* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Acute Care Problems Case Studies 1 and 2
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Cardiac surgery wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
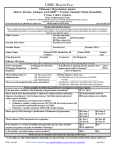
Running head: CASE STUDIES 1 AND 2 Acute Care Problems Case Studies 1 and 2 Laura J Langenhop Wright State University 1 CASE STUDIES 1 AND 2 2 Acute Care Problems Case Studies 1 and 2 Question 1: What is the most likely diagnosis for this patient and what are the criteria for the diagnosis? The patient’s symptoms, medications, social history, and physical examination lead to the differential diagnoses of pulmonary arterial hypertension, pulmonary embolism, right-sided heart failure, insufficiency of the tricuspid valve, and pneumonia (Moser & Reigel, 2008). The most likely diagnosis for this patient is pulmonary arterial hypertension associated with the use of Fenfluramine and Phentermine (Moser & Riegel, 2008). The symptoms of pulmonary arterial hypertension are the decrease in exercise activity, fatigue, syncope, and chest discomfort (Moser & Reigel, 2008; Barst et al., 2004). On physical examination, a-waves are present with jugular venous distension that can be interpreted as right ventricular involvement and increased fluid volume (Longo et al., 2012). A second pulmonic sound is heard on auscultation, a heave is noted on the left sternal border with an S3 gallop revealing tricuspid valve regurgitation, the patient has pedal edema, hepatomegaly, and ascites (Moser & Reigel, 2008). The subjective and objective data the patient presents are common in patients with pulmonary hypertension. In patients with pulmonary arterial hypertension, 87 percent have right ventricular hypertrophy and 79 percent have right axis deviation on their electrocardiograms (Moser & Reigel, 2008). The electrocardiogram has a sensitivity of 55 percent and a specificity of 70 percent when screening for pulmonary arterial hypertension (Barst et al., 2004). The patient has right axis deviation, right atrial enlargement, prominent RSR prime in leads V1 through V6 with ST-segment depression, and T wave inversion. Patients with RSR prime in lead V1 indicate to the advanced practice registered nurse (APRN) pulmonary involvement as well as possible CASE STUDIES 1 AND 2 3 conduction abnormalities caused by an obstruction from the right ventricular outflow tract (Grauer, 1998). The electrocardiogram findings are all common in patients with pulmonary arterial hypertension (Moser & Reigel, 2008). The chest radiograph of the patient reveals cardiomegaly, clear lungs fields, and an enlarged pulmonary trunk. The patient’s cardiomegaly is due to the heart’s ability to remodel and adjust to increased pulmonary pressures (Longo et al., 2012). When the right ventricle myocardium becomes ischemic due to excessive demands, failure occurs (Longo et al, 2012). Since the lungs fields are clear with no evidence of hyperinflation or pleural effusions, the patient can be excluded from pulmonary venous hypertension involving left sided heart failure and from an obstructive lung disease as the cause of the patient’s pulmonary hypertension (Barst et al., 2004). There has been suspicion that Fenfluramine and other anorexigens increase 5-HT and block the reuptake of serotonin in the blood leading to increased pulmonary blood flow and increased arterial growth of the pulmonary smooth muscle (Rothman, Ayestas, Dersch, & Baumann, 1999). Exposure to Fenfluramine for at least three months has shown to increase the incidence of idiopathic pulmonary arterial hypertension (McLaughlin et al., 2009). The patient has been exposed to Fenfluramine and Phentermine for the past two years creating a high risk for pulmonary hypertension. The patient is a cigarette smoker as well, causing further vasoconstriction of the pulmonary vasculature (Longo et al., 2012). The classification of pulmonary hypertension is based on the New York Heart Association’s (NYHA) functional status of patients with pulmonary hypertension (Moser & Reigel, 2008). The patient would be placed in the NYHA functional class IV (Moser & Reigel, 2008). NYHA class IV is defined as patients with pulmonary hypertension who are unable to CASE STUDIES 1 AND 2 4 perform any physical activity without exhibiting symptoms of dyspnea and fatigue as well as