* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Digestive System Day 2
Survey
Document related concepts
Transcript
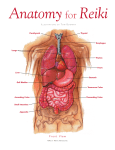
NOTES – DIGESTIVE SYSTEM ANATOMY Interesting Digestive System Facts After you eat how long does it take for the stomach to empty? Within 2-6 hours, all food is emptied into the small intestine. How many pounds of food does the average person eat in a year? 1,100 How many feet long are your intestines? about 20-30 ft long. NOTES – DIGESTIVE SYSTEM ANATOMY • Oral Cavity • mouth, pharynx, esophagus • MOUTH • SALIVARY GLANDS – produce saliva • Saliva Components • Mostly water – about 99.5% • SALIVARY AMYLASE – digests starch • LYSOZYME – antibacterial action • MUCIN – lubricant • chewing and saliva with food form a BOLUS • PHARYNX • common area for food and air • Epiglottis • prevents food from entering the trachea (wind pipe) • ESOPHAGUS • transports bolus from pharynx to stomach Pierces diaphragm and joins stomach at cardiac sphincter • involuntary muscular movement of food - PERISTALSIS Homeostatic Imbalance • Heartburn – Stomach acid regurgitates into esophagus – Likely with excess food/drink, extreme obesity, pregnancy, running – Also with hiatal hernia - structural abnormality • Part of stomach above diaphragm • Can esophagitis, esophageal ulcers, esophageal cancer © 2013 Pearson Education, Inc. Esophagus • Esophageal mucosa contains stratified squamous epithelium – Changes to simple columnar at stomach • Esophageal glands in submucosa secrete mucus to aid in bolus movement © 2013 Pearson Education, Inc. Figure 23.12a Microscopic structure of the esophagus. Mucosa (stratified squamous epithelium) Submucosa (areolar connective tissue) Lumen Muscularis externa • Circular layer • Longitudinal layer Adventitia (fibrous connective tissue) © 2013 Pearson Education, Inc. Figure 23.12b Microscopic structure of the esophagus. Mucosa (stratified squamous epithelium) © 2013 Pearson Education, Inc. Esophagus-stomach junction Simple columnar epithelium of stomach • STOMACH • a storage & mixing chamber • secretions • mucus • hydrochloric acid (HCl) • HCl activates pepsinogen to pepsin which is main enzyme that digests protein Figure 23.14a Anatomy of the stomach. Cardia Fundus Esophagus Muscularis externa • Longitudinal layer • Circular layer • Oblique layer Serosa Body Lumen Lesser curvature Rugae of mucosa Greater curvature Duodenum © 2013 Pearson Education, Inc. Pyloric sphincter (valve) at pylorus Pyloric canal Pyloric antrum Figure 23.14b Anatomy of the stomach. Liver (cut) Fundus Body Spleen Lesser curvature Greater curvature © 2013 Pearson Education, Inc. Stomach: Microscopic Anatomy • Mucosa – Simple columnar epithelium composed of mucous cells • Secrete two-layer coat of alkaline mucus – Surface layer traps bicarbonate-rich fluid beneath it – Dotted with gastric pits gastric glands • Gastric glands produce gastric juice © 2013 Pearson Education, Inc. Figure 23.15b Microscopic anatomy of the stomach. Gastric pits Surface epithelium (mucous cells) Gastric pit Mucous neck cells Parietal cell Gastric gland Chief cell Enteroendocrine cell © 2013 Pearson Education, Inc. Enlarged view of gastric pits and gastric glands Figure 23.30b Mesenteries of the abdominal digestive organs. Liver Gallbladder Lesser omentum Stomach Duodenum Transverse colon Small intestine Cecum Urinary bladder © 2013 Pearson Education, Inc. Homeostatic Imbalance • Gastritis – Inflammation caused by anything that breaches mucosal barrier • Peptic or gastric ulcers – Erosions of stomach wall • Can perforate peritonitis; hemorrhage – Most caused by Helicobacter pylori bacteria – Some by NSAIDs © 2013 Pearson Education, Inc. Figure 23.16 Photographs of a gastric ulcer and the H. pylori bacteria that most commonly cause it. Bacteria Mucosa layer of stomach A gastric ulcer lesion © 2013 Pearson Education, Inc. H. pylori bacteria Homeostatic Imbalance • Vomiting (emesis) caused by • Extreme stretching • Intestinal irritants, e.g., bacterial toxins, excessive alcohol, spicy food, certain drugs • Chemicals/sensory impulses emetic center of medulla • Excessive vomiting dehydration, electrolyte and acid-base imbalances (alkalosis) © 2013 Pearson Education, Inc. • movement • mixing waves - peristalsis • bolus becomes chyme • SMALL INTESTINE • parts: duodenum, jejunum, ileum • Function: • digestion and absorption • intestinal juice – water & mucus • epithelial cells have digestive enzymes to digest ALL classes of food