* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download CME: Total Anomalous pulmonary venous Drainage(TAPVD)
Remote ischemic conditioning wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Heart failure wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Cardiac surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
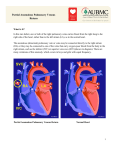
CME: Total Anomalous pulmonary venous Drainage(TAPVD) Incidence: The incidence of total anomalous pulmonary venous drainage is 0.008% of live births, 2.2% in patients with congenital heart disease. What is the TAPVD : Total anomalous pulmonary venous return is a congenital anomaly in which there is no connection between the pulmonary veins and the left atrium; the pulmonary veins instead connect directly into the right atrium or to a systemic vein (Innominate, superior vena cava (SVC), Azygus, inferior vena cava ( IVC) , hepatic vein or portal vein) by an alternative pathway (vertical vein). Because all venous blood returns to the right atrium, the survival of baby depends upon the obligatory connection between the left and right atria. Classification of TAPVD : Darvin et al ( 1957) : Type-I: TAPVR involves drainage into the systemic venous system via a left-side vertical vein (an embryologic remnant of the left cardinal system), which drains into the left brachiocephalic vein or directly into the right superior vena cava. It accounts for 46% of patients who have TAPVR. Incidence: 46% of total cases Type II : It involves drainage directly into the heart, usually via the coronary sinus or directly into the right atrium. Incidence- 26% of total cases. Type III : It involves drainage via a descending vein that courses below the diaphragm and joins the inferior vena cava, hepatic veins, or portal system. This type typically features obstruction of the pulmonary venous return and clinically present during the initial days of extrauterine life. Incidence: 24 % of total cases. Type IV, It is rare, involves multiple sites of drainage. Incidence: approx 5% of total cases. Clinical features : Onset of symptoms: Most patients develop symptoms within the 1st year of life: tachypnea, feeding difficulties, frequent respiratory infections, and failure to thrive. Early onset of symptom: Those patients who have pulmonary venous obstruction may present urgently within the 1st few days of life with tachypnea, cyanosis, and heart failure. Classical Clinical Findings : Unobstructed TAPVD : Classical findings of ASD - wide and fixed split of second heart sound with ejection RV S3 and ejection systolic murmur in an infant presenting with congestive heart failure and borderline cyanosis must raise the suspicion of TAPVD. Obstructed TAPVD : Usually in TAPVD pulmonary venous blood takes a longer course to reach left atria. This pathway can be restrictive at places like at level of interatrial connection or draining ascending or descending vertical vein leading to increase in pulmonary venous pressure and decrease in systemic cardiac output. This diagnosis must be suspected in a very sick cyanosed (borderline) neonate with CHF who has a normal split of second heart sound with loud P2 with RVS3, ESM . Chest X-Ray : The chest radiographs of patients who have unobstructed types of TAPVR typically exhibit right atrial and right ventricular hypertrophy with increased pulmonary blood flow. In patients whose return is to the left brachiocephalic vein, there may be a characteristic enlargement of the superior mediastinum, bilaterally in a figure-8 or snowman shape. An electrocardiogram will usually show right-axis deviation with right atrial P-wave abnormality and right ventricular hypertrophy. Obstructed TAPVC presents with relatively normal cardiac size and features of pulmonary venous hypertension, ground glass opacity. Echocardiography: Two-dimensional echocardiography has been shown to establish the diagnosis accurately. CT Angio/ conventional catheterization : may be necessary if echocardiography is inconclusive in determining the site(s) of the pulmonary venous connections. Treatment: Precise description of the drainage sites is important in determining the suitable surgical approach. The diagnosis of TAPVR is an indication for open heart surgery. If the condition remains untreated, it is usually fatal before 1 year of age. Since 1963, the standard incision has been a median sternotomy. Surgical Mortality and Morbidity Due to better diagnostic capabilities and to improvements in surgical techniques, operative death has decreased from 15.8% in 1984 to as low as 0 in a later case series. The repair of TAPVR has become a surgical procedure with very low risks of morbidity and death. Long-term Outcome of TAPVD repair : The repair of supradiaphragmatic TAPVR in infants, children, and even adolescents is followed a normal life similar to that after the closure of a nonrestrictive ostium secundum atrial septal defect and a long-term survival is expected in most patients. Michielon G, reported a postsurgical survival rate of 87.3% for patients at 18 years of age, with no difference according to anatomic type of TAPVR or surgical technique. Complication:, Major expected morbidities observed in a post op patients are – 1. Post-repair pulmonary venous obstruction (around 11%) : May need reintervention. 2. Pulmonary vein stenosis: May pre exist but may go undetected before the surgery. 3. Late arrhythmias - Like sinus node dysfunction, including sinus bradycardia, sinus pauses, and chronotropic impairment in most of the patients 10 years postoperatively; however, significant atrial and ventricular arrhythmias appear to be uncommon. Suggested Reading : 1. Craig JM ,Darling RC, Pothney WB, Total anomalous pulmonary venous drainage on right side of heart; report of 17 autopsied cases not associated with other major cardiovascular anomalies. Lab invest 1957; 6 (1) 44-64. 2. Bando K. . Turentine MW., Ensing GJ, Surgical management of total anomalous pulmonary venous drainage – 30 year trend. Circulation, 1996,94 (9th suppliment) II12-6 3. Tanel RE., Kirshbom PM, Paridon SM , Hartman DM et al. Long term non invasive arrhythmia assessment after total anomalous pulmonary venous connection repair. Am Heart J. 2007: 153 (2):267-74 4. Cooley DA, Oscar VC, MD, and Fernando MP, Repair of Total Anomalous Pulmonary Venous Return: Results after 47 Years. Tex Heart Inst J. 2008; 35(4): 451–453.