the display of signs and symptoms of right ventricular failure even at rest (Moser & Reigel, 2008). Of the five categories of pulmonary hypertension, the patient will most likely be classified as being in category one. Category one is defined as patients having pulmonary arterial hypertension or having an elevated pulmonary arterial pressure (PAP) with a normal pulmonary capillary wedge pressure (PCWP) (Rich, 2012). More specifically, the patient is placed in the category with the cause being exposure to toxins and drugs (Rich 2012). Question 2: What diagnostic test should be performed? Explain your rationale. Initially, a transthoracic echocardiogram is completed when there is suspicion of pulmonary hypertension. The echocardiogram will estimate pulmonary arterial systolic pressure, size of atria and ventricles, valve functionality, estimated pulmonary vascular resistance, and intra-cardiac or intrapulmonary shunts (Barst et al., 2004). Pulmonary hypertension is suspected through an echocardiogram when the patient’s pulmonary artery systolic pressure is greater than 35 mm Hg or the mean is greater than 25 mm Hg at rest or greater than 30 mm Hg with exercise (Barst et al., 2004). The most confirmatory test that can be done to diagnose pulmonary arterial hypertension is a right heart catheterization with a vasodilator challenge (Barst et al., 2004). Diagnosis of pulmonary arterial hypertension from a right heart catheterization is confirmed when the patient’s mean pulmonary artery pressure (PAP) is greater than 25 mmHg at rest, the pulmonary capillary wedge pressure (PCWP) is less than or equal to 15 mmHg, and the pulmonary vascular resistance (PVR) is greater than three wood units (Barst et al., 2004). If the PCWP is elevated above 15 mmHg, the presence of left ventricular heart disease or pulmonary venous obstruction should be investigated (Barst et al., 2004). Portal hypertension can also be detected by an CASE STUDIES 1 AND 2 5 increased gradient between free and occluded hepatic venous pressures at the time of the right heart catheterization (Galie et al., 2009). A vasodilator challenge should be completed during the right heart catheterization in patients being considered for calcium channel blocker therapy (Barst et al., 2004). Examples of acute vasodilator challenge medications are inhaled nitric oxide, intravenous Epoprostenol, intravenous Adenosine, or inhaled Iloprost (Barst et al., 2004). An acute response to vasodilator therapy is defined as a reduction in the mean pulmonary artery pressure by 10 mmHg for a total mean pulmonary artery pressure of 40 mmHg or less without a decrease in cardiac output (McLaughlin et al., 2009). A ventilation-perfusion (VQ) scan is essential to rule out an embolus causing the patient’s pulmonary hypertension (Galie et al., 2009). This specific patient is a smoker and is on contraceptives making her at risk for thromboembolic events. A VQ scan has a sensitivity of 90 percent to 100 percent and a specificity of 94 percent to 100 percent in deciphering between chronic thromboembolic pulmonary hypertension and idiopathic pulmonary hypertension (Barst et al., 2004). If a pulmonary embolus is suspected, a computerized tomography scan of the chest may also be completed to further evaluate the evidence of pulmonary embolus or lung parenchymal disease (Galie et al., 2009). Laboratory values may be drawn to aid in determining the cause of the pulmonary hypertension as well as to view the affects the patient’s pulmonary hypertension has on the body and surrounding organ systems. An anti-nuclear antibody (ANA) titer will be collected to rule out a connective tissue disorder as the cause of the patient’s pulmonary hypertension (Barst et al., 2004). If the ANA levels are substantially high, a rheumatoid consultation may be warranted (Barst et al., 2004; McLaughlin, 2009). Serological testing to view connective tissue diseases, CASE STUDIES 1 AND 2 6 human immunodeficiency virus (HIV), and hepatitis as potential causes may be completed after further questioning of risk factors (Galie et al., 2009). A complete blood cell count, liver function tests, thyroid function tests, and anti-phospholipid antibodies such as a lupus anticoagulant are also recommended (Barst et al., 2004; Galie et al., 2009). A brain natriuretic peptide (BNP) level is drawn to evaluate right and left