Duodenum • Curves around head of pancreas; shortest part – 25 cm • Bile duct (from liver) and main pancreatic duct (from pancreas) – Join at hepatopancreatic ampulla – Enter duodenum at major duodenal papilla – Entry controlled by hepatopancreatic sphincter © 2013 Pearson Education, Inc. Figure 23.21 The duodenum of the small intestine, and related organs. Right and left hepatic ducts of liver Cystic duct Common hepatic duct Bile duct and sphincter Accessory pancreatic duct Mucosa with folds Tail of pancreas Pancreas Jejunum Gallbladder Major duodenal papilla Hepatopancreatic ampulla and sphincter © 2013 Pearson Education, Inc. Main pancreatic duct and sphincter Duodenum Head of pancreas Jejunum and Ileum • Jejunum – Extends from duodenum to ileum – About 2.5 m long • Ileum – Joins large intestine at ileocecal valve – About 3.6 m long © 2013 Pearson Education, Inc. Figure 23.30c Mesenteries of the abdominal digestive organs. Greater omentum Transverse colon Transverse mesocolon Descending colon Jejunum Mesentery Sigmoid mesocolon Sigmoid colon Ileum © 2013 Pearson Education, Inc. Structural Modifications • Increase surface area of proximal part for nutrient absorption – Circular folds (plicae circulares) – Villi – Microvilli © 2013 Pearson Education, Inc. Structural Modifications • Circular folds – Permanent folds (~1 cm deep) that force chyme to slowly spiral through lumen more nutrient absorption • Villi – Extensions (~1 mm high) of mucosa with capillary bed and lacteal for absorption • Microvilli (brush border) – contain enzymes for carbohydrate and protein digestion © 2013 Pearson Education, Inc. Figure 23.22a Structural modifications of the small intestine that increase its surface area for digestion and absorption. Vein carrying blood to hepatic portal vessel Muscle layers Circular folds Villi © 2013 Pearson Education, Inc. Lumen Figure 23.22b Structural modifications of the small intestine that increase its surface area for digestion and absorption. Microvilli (brush border) Absorptive cells Lacteal Goblet cell Blood capillaries Mucosaassociated lymphoid tissue Intestinal crypt Muscularis mucosae Duodenal gland © 2013 Pearson Education, Inc. Villus Enteroendocrine cells Venule Lymphatic vessel Submucosa Figure 23.22c Structural modifications of the small intestine that increase its surface area for digestion and absorption. Absorptive cells Goblet cells Villi © 2013 Pearson Education, Inc. Intestinal crypt Figure 23.23 Microvilli of the small intestine. Mucus granules Microvilli forming the brush border Absorptive cell © 2013 Pearson Education, Inc. Homeostatic Imbalance • Chemotherapy targets rapidly dividing cells – Kills cancer cells – Kills rapidly dividing GI tract epithelium nausea, vomiting, diarrhea © 2013 Pearson Education, Inc. • LIVER • performs many functions – main blood filter in digestive system • in digestion it secretes BILE into the gall bladder • the gall bladder then dumps bile into small intestine Figure 23.24a Gross anatomy of the human liver. Sternum Nipple Bare area Liver Falciform ligament Left lobe of liver Right lobe of liver Gallbladder © 2013 Pearson Education, Inc. Round ligament (ligamentum teres) Figure 23.24b Gross anatomy of the human liver. Lesser omentum (in fissure) Left lobe of liver Porta hepatis containing hepatic artery (left) and hepatic portal vein (right) Quadrate lobe of liver Ligamentum teres Bare area Caudate lobe of liver Sulcus for inferior vena cava Hepatic vein (cut) Bile duct (cut) Right lobe of liver Gallbladder © 2013 Pearson Education, Inc. Figure 23.21 The duodenum of the small intestine, and related organs. Right and left hepatic ducts of liver Cystic duct Common hepatic duct Bile duct and sphincter Accessory pancreatic duct Mucosa with folds Tail of pancreas Pancreas Jejunum Gallbladder Major duodenal papilla Hepatopancreatic ampulla and sphincter © 2013 Pearson Education, Inc. Main pancreatic duct and sphincter Duodenum Head of pancreas Figure 23.25a–b Microscopic anatomy of the liver. Lobule © 2013 Pearson Education, Inc. Central Connective vein tissue septum Liver: Microscopic Anatomy • Hepatocytes – increased rough & smooth ER, Golgi, peroxisomes, mitochondria • Hepatocyte functions – Process bloodborne nutrients – Store fat-soluble vitamins – Perform detoxification – Produce ~900 ml bile per day © 2013 Pearson Education, Inc. Liver • Regenerative capacity – Restores full size in 6-12 months after 80% removal – Injury hepatocytes growth factors endothelial