vessel’s end. Lymphatic system • lymphatic system is an accessory route by which interstitial fluid can be returned to the blood Lymphatic system--structure • overlapping endothelial cells--valvelike Lymphatic system • • • • return of excess filtered fluid defense against disease transport of absorbed fat return of filtered protein clinical point: • edema—swelling of the tissues because of excess interstitial fluid 1 Reduced concentration of plasma proteins kidney disease; reduced synthesis of plasma proteins as a result of liver disease; a diet deficient in protein; clinical point: • edema—swelling of the tissues because of excess interstitial fluid 2.Increased permeability of the capillary walls tissue injury or allergic reaction clinical point: • edema—swelling of the tissues because of excess interstitial fluid 3.Increased venous pressure-congestive heart failure congestive heart failure clinical point: • edema—swelling of the tissues because of excess interstitial fluid 4.Blockage of lymph vessels—filariasis elephantiasis mosquito-borne parasitie worm veins • Vein serve as a blood reservoir as well as passageways back to the heart • Structure and feature : -- large radius (low resistance) ; -- more collagen fibers, less elastin fibers, -- smooth muscle little inherent myogenic tone highly distensible -- venous smooth muscles is abundantly supplied with sympathetic nerve fiber -- capacitance vessels (storage capacity, at rest more than 60%) veins Percentage of total blood volume in different parts of the circulatory system at rest Venous return central venous pressure: pressure within right atrial and big vein in thoracic cavity significance: detact CVP in case overload as injecting . Venous return • Venous return : the volume of blood entering each atrium per minute from the veins (the venous capacity affect it) • Venous return caused by pressure gradient (determined by cardiac contraction ): At the beginning of vein , mean pressure average 17 mm Hg . The atrial pressure is near 0 mm Hg. The factors that influences venous return (1) Driving pressure impart by the cardiac contraction. (primary factors) (2) sympathetic activity (3) skeletal muscle activity (4) the effect of venous valves (5) respiratory activity (6) effect of cardiac suction Influencing the pressure gradient between the veins and the heart (secondary factors) The factors that influences venous return • Effect of sympathetic activity on venous return • Mobilizing the stored blood : sympathetic stimulation produces venous vasoconstriction , which elevates venous pressure • Decreasing venous capacity: venous return increase , the contractility of heart increase, the cardiac output increase the different outcomes of vasoconstriction in arterioles and veins: Arteriolar vasoconstriction increase the resistance and reduces flow (less blood can enter and flow through a narrowed arteriole) venous Vasoconstriction decrease the capacity and increases flow (narrowing of veins squeezes out more of the blood that is already present in the veins) The factors that influences venous return • Effect of skeletal muscle activity on venous return (1) When skeletal muscle contract, veins are compressed, decreased the venous capacity , increase the venous return •Skeletal pump: one way extra blood stored in the veins is returned to the heart during exercise Skeletal pump enhancing the venous return The factors that influences venous return • (2) Skeletal muscle pump counters the effect of gravity on the venous system -- Gravity force: • When a person is lying down , the gravity force is uniform (no need consider it) • When a person stands up, the gravity force is not uniform (the pressure caused by cardiac contraction and the weight of the column of blood ) 90 mm Hg caused by gravitational effect 10 mm Hg caused by pressure imparted by cardiac contraction (friction loss) Pressure=100 mm Hg P=90mmhg Effect of contraction of the skeletal muscles (as in walking ) completely empties given vein segments, interrupting the column of blood that must be supported by the lower veins The factors that influences venous return • Effect of venous valves on venous return Blood can only be driven forward because the large veins are equipped with one-way valves spaced at 2 to 4cm intervals. Venous valves play a role in conteracting gravitational effect by minimizing the backflow of blood and temporarily supporting portions of the column of blood The factors that influences venous return • Effect of respiratory activity on venous return as a result of respiratory activity, the pressure inside the chest averages 5 mm Hg less than atmospheric pressure. between the lower veins and the chest veins , there is a pressure gradient The factors that influences venous return • Effect of cardiac suction on venous return • During the contraction , the amount of blood pumping increase , the venous return increase • During the relaxation , increasing the vein-to-atria pressure gradient, venous return enhanced Regulation of blood pressure • mean blood pressure is closely regulated (not too high or too low) • When blood pressure is too low, there is no adequate blood flow to tissue • When blood pressure is too high, the workload of heart increased and the risk of small blood vessels damage or rupture increased • MAP=CO X total peripheral resistance • indicates the determinants of MAP MAP=DP+1/3pulse pressure Blood pressure regulation • Two types: • Long-term mechanism: related to the regulation of urine formation and thirst (requiring minutes to days) (humoral regulation) • Short-term mechanism: related to the regulation of CO and total peripheral resistance (within seconds) -Baroreceptor reflex (nervous regulation) Mean arterial blood pressure Cardiac output Heart rate Total peripheral resistance Stroke volume Arteriolar radius Blood viscosity RBC Parasympath -etic activity sympath-etic activity and epinepherine Effective circulatory Blood volume Respirato -ry activity Venous return Cardiac suction Skeletal muscle activity Local control Sympathetic activity and E Extrinsic control Vasopre -ssin Factors influence the BP • Stroke volume: SV increase, the blood amount in the artery increase during systole, systole pressure increase and diastole almost remain constant or increase less (resistance and HR constant) pulse pressure increase The systolic pressure change mainly reflect the change of SV Factors influence the BP • Total peripheral resistance : R increase (CO constant) , the velocity of the blood flow to tissue decrease, the blood amount left in the artery increase (during diastole) , diastole pressure increase largely , pulse pressure decrease . • So diastolic pressure change mainly reflect the change of total peripheral resistance Factors influence the BP • Heart rate : HR increase (SV and total peripheral resistance constant) , the diastole shortening , so blood flow to down-stream tissue decrease, the left blood in artery more than before, so diastolic pressure increase largely , pulse pressure decrease