ventricle wall stress (Barst et al., 2004; Galie et al., 2009). A uric acid level is drawn as a marker for ineffective oxidative metabolism of ischemic peripheral tissue. Troponin levels are drawn to screen for coronary artery disease, pulmonary embolus, and cardiac damage (Galie et al., 2009). Finally, a six-minute walk test is completed to assess functional class (McLaughlin et al., 2009). Though this is not a diagnostic tool, the walk test is helpful in determining the severity of the disease and exercise capacity. The six-minute walk test will be completed initially at time of suspected diagnosis and after initiation of treatment is ordered to assess progress (Moser & Reigel, 2008; McLaughlin et al., 2009). Question 3: What is the appropriate therapy for this patient? Include all types of therapy and rationale for your choices. The overall goals of therapy are to increase quality of life, decrease symptoms, and increase functionality (McLaughlin et al., 2009). In patients with a favorable vasodilator affect during their right heart catheterizations, calcium channel blocker therapy should be initiated first (McLaughlin et al., 2009). Long acting calcium channel blockers such as Cardizem, Nifedipine, or Amlodipine are recommended (McLaughlin et al., 2009). If the patient does not progress to functional class one or two on calcium channel blocker therapy, the patient is then considered a chronic responder and alternative therapy should be initiated (Barst et al., 2004). In patients who do not respond to the vasodilator challenge during the right heart catheterization or do not CASE STUDIES 1 AND 2 7 progress with the use of calcium channel blocker therapy, oral medications such as Sildenafil and Bosentan or intravenous medications such as Epoprostenol or Treprostinil therapy may be initiated (McLaughlin et al., 2009). Prostacyclins such as Iloprost, Epoprostenol, and Treprostinil are used in the treatment for pulmonary hypertension. Iloprost, an inhaled medication, is a prostacyclin analogue. Iloprost has been shown to improve symptoms and increase exercise tolerance (Rich, 2012). Epoprostenol, an intravenous medication, has shown to increase survival in patients who fail conventional therapy (McLaughlin et al., 2009). Epoprostenol has a short half-life and requires permanent intravenous access for administration (Rich, 2012). Epoprostenol has been studied in patients with functional class three and four (McLaughlin et al., 2009). Treprostinil may be given intravenously or subcutaneously at a continuous rate (Rich, 2012). Like Epoprostenol, Treprostinil has shown to increase exercise tolerance and decrease symptoms (McLaughlin et al., 2009). Prostacyclins have benefits of vasodilation, platelet inhibition, and hampers growth of vascular smooth muscle (Rich, 2012). Endothelin receptor antagonists, such as Bosentean and Ambristenan, block endothelin-1 causing vasodilation of the smooth muscle (McLaughlin et al., 2009). Bosentan has been shown to increase patients’ six-minute walk tests, decrease pulmonary vascular resistance, and decrease mean pulmonary arterial pressure (McGlaughlin et al., 2009). Liver function testing should be completed routinely and a complete blood cell count should be obtained after three months of treatment (McLaughlin et al., 2009). Ambrisentan has also been shown to increase patients’ sixminute walk test times. Liver injury and teratogenicity have been reported when using Ambrisentan (McLaughlin et al., 2009). Monthly pregnancy testing should be completed as when on Ambrisentan (McLaughlin et al., 2009). CASE STUDIES 1 AND 2 8 Phosphodiesterase inhibitors such as Sildenafil and Tadalafil are used to increase the effects of cyclic guanylate cyclase and therefore aid in relaxation and vasodilation of the vessels (McLaughlin et al., 2009). Sildenafil is a phosphodiesterase-5 inhibitor (Lexicomp, 2014). Sildenafil has shown to increase patients’ six-minute walk tests and increase functional status in patients with idiopathic pulmonary hypertension and pulmonary hypertension related to a connective tissue disease (McLaughlin et al., 2009). Combination therapy with Sildenafil and other agents has also been studied and has shown to have benefits on quality of life, mean pulmonary arterial pressure, and patients’ six-minute walk tests (McLaughlin et al., 2009). The patient’s right atrial and ventricular enlargement, the patient may eventually be a candidate for Digoxin therapy (McLaughlin et al., 2009). Right atrial enlargement puts the patient at risk for arrhythmias (Moser & Riegel. 