cell proliferation © 2013 Pearson Education, Inc. Homeostatic Imbalance • Hepatitis – Usually viral infection, drug toxicity, wild mushroom poisoning • Cirrhosis – Progressive, chronic inflammation from chronic hepatitis or alcoholism – Liver fatty, fibrous portal hypertension • Liver transplants successful, but livers scarce © 2013 Pearson Education, Inc. • bile EMULSIFIES fats – breaks fat into smaller pieces – easier for fat digesting enzymes to do their work Normal liver fatty liver Cirrhosis of the liver • PANCREAS • pancreatic enzymes are important for the digestion of all major classes of food • four enzymes and bicarbonate • all are dumped into small intestine Figure 23.26a Structure of the enzyme-producing tissue of the pancreas. Small duct Acinar cell Basement membrane Zymogen granules Rough endoplasmic reticulum Duct cell One acinus © 2013 Pearson Education, Inc. Figure 23.26b Structure of the enzyme-producing tissue of the pancreas. Acinar cells Pancreatic duct © 2013 Pearson Education, Inc. • LARGE INTESTINE • Parts: ascending colon, transverse colon, descending colon, sigmoid colon • chyme is converted to feces • absorption of water & salts • E. coli bacteria synthesizes vitamin K Figure 23.29a Gross anatomy of the large intestine. Left colic (splenic) flexure Right colic (hepatic) flexure Transverse mesocolon Transverse colon Epiploic appendages Superior mesenteric artery Descending colon Haustrum Ascending colon IIeum Cut edge of mesentery IIeocecal valve Tenia coli Sigmoid colon Cecum Appendix Rectum Anal canal © 2013 Pearson Education, Inc. External anal sphincter Figure 23.30d Mesenteries of the abdominal digestive organs. Liver Lesser omentum Pancreas Stomach Duodenum Transverse mesocolon Transverse colon Mesentery Greater omentum Jejunum Ileum Visceral peritoneum Parietal peritoneum Urinary bladder Rectum © 2013 Pearson Education, Inc. Homeostatic Imbalance • Low fiber diet narrowed colon strong contractions increased pressure on walls diverticula (herniations of mucosa) • Diverticulosis commonly in sigmoid colon – Affects ½ people > 70 years • Diverticulitis – Inflamed diverticula; may rupture and leak into peritoneal cavity; may be life threatening © 2013 Pearson Education, Inc. Homeostatic Imbalance • Irritable bowel syndrome – Functional GI disorder – Recurring abdominal pain, stool changes, bloating, flatulence, nausea, depression – Stress common precipitating factor • Stress management important in treatment © 2013 Pearson Education, Inc. Malabsorption of Nutrients • Gluten-sensitive enteropathy (celiac disease) – Immune reaction to gluten – Gluten causes immune cell damage to intestinal villi and brush border – Treated by eliminating gluten from diet (all grains but rice and corn) © 2013 Pearson Education, Inc. Developmental Aspects • Oral membrane mouth opening • Cloacal membrane anus • By week 5 alimentary canal continuous tube from mouth to anus • Shortly after, accessory organs bud from mucosa © 2013 Pearson Education, Inc. Figure 23.36 Embryonic development of the digestive system. Lung bud Brain Oral membrane Heart Yolk sac Stomodeum Foregut Liver Site of liver development Body stalk Gallbladder Hindgut Cystic duct Ventral pancreatic bud Proctodeum Endoderm © 2013 Pearson Education, Inc. Bile duct Midgut Spinal cord Cloacal membrane Stomach Dorsal pancreatic bud Duodenum Homeostatic Imbalance • Cleft palate and cleft lip • Tracheoesophageal fistula – Opening between esophagus and trachea • Cystic fibrosis – Genetic disease thick mucus can block pancreatic duct © 2013 Pearson Education, Inc. Developmental Aspects • Fetal nutrition via placenta, but GI tract stimulated to mature by amniotic fluid swallowed in utero • Newborn's rooting reflex helps infant find nipple; sucking reflex aids in swallowing • Newborns double birth weight in six months; adult diet by 2 years • Cholecystitis, ulcers – problems of middle age © 2013 Pearson Education, Inc. Developmental Aspects • During old age – GI tract activity declines, less digestive juice, absorption less efficient, peristalsis slows less frequent bowel movements – Taste/smell less acute; periodontal disease often develops – Diverticulosis, fecal incontinence, and cancer of GI tract fairly common © 2013 Pearson Education, Inc. Cancer • Stomach and colon cancers rarely have early signs or symptoms • Metastasized colon cancers frequently cause secondary liver cancer • Prevention – Regular dental and medical examination © 2013 Pearson Education, Inc.