* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Side Effects
Survey
Document related concepts
Transcript
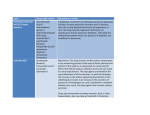
Pharmacologic Management of Hypertension Deborah E. Westbrook, RPh, M.S. Pediatric Clinical Pharmacy Specialist Vidant Medical Center Objectives Review the pharmacologic classes of medications which are most commonly used to manage hypertension in the pediatric patient Recognize compelling indications or patient characteristics which may influence prescribing decisions Know the most common adverse drug reactions associated with each class of medication and how to monitor for these events Discuss the step-wise approach to initiating drug therapy and how to alter drug regimens based on response. Myocardial Contractility Stroke Volume Cardiac Output Blood Pressure Size of vascular compartment Heart Rate Peripheral Resistance ABC’s of Antihypertensive Therapy Angiotensin Converting Enzyme (ACE) Inhibitors Angiotensin Receptor Blockers (ARBs) Beta-Adrenergic Antagonists Calcium Channel Blockers Diuretics ACE Inhibitors Mechanism of Action Inhibits angiotensin I from being converted to angiotensin II by blocking the angiotensin converting enzyme (ACE) Examples of Agents in Class Captopril Enalapril Lisinopril ACE Inhibitors ACE Inhibitors Effect on Blood Pressure Vasodilation ↓ PVR Prevents aldosterone release ↓CO Decreases vasopressin release ↓CO Blocks the CNS release of norepineprhine ↓CO Prevents breakdown of bradykinin ↓PVR ACE Inhibitors Side Effects Decreased Renal Function Hyperkalemia Cough Angioedema Leucopenia Anemia ACE Inhibitors Contraindications Bilateral renal artery stenosis Solitary kidney with renal stenosis Pregnancy ACE Inhibitors Compelling Indications Protein wasting nephropathy (Nephrotic syndrome, FSGS) Polycystic Kidney Disease Diabetes Congestive Heart Failure Angiotensin Receptor Antagonist (ARBs) Mechanism of Action Block AT1 receptors that are stimulated by Angiotensin II Effect on Blood Pressure -Same as ACEi Commonly Prescribed Agents in Class Losartan Valsartan Irbesartan Angiotensin Receptor Antagonists Adrenals Blood Vessels Heart Kidney Pituitary CNS ARBs Side Effects Hyperkalemia Decreased renal function Cough (not as common as with ACEi) Angioedema Contraindications Pregnancy βeta-adrenergic Antagonist Mechanism of Action Block the action of catecholamines on βeta-adrenergic receptors Effect on Blood Pressure ↓CO 1) Decrease heart rate and contractility 2) Decrease renin production ↓PVR 3) Decrease norepinephrine outflow from CNS ↓CO βeta-Blockers β-1 Selective Blocking Agents Metoprolol Atenolol Bisoprolol Non-selective Beta-blocker (block β1 and β2) Propranolol Nadolol Non-selective Beta-blockers with α-1 antagonist action Labetalol Carvedilol βeta- Blockers Side Effects Bronchospasm Bradycardia Fatigue Nightmares Requires Weaning Masks signs and symptoms of hypoglycemia Depression βeta- Blockers Compelling Indications Patients with signs of increased sympathetic drive Pheochromocytoma Use with Caution Athletes Asthmatics Diabetics Calcium Channel Blockers Mechanism of Action Block the influx of calcium into the vasculature and heart muscle Effect on Blood Pressure ↓PVR Vasodilation Decreases contractility ↓CO ø K Ca++ KK Na+ Calcium Channel Blockers K+ Calcium Channel Blockers Dihydropyridine Calcium Channel Blockers Amlodipine Nifedipine Nicardapine Non-dihydropyridine Calcium Channel Blockers Diltiazem Verapamil Calcium Channel Blockers Side Effects Peripheral Edema Flushing Headache Dizziness Reflex tachycardia (Nifedipine) Gingival hypertrophy Calcium Channel Blockers Compelling Indications Renal transplant patients Chronic lung disease Hyperlipidemia Black hypertensive population Protein loosing nephropathies in patients with contraindications to ACEi/ARBs Diuretics Mechanism of Action Increase water and sodium loss in renal tubule Effect on Blood Pressure Decreases blood volume (short term) Decreases stiffness of blood vessels (long term) ↓CO ↓PVR Diuretics Thiazides act at distal convoluted tubule Loop Diuretics act at ascending Loop of Henle Potassium Sparing Diuretics act in distal tubule to block aldosterone effects Diuretics Side Effects Thiazides Hypokalemia Hyperuricemia Hyperglycemia Hyperlipidemia Loop Diuretics Hypokalemia Hypocalcemia Aldosterone Inhibitors Gynecomastia Menstrual irregularity Diuretics Indications Often used in combination with other agents Hypertension resulting from fluid overload Patients on steroid therapy Glomerulonephritis Caution/Contraindications Thiazides contraindicated with GFR < 30 Monitor potassium- may be low with Thiazides and Loops. May be elevated with Potassium sparing. Athletes Central α2-Agonist (Clonidine) Mechanism of Action Block sympathetic outflow of norepinephrine through stimulation of α-2 receptors in brain resulting in sympathetic tone reduction Effect on Blood Pressure Decrease Heart Rate and Contractility Decrease Renin Release ↓CO ↓PVR Commonly used for attention deficit/hyperactivity disorder Central α2-Agonist (Clonidine) Side Effects Lethargy Rebound Hypertension Formulations Tablets Compounded suspension Transdermal Patches Indications for Medication Prehypertension 90-95TH Percentile for height and age Institute life style changes NO medications unless compelling indications such as CKD, Diabetes, Heart Failure, or Left Ventricular Hypertrophy Recheck in 6 months Indications for Medication Stage 1 Hypertension 95th-99th Percentile plus 5 mmHg for height and age Lifestyle changes Recheck in 1-2 weeks or sooner if symptomatic Initiate therapy based on clinical or compelling indications Indications for Medication Stage 2 >99th percentile plus 5 mmHg for age and height Lifestyle changes See within a week, or refer Initiate stepwise therapy What Agent to Use? Is there an identifiable cause for hypertension? If no identifiable cause are there other co-morbidities that may be improved or worsened by the drug choice prescribed? First line agents for consideration according to Fourth Report - CCB, ACE inhibitor, diuretics Treatment Adherence Lifestyle Changes Medication Adherence Assessment/Improvement Parental/Patient Education Medication Calendars Pill Boxes Blood pressure logs Reminder Apps on Phone Simplify Medication Regimen References Feld LG, Corey H. Hypertension in childhood. Pediatr Rev 2007;28;283-298. The Fourth Report on the Diagnosis, Evaluation,andTreatment of High Blood Pressure in Children and Adolescents. Pediatrics 2004;14:555-576. Lande M,Flynn J. Treatment of hypertension in children and adolescents. Pediatr Nephrol 2009; 24:1939-1949. • Lurbe E, Cifkova R,Cruickshank JK, et al. Management of high blood pressure in children and adolescents:recommendations of the European Society of Hypertension. J Hypertens 2009; 27:1719-1742. • Hadtstein C,Schafer F. Hypertension in children with chronic kidney disease:pathophysiology and management. Pediatr Nephrol. 2008; 23:363-371. • James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guidelines for the management of high blood pressure in adults. Report from the panel members appointed too the Eighth Joint National Committee. JAMA. 2013 published online December 18,2013.