2008). Digoxin has shown to increase cardiac contractility as a positive inotropic agent as well as increasing cardiac output and cardiac index (McLaughlin et al., 2009). The patient may also be in need of diuretic therapy. As right ventricular function worsens, volume overload as seen in the abdomen and lower extremities increases. Choice for diuretic therapy typically includes loop diuretics to help in decreasing right ventricular volume (McLaughlin et al., 2009). Renal function, magnesium levels, and potassium levels should be monitored when the patient is on diuretic therapy (McLaughlin et al., 2009; Lexicomp, 2014). Recommendations from the American College of Cardiology for anticoagulation therapy in patients with idiopathic pulmonary arterial hypertension recommend warfarin therapy to maintain an international normalized ratio of 1.5 to 2.5 seconds (McLaughlin et al., 2009). Anticoagulation therapy has also shown to be favorable in patients with diet and drug induced CASE STUDIES 1 AND 2 9 pulmonary arterial hypertension (McLaughlin et al., 2009). Oxygen therapy is recommended to keep oxygen saturation levels greater than 90 percent (McLaughlin et al., 2009). According to the Ohio Formulary, the APRN may prescribe calcium channel blockers, Digoxin, and diuretics (Ohio Board of Nursing, 2014). The APRN may prescribe anticoagulation, endothelin receptor analogues, prostacylcins, and phophodiesterase inhibitors if these medications are within the APRN’s standard care arrangement (Ohio Board of Nursing, 2014). Low-grade exercise is recommended as it has shown to improve six-minute walk test results, functional class, and peak oxygen consumption (Barst et al., 2004; McLaughlin et al., 2004). A low sodium diet is advised to help reduce fluid retention with patients in right-sided heart failure (Barst et al., 2004). Education would also be given to the patient regarding the pneumonia and influenza vaccines and the importance of receiving such vaccines (McLaughlin et al., 2009). In viewing long term, surgical interventions that may be performed to help symptom relief and improve quality of life in patients with pulmonary hypertension include an atrial septostomy, heart and lung transplantation, pulmonary thromboendarterectomy, and use of a right ventricular assist device (McLaughlin et al., 2009). An atrial septostomy creates a right to left shunt between atria. By creating a shunt, the right sided pressures of the heart decrease and cardiac output increases because of the increased volume seen on the left side of the heart as a result of the shunt (McLaughlin et al., 2009). An atrial septostomy is recommended in patients with intractable right heart failure even after maximal medical efforts (McLaughlin et al., 2009). Lung and heart transplantation may be considered in end-stage pulmonary hypertension patients (McLaughlin et al., 2009). The choice to transplant both the heart and the lungs depends CASE STUDIES 1 AND 2 10 upon the patient’s cardiac function. Heart and lung transplantation is typically offered to patients in intractable right heart failure who are dependent on inotropic therapy. Once a patient is considered for and is agreeable to heart and lung transplantation, consistent follow-up is recommended with the goal to stabilize and maintain cardiac function (McLaughlin et al., 2009). Patients who are diagnosed with chronic thromboembolic pulmonary hypertension may have a thromboendarterectomy completed in order to remove material from the pulmonary vasculature and decrease pulmonary vascular resistance (McLaughlin et al., 2009). Patients who have pulmonary hypertension and who are also in right ventricular failure have recently had the option to receive a right ventricular assist device (RVAD). Though there seems to be usefulness for the RVAD in patients with pulmonary hypertension, recommendation for further research has continued to test for the effectiveness of the device in this patient population (McLaughlin et al., 2009). CASE STUDIES 1 AND 2 11 Case Study 2 1. What is your differential diagnosis? Explain. The patient’s differential diagnoses are pre-renal failure, acute tubular