* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download tutorial 1 GUS
Resting potential wikipedia , lookup
Stimulus (physiology) wikipedia , lookup
Cardiac output wikipedia , lookup
Threshold potential wikipedia , lookup
Hemodynamics wikipedia , lookup
Countercurrent exchange wikipedia , lookup
Exercise physiology wikipedia , lookup
Haemodynamic response wikipedia , lookup
Biofluid dynamics wikipedia , lookup
Glucose meter wikipedia , lookup
Common raven physiology wikipedia , lookup
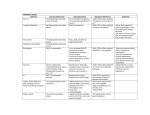
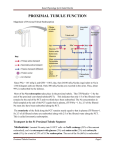
• The functional unit of the kidneys is the _____________________. • Urine is eliminated from the bladder through the ______________. • The two regions of the kidney are an outer ______________and an inner _______________. • Tubular _____________________ and tubular _____________________ are selective processes that occur in the nephron. • The specialized cells of the _____________________, located within the _____________________, detect changes in the rate at which fluid is flowing past them through the distal tubule. Regional differences in nephron structure Cortical nephrons - have glomeruli located in the ------------------------. - have ______________loops of Henle that penetrate only a short distance into the ________________ Regional differences in nephron structure (cont.) Juxtamedullary nephrons. - have glomeruli that lie ______________cortex near the medulla - have ______________loops of Henle that dip deeply into the _________________. • have specialized peritubular capillaries _________________ • The kidney produces following hormones : • Erythropoietin • 1,25 dihydroxycholecalciferol (Vitamin D3, calcitriol) • Renin • The fluid within the Bowman’s capsule virtually the same as in the plasma. • Except • It is free from: – _______________ – ________________ • Fluid filtered pass through three layers of the glomerular membrane • ________________________ • _________________________ • __________________________ GFR: Definition: The volume of plasma filtered from both kidneys per minute. • GFR = _______ ml/min = _______ liters/day • GFR= _____________ x ______________ • Forces determining Net Filtration Pressure (NFP) – ___________________ – ____________________ – ________________________ • NFP = ( PGC + BC ) - ( PBC + GC ) • Calculate NFP if – Glomerular capillary hydrostatic pressure = 60 – Plasma colloidal osmotic pressure is = 40 – Bowman's capsule hydrostatic pressure is = 10 – Ans = 10 • Increase of PBc can be caused by 1. _________________________ 2. _________________________ 3. _________________________ • plasma colloid osmotic pressure increases ________________ Decreases __________________ Adjustments of Afferent Arteriole Caliber to Alter The GFR Baroreceptor Reflex Influence on the GFR Autoregulation The major function of autoregulation in the kidneys is to maintain a relatively constant GFR and renal blood flow despite considerable arterial pressure fluctuations that can occur. Autoregulation: • Myogenic autoregulation TWO THEORIES • Tubuloglomerular feedback Myogenic Mechanism Vascular smooth muscle contraction in response to increased stretch Arterial Pressure Stretch of Blood Vessel Cell Ca++ Permeability Blood Flow Vascular Resistance Intracell. Ca++ Macula Densa Feedback (Tubuloglomerular feedback) GFR Distal NaCl Delivery Macula Densa NaCl Reabsorption (macula densa feedback) Afferent Arteriolar Resistance GFR (return toward normal) What is a Glomerular Filtration Fraction? • The Filtration Fraction (FF) is the ratio of the GFR to the renal plasma flow (GFR/TRPF). • Renal blood flow = 1.1 L/min • 20-25% of total cardiac output (5 L/min). • Of the 625 ml of plasma enters the glomeruli via the afferent, 125 (the GFR) filters in the Bowman’s capsule, the remaining passing via efferent arterioles into the peritubular capillaries • Filtration fraction = (GFR/TRPF) = 0.2 • So, GFR is About 20% of the Renal Plasma Flow The filtration fraction The Filtration Fraction (FF) is the ratio of the GFR to the renal plasma flow = (GFR/TRPF). Reabsorption and Secretion The amount of a substance filtered into Bowman's space per unit time is called the filtered load: • Filtered load = _____ • Excretion rate = _____ _________ __________ • Reabsorption/secretion rate = FL – Excretion rate Reabsorption ROUTES Reabsorption - Transport Mechanisms WHAT ARE THE DIFF MECHANISMS ? – Primary active transport EXAMPLE ? • Sodium-potassium pumps in basolateral membrane only – Secondary active transport – EXAMPLE ? • co-transport (glucose, amino acids) • counter-transport (K+, H+) – Passive Reabsorption – EXAMPLE ? • Osmosis (H2O) • Electrostatic attraction (Cl-) Sodium Reabsorption Glucose Reabsorption SGLT 2 GLUT 2 Reabsorption Transport Maximum(Tmax) • DEF:_________________________________________ • WHAT creates a limit to the rate of substances transport. ? SATURATION OF TRANSPORT PROTEINS • Therefore, excess of that substance is ____________ • EXCRETED Glucose Transport Maximum Figure 27-4; Guyton and Hall RENAL THRESHOLD FOR GLUCOSE • DEFINITION ? • The is the plasma level at which the glucose first appears in the urine . • The actual renal threshold is about • 200 mg/dL of arterial plasma, • which corresponds to a venous level of about 180 mg/dL. • What causes in splay ? – TmG in all the tubules is not identical and – All the glucose were not removed from each tubule when the amount filtered was below the TmG. GFR = 120 ml/min, Plasma glucose of 200 mg/dl (2mg/ml), transport max (Tm) 200 mg/min What is the glucose excretion for this patient? Passive Reabsorption • Passive reabsorption depends on: – Electrical gradient (electrostatic attraction). – Concentration gradient – Membrane permeability – Time available in the tubule for reabsorption Passive Reabsorption Secondary water Reabsorption via osmosis Sodium reabsorption makes both intracellular and extracellular fluid hypertonic to the tubular fluid. Water follows with sodium into the peritubular capillaries. Na+ Na+ H2O capillary Tubular cell Tubular lumen Passive Reabsorption Secondary ion reabsorption via electrostatic attraction Negative ions (Cl-) tend to follow with the positive sodium ions by electrostatic attraction. Na Na+ Cl- capillary Tubular cell Tubular lumen Urea–Example of Passive Reabsorption Na+ reabsorption H2O reabsorption Increase concentration of urea in tubular fluid Passive reabsorption of urea Mechanisms by which Water, Chloride, and Urea Reabsorption are Coupled with Sodium Reabsorption Figure 27-5; Guyton and Hall PAH –EXAMPLE OF SECRETION • • • • PAH is an organic acid Used for measurement of renal plasma flow Both filtered and secreted PAH transporters located in peritubular membrane of proximal tubular cells. • There are parallel secretory mechanism for secretion of organic bases like quinine and morphine PAH Filtration, Secretion & Excretion References • Human physiology by Lauralee Sherwood, seventh edition • Text book physiology by Guyton &Hall,11th edition • Text book of physiology by Linda .s contanzo,third edition