necrosis, interstitial nephritis, contrast-induced nephropathy, or post-renal failure (Kemp, Burns, & Brown, 2008). Acute kidney injury is defined as a serum creatinine that has increased by one to two-fold from baseline, a urine output of 0.5 ml/kg/hr for greater than six hours, or a presumed decrease in urine output within one week (The Renal Association, 2011). This specific patient is at risk for acute kidney injury because of the patient’s history of heart disease, atherosclerotic disease, diabetes, and use of a nephrotoxic agent (The Renal Association, 2011). Oliguria reported at less than 400 mL in 24 hours reflects a more significant acute kidney injury (Li & Vijaylan, 2012). In contrast, complete oliguria usually is reflective in urinary obstruction, septic shock, ischemia, and renal artery occlusion (Li & Vijaylan, 2012). Based on the patient’s symptoms and use of intravenous contrast, the diagnosis of post-renal failure is unlikely. The patient’s symptoms and clinical picture are more indicative to pre-renal failure of contrast-induced nephropathy (Li & Vijaylan, 2012). The most common cause for acute kidney injury is pre-renal azotemia (Waikar & Bonventre, 2012). Reasons for pre-renal acute kidney injury are low cardiac output, hypovolemia, and use of medications that stand in the way of renal autoregulatory responses (Waiker & Bonventre, 2012). The patient was placed on a nephrotoxic drug, Lisinopril, causing decreased glomerular filtration by increasing vasodilation in the afferent arteriole and decreasing vasoconstriction in the efferent arteriole (The Renal Association, 2011; Waiker & Bonventre, 2012). The patient was also placed on Nitroglycerin, a venodilator, adding to further vasodilation (Longo et al., 2012). The patient has a history of hypertension with dot hemorrhages CASE STUDIES 1 AND 2 12 on his fundus, revealing breakdown of the vascular wall (Walsh, O’Rourke, & Shaver, 2011). The patient may be so used to a higher blood pressure that the ACE-inhibitor and Nitroglycerin administered together decreased the patient’s renal perfusion therefore causing pre-renal failure (Waiker & Bonventre, 2012). Acute interstitial nephritis (AIN) is usually related to a hypersensitivity reaction to medications such as antimicrobials and anticonvulsants (Marino, 2014). Oliguria is typically not seen and the injury with symptoms occurs one to two weeks after exposure to agents (Marino, 2014). The onset of this patient’s symptoms rules out interstitial nephritis. Acute tubular necrosis (ATN) results from an increased pre-renal state as a result from hypovolemia, ischemia, sepsis, and administration of toxins (Li & Vijaylan, 2012). Endothelial damage occurs resulting in vasoconstriction, increased permeability, and increased interstitial pressure, ultimately leading to decreased capillary blood flow (Yaqub & Molitoris, 2009). Common causes of acute tubular necrosis are ischemia, rhabdomyolysis, hemoglobinuria, and cast nephropathy (Li & Vijaylan, 2012). The most common cause for the patient’s acute kidney injury is contrast-induced nephropathy (CIN) from the intravenous contrast administered during the percutaneous coronary intervention (PCI). Serum creatinine increases within 24-48 hours of contrast administration (Waiker & Bonventre, 2012). Patients are more at risk for CIN with the presence of pre-existing renal insufficiency, heart failure, and diabetic nephropathy (Waikar & Bonventre, 2012). The patient already had a baseline creatinine of 1.6 mg/dL and dot hemorrhages from hypertension and/or diabetes (Walsh et al., 2011). The patient has an S4 gallop from his myocardial infarction, which can also be an indicator of left ventricular dysfunction leading to an increased CASE STUDIES 1 AND 2 13 risk for CIN (Longo et al., 2012). Further diagnostic work ups such as urinalysis and urine electrolytes will need to be completed in order to make an accurate diagnosis. 2. What is your next step to diagnose the problem? Explain. Of what value is urinalysis and urinary electrolytes? The next step to diagnose this specific patient is to obtain a urinalysis and urine electrolytes testing in order to determine a specific diagnosis. A urinalysis is useful in determining the cause of the kidney injury. A urinalysis tests the color, pH, specificity, and sediment of the urine (Huether, 2010). From the urinalysis, intrinsic ATN would reveal granular casts, glomerular disease would reveal red blood cells casts, and interstitial nephritis would reveal white blood cell casts and urine eosinophilia (Li & Vijaylan, 2012). Glomerular disease can be suspected as a result of a three to four + protein with red blood cells (The Renal Association, 2011). An elevated white blood cell count on a urinalysis is typically seen with infection, interstitial nephritis, and glomerular nephritis (Lin & Denker, 2012). Acute kidney injury or ATN related to nephrotoxins, sepsis, or ischemia will have “muddy brown” casts and tubular epithelial casts. Pre-renal azotemia sediment is normal or has occasional hyaline and granular casts (Lin & Denker, 2012). Hematuria is common in patients with a urinary obstruction or post-renal failure. In the event that post-renal failure is highly suspected, certain testing should be completed. Bladder catheterization can quickly rule out urethral obstruction (Lin & Denker, 2012). A renal ultrasound may be performed in order to determine sources of obstruction unless another diagnosis has been made for the patient’s acute renal failure (Lin & Denker, 2012). If an CASE STUDIES 1 AND 2 14 obstruction is found, further treatment such as a dilatation is recommended (Lin & Denker, 2012). In patients suspected to have pre-renal failure, urine osmolality, urine/creatinine ratio, urine sodium, fractional excretion of sodium (FENa), fractional excretion of urea (FEurea), and urine specificity should be obtained (The Renal Association, 2011). The urine electrolytes also differentiate between the diagnosis of pre-renal failure or intrinsic renal failure (Li & Vijayan, 2012). In patients with pre-renal failure, sodium and urea reabsorption are increased due to hypovolemia or hypotension. The ureas and sodium reabsorption cause a decrease in FENa and FEurea and an increase in the blood urea/creatinine ratio (The Renal Association, 2011). Patients with acute tubular necrosis typically have increased FENa and FEurea levels (Lin & Denker, 2012). Medications such as diuretics can falsely skew the FENa as decreased because of the sodium-reducing characteristics of diuretics (The Renal Association, 2011). In patients with pre-renal failure, urine is concentrated, revealing an osmolality greater than 500 mOsm (Lin & Denker, 2012). Urine sodium is decreased to less than 20 mEq/L due to sodium reabsorption in the face of hypotension or decreased volume (Lin & Denker, 2012). Urine osmolality will be less than 350 mOsm and the urine sodium will be greater than 40 mEq/L in patients with ATN in comparison to patients with pre-renal failure (Lin & Denker, 2012). In patients with intrinsic renal failure, more specifically ATN, the kidneys lose their ability to reabsorb sodium and concentrate the urine (Li & Vijayan, 2012). In response to this, the patient’s FENa is >1% and the FEurea is >50% (Li & Vijayan, 2012). It is useful to note that patients with contrast induced nephropathy (CIN), though not a pre-renal kidney injury, will present with a decreased FENa. The contrast increases endothelin in the renal vasculature CASE STUDIES 1 AND 2 15 causing increased renal vasoconstriction and increased sodium reabsorption (Li & Vijayan, 2012). 3. What are the indications for dialysis in AKI? Be specific. The indications for renal replacement therapy are volume overload, hyperkalemia, metabolic acidosis, uremia, and the need to remove toxins as a result of an ineffectiveness of current medical treatment (Marino, 2014). If treatment is not effective and the blood urea nitrogen (BUN) levels continue to rise or show no signs of improvement, dialysis is recommended (Lin & Denker, 2012). Worsening acidosis can occur as the kidneys lose their ability to absorb bicarbonate and excrete acids (Li & Vikayan, 2012). Patients with hyperkalemia are at risk for life threatening adverse cardiac arrhythmias (Longo et al., 2012). Pharmacologic measures such as intravenous calcium, insulin, sodium bicarbonate, and inhaled albuterol are administered to enhance intracellular shift of potassium. The pharmacological methods can be unpredictable and inefficient, while dialysis can be a much safer and a faster alternative (Li & Vijaylan, 2012). Patients with volume overload despite diuretic use and confirmed pulmonary edema with respiratory compromise are subject to initiating dialysis (Li & Vijaylan, 2012). Complications of uremia such as asterixis, pericardial rub, encephalopathy, or bleeding also indicate the need for dialysis (Lin & Denker, 2012). Uremic patients’ findings do not always correlate with the BUN levels (Li & Vijaylan, 2012). In patients with uremia, clinical findings and symptoms decide the start of dialysis (Li & Vijaylan, 2012). 4. Write a set of admitting orders for the patient. Be specific. Admission: o Admit to the coronary care unit CASE STUDIES 1 AND 2 o Consult Nephrology Diagnosis: o Acute Myocardial infarction status post PCI o Contrast Induced Nephropathy o Secondary Diagnosis: Type 2 Diabetes, CAD Condition: o Serious Allergies: o No known drug allergies Vital Signs: o Blood pressure, pulse, and respirations q4 hour o Temperature q4 hours Notify the APRN if: o BP <90/50 or >160/90 o Pulse <50 or >120 o Respirations <10 or >26 o Temperature <96.0 F or >101.5 F o SpO2 <90% o Any sudden change in vital signs Activity: o Activity as tolerated o Out of bed three times per day o Ambulate in hallway with RN with continuous cardiac monitoring 16 CASE STUDIES 1 AND 2 Nursing: o Daily weights o Strict I and O o Call NP if urine output <30mL/hr o Insert foley catheter if patient unable to void o Incentive spirometry q2 hours o Measure blood sugar ACHS Diet: o 1800 No Concentrated Carbohydrates Low Fat, 2 gram Sodium diet o Protein Restriction 0.60 g/kg/day (Bargman & Skorecki, 2012) o 35 kcal/kg/day (Bargman & Skorecki, 2012) o Encourage fluids IV orders: o Maintain IV access on patient Medications: o 0.9% Normal Saline intravenous 100 mL/hr continuous o Nitroglycerin 25 mg/250 mL intravenous (10 mcg/min-100 mcg/min titrate) Titrate for chest pain and to keep blood pressure >90/60 or MAP > 65. o Aspirin 81 mg oral daily o Plavix 75 mg oral daily o Metoprolol 12.5 mg oral twice daily (hold for HR <55 bpm and BP <90/50) o Atorvastatin 40 mg oral nightly o Humalog Regular Insulin 0700, 1100, 1500, 2100 17 CASE STUDIES 1 AND 2 18 o Sliding Scale: o <70 mg/dL Hypoglycemia Protocol o 70mg/dL-125 mg/dL 0 units o 126 mg/dL-150 mg/dL 2 units o 151 mg/dL-200 mg/dL 4 units o 201 mg/dL-250 mg/dL 6 units o 251 mg/dL-300 mg/dL 8 units o 301 mg/dL-350 mg/dL 10 units o 351 mg/dL-400 mg/dL 12 units o >400 mg/dL 14 units and call NP o Normal saline 0.9% 10mL intravenous flush q8 hours o Docustae100 mg oral PRN one time daily o Acetaminophen 650 mg oral q4 hours PRN for moderate pain o Morphine 2-4 mg intravenous q2 hours for severe pain o Odansteron 4 mg intravenous q6 hours for nausea o 25 mL of D50 IV if patient blood sugar <70 mg/dL and unable to drink and re-check blood sugar 15 minutes after administration o 50 mL of D50 IV if patient blood sugar <50 mg/dL and unable to drink and re-check blood sugar 15 minutes after administration Laboratory: o CBC, now and then daily o EP1, now and Q12 hours o Cardiac profile q6 hours CASE STUDIES 1 AND 2 19 o Urinalysis x1 STAT o Urine electrolytes x1 STAT o Urine Microalbumin o HgAlc tomorrow am o EKG now x1 and then in the morning Special: o Consult Nephrology o Discontinue all nephrotoxic agents o Hypoglycemic Protocol: If patient blood sugar <70 mg/dL, give 15 grams of carbohydrates (glass of juice, crackers, or milk) and re-check blood sugar 30 minutes after administration. If blood sugar remains low, repeat snack and call NP o For any questions please call the CCU APRN phone at 513-666-3542 Thank you, Laura J Langenhop APRN 5. Complete the following chart with values present in pre-renal and acute renal failure. Be certain to reference chart. Laboratory Test Pre-renal Acute Renal Failure FeNa <1% >2% BUN to creatinine ratio >20:1 10-15:1 Urine specific gravity >1.020 1.010-1.020 Urine osmolality, mOm per Kg Urine Sodium concentration, mEq per L (mmol per L) Urine Sediment >500 mOsm/kg <350 mOsm/kg <20 mEq/L >40 mEq/L Usually no cells, some hyaline casts Brown granular cells, epithelial cells CASE STUDIES 1 AND 2 20 Table 1 Adapted from (Lin & Denker, 2012). Azotemia and urinary abnormalities. In Longo et al., Harrison’s Principles of Internal Medicine 18th edition. New York, NY: McGraw Hill. CASE STUDIES 1 AND 2 21 References Bargman, J. M., & Skorecki, K. (2012). Chronic kidney disease. In D. L. Longo, D. L. Kasper, J. L. Jameson, A. S. Fauci, S. L. Hauser, & J. Loscalzo (Eds.), Harrison’s principles of internal medicine (18th ed.). Retrieved from http://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx?bo okid=331§ionid=40727069&jumpsectionID=40754172&Resultclick=2 Barst, R. J., McGoon, M., Torbicki, A., Sitbon, O., Krowka, M. J., Olschewski, H., & Gaine, S. (2004). Diagnosis and differential assessment of pulmonary arterial hypertension. Journal of the American Academy of Cardiology, 43(12s1), S40-S47. http://dx.doi.org/10.1016/j.jacc.2004.02.032 Galie, N., Hoeper, M. M., Humbert, M., Torbicki, A., Vachiery, J., Barbera, J. A., ... Simonneau, G. (, ). . , (), . http://dx.doi.org/Retrieved from Galie, N., Hoeper, M. M., Humbert, M., Torbicki, A., Vachiery, J., & Barbera, J. A. (2009). Guidelines for the diagnosis and treatment of pulmonary hypertension. European Heart Jouranl, 30(20), 2493-2537. http://dx.doi.org/10.1093/eurheartj/ehp297 Grauer, K. (1998). A practical guide to ECG interpretation (2 ed.). St. Louis, MO: Mosby. Huether, S. E. (2010). Structure and function of the renal and urologic systems. In K. L. McCance, S. E. Huether, V. L. Brashers, & N. S. Rote (Eds.), Pathophysiology: The biologic basis for disease for disease in adults and children (6th ed., pp. 1344-1364). Maryland Heights, MO: Mosby Elsevier. Kemp, W. L., Burns, D. K., & Brown, T. G. (2008). Pathology: The big picture. Retrieved from http://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx?bo okid=499§ionid=41568299&jumpsectionID=41572000&Resultclick=2 CASE STUDIES 1 AND 2 22 Lexicomp. (2014). Retrieved from http://webstore.lexi.comPDA-software-for –nurses Li, T., & Vijayan, A. (2012). Acute kidney injury. In M. Kollef, & W. Isakow (Eds.), The washington manual of critical care (2nd ed., pp. 351-366). Philadelphia, PA: Lippincott Williams & Wilkins. Lin, J., & Denker, B. A. (2012). Azotemia and urinary abnormalities. In D. L. Longo, D. L. Kasper, J. L. Jameson, A. S. Fauci, S. L. Hauser, & J. Loscalzo (Eds.), Harrison’s principled of internal medicine (18th ed.). New York, NY: McGraw Hill. Longo, D. L., Fauci, A. S., Kasper, D. L., Hauser, S. L., Jameson, J. L., & Loscalzo, J. (2012). Harrison’s principles of internal medicine (18 ed.). : McGraw Hill. Marino, P. L. (2014). The ICU book (4th ed.). New York, NY: Wolters Kluwer. McLaughlin, V. V., Archer, S. L., Badesch, D. B., Barst, R. J., Farber, H. W., Lindner, J. R., ... Varga, J. (2009). ACCG/AHA 2009 expert consensus document on pulmonary hypertension. Journal of American College of Cardiology, 53(17), 1573-1619. http://dx.doi.org/10.1016/j.jacc.2009.01.004 Moser, D. K., & Riegel, B. (2008). Cardiac nursing: A companion to Braunwald’s heart disease. St. Louis, MO: Saunders Elsevier. Ohio Board of Nursing (2014). The formulary developed by the Committee on Prescriptive Governance. Retrieved from http://www.nursing.ohio.gov/practice.htm Rich, S. (2012). Pulmonary hypertension. In D. L. Longo, D. L. Kasper, J. L. Jameson, A. S. Fauci, S. L. Hauser, & J. Loscalzo (Eds.), Harrison’s principles of internal medicine (18th ed.). New York, NY: McGraw Hill. Rothman, R. B., Ayestas, M. A., Dersch, C. M., & Baumann, M. H. (1999). Aminorex, fenfluramine, and chlorphentermine are serotonin transporter substrates implications for CASE STUDIES 1 AND 2 23 primary pulmonary hypertension. Circulation, 100, 869-875. http://dx.doi.org/10.1161/_01.CIR.100.8.869 The Renal Association. (2011). Acute Kidney injury. Retrieved from http://www.renal.org/guidelines/modules/acute-kidney-injury#sthash.IN7ODao8.dpbs Waikar, S. S., & Bonventre, J. V. (2012). Acute kidney injury. In D. L. Longo, D. L. Kasper, J. L. Jameson, A. S. Fauci, S. L. Hauser, & J. Loscalzo (Eds.), Harrison’s principles of internal medicine (18th ed., pp. 2293-2308). New York, NY: McGraw Hill. Walsh, R. A., O’Rourke, R. A., & Shaver, J. A. (2011). The history, physical, and cardiac auscultation. In V. Fuster, R. A. Walsh, & R. A. Harrington (Eds.), Hurst’s the heart (13th ed.). Retrieved from http://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/book.aspx?book id=376 Yaqub, M. S., & Molitoris, B. A. (2009). Acute kidney injury. In E. V. Lerma, J. S. Berns, & A. R. Nissenson (Eds.), Current diagnosis and treatment: nephrology & hypertension). Retrieved from http://accessmedicine.mhmedical.com.ezproxy.libraries.wright.edu:2048/content.aspx?bo okid=372§ionid=39961145&jumpsectionID=39962184&Resultclick=2