* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Nursing Consideration
Coronary artery disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
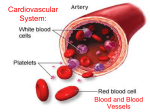
Cardiac arrest wikipedia , lookup
CARDIOVASCULAR SYSTEM Diagnostic and Laboratory Studies Prepared By Ms. Jennifer Castillon,RN.MAN. Electrolytes Coagulation Studies Erythrocyte Studies White Blood Cell Count Serum Enzymes and Cardiac Markers Serum Lipids ECG CVP Pericardiocentesis ELECTROLYTES POTASSIUM (3.5 – 4.5mEq/L) Nursing Consideration: A-ccurate note if the patient is receiving K supplement B-lood should not be drawn from site where an IV infusion exists C-lenching and unclenching of hand can increase the level ELECTROLYTES HYPERKALEMIA – elevated potassium level Results to ECG changes like: Tall, peaked T wave Prolonged PR interval Loss of P wave Widening of QRS complex which lead to ventricular fibrillation or cardiac arrest. ELECTROLYTES HYPOKALEMIA – decreased potassium level Results to ECG changes like: Presence of U wave premature ventricular contractions (PVC’S) which can deteriorate into VT or VF. ELECTROLYTES MAGNESIUM (1.5 -2 mEq/L) Nursing Consideration: P-rolong use of magnesium products will cause increased serum levels -arenteral nutrition therapy or P excessive loss of body fluids may decrease serum levels Hypomagnesemia Hypermagnesemia ELECTROLYTES CALCIUM (4.8- 8.5 mg/dl) Nursing Consideration: Instruct the client to eat a diet with a normal calcium level (800 mg/day) for 3 days before the test. Instruct the client that fasting may be required for 8 hours before the test ELECTROLYTES HYPERCALCEMIAincreased level of calcium. Rhythm disturbances may include: Bradycardia; first, second and third degree heart block and RBBB ELECTROLYTES HYPOCALCEMIA- decreased level of calcium. myocardial contractility, cardiac output and hypotension. ECG prolonged QTc interval leads to life-threatening ventricular dysrthymia. COAGULATION STUDIES ACTIVATED PARTIAL THROMBOPLASTIN TIME (APTT)- to measure the effectiveness of IV or subcutaneous heparin administration. A-mount of time it takes in seconds for recalcified plasma to clot after partial thromboplastin is added P-erformed for patient receiving heparin T-est for deficiencies and inhibitors of clotting factors T-ime: 20 to 36 seconds COAGULATION STUDIES PROTHROMBIN TIME (PT) and INTERNATIONAL NORMALIZED RATIO (INR)- to determine therapeutic dosage of warfarin necessary to achieve anticoagulation. P-rothrombin is a vitamin K dependent glycoprotein produced by the liver for fibrin clot formation T-o monitor response to warfarin sodium (Coumadin) COAGULATION STUDIES PROTHROMBIN TIME (PT) and INTERNATIONAL NORMALIZED RATIO (INR) Normal Values: PT: – 9.6 to 11.8 secs (male) – 9.5 to 11.3 secs (female) INR: – 2.0 to 3.0 (standard warfarin tx) – 3.0 to 4.5 (high dose warfarin tx) COAGULATION STUDIES PROTHROMBIN TIME (PT) and INTERNATIONAL NORMALIZED RATIO (INR) Nursing Considerations: A - baseline PT should be drawn before anticoagulation therapy B -e sure to apply direct pressure to the venipuncture site C -oncurrent warfarin therapy with heparin therapy can lengthen the PT D -iets high in green leafy vegetables can shorten PT E -xpect 1.5 to 2 times longer PT if on anticoagulation therapy F -or PT greater than 30 secs, initiate bleeding precautions COAGULATION STUDIES PLATELET COUNT Plug formation Clot retraction Coagulation factor activation COAGULATION STUDIES PLATELET COUNT Nursing Considerations: B-leeding precautions should be instituted in clients with low platelet M-onitor venipuncture site C-hronic cold weather, high altitudes, and exercise increase platelet count ERYTHROCYTE STUDIES RED BLOOD CELLS 4.5-6 million/mm3 in males 4-5.5 million/mm3 in females • <RBC – Anemia (Fatigue, SOB) • >RBC – Polycythemia (erythrocytosis) – ERYTHROCYTE STUDIES HEMOGLOBIN Hemoglobin is the main component of erythrocytes and serves as the vehicle for transporting O2 and CO2 Normal Values: – 14 to 18g/dl (male) – 12 to 16 g/dl (female) ERYTHROCYTE STUDIES HEMATOCRIT Hematocrit represents the volume percentage of RBC’s in whole blood and is an important measurement in the identification of anemia or polycythemia Normal Values: – 40% to 54% (male) – 38% to 48% (female) WHITE BLOOD CELL COUNT WHITE BLOOD CELL or leukocytes Immune defense system of the body WBC 5,000-10,000 cells/mm3 – <WBC – leukopenia (risk for infection) – >WBC – leukocytosis (infection/inflammation) – >100,000 – incapable of phagocytosis (leukemia) CARDIAC BIOMARKERS OR CARDIAC ENZYMES CREATINE KINASE (CK) Found in: CK-MB (Cardiac)--- 0% to 5% CK-BB (Brain)--- 0% CK-MM (Muscles)--- 95% to 100% Rise- 4-8hours after MI Peak – 15 -24 hours Remain elevated – 2-3days CARDIAC MARKERS CREATINE KINASE (CK) Nursing Considerations: CK-MM: Avoid strenuous physical activity for 24 hours before the test Avoid ingestion of alcohol for 24 hours before the test Invasive procedures and intramuscular injections may falsely elevate CK levels CARDIAC MARKERS Troponin T and Troponin I Elevation occurs after 3 – 6hours after the acute myocardial damage has occurred. CARDIAC MARKERS LACTASE DEHYDROGENASE (LDH) Nursing Considerations: LDH isoenzyme levels should be interpreted in view of the clinical findings Testing should be repeated on 3 consecutive days CARDIAC MARKERS MYOGLOBIN – nonspecific indicator of myocardial cell damage both cardiac and skeletal muscle. Injury to skeletal muscle will cause a release of myoglobin into the blood. Rise about 1 – 4hours after myocardial injury SERUM LIPIDS Total Cholesterol--140 to 199 mg/dl Low Density Lipoprotein (LDL)--- <130 mg/dl High Density Lipoprotein (HDL)--- 30 to 70 mg/dl Triglycerides--< 200 mg/dl SERUM LIPIDS Nursing Considerations: No oral contraceptives NPO except water for 12 to 14 hours No alcohol for 24 hours No high cholesterol foods the evening meal before the test ECG E -valuates heart rate and the regularity of heartbeats. C-ardiac dysrhythmias, MI, and cardiac hypertrophy - raph of the electrical G impulses moving through the heart. ECG Nursing Consideration: E -lectrical shock will not occur C-ardiac medications of the patient should be documented G-ive instructions to lie still, breathe normally, and refrain from talking during the test Central Venous Pressure (CVP) C-atheter is attached to an IV infusion and H2O manometer by a three way stopcock V -eins external jugular, antecubital, or femoral P - ressure within the superior vena cava CVP Normal Value: 3 to 8 mmHg Position: Cardiac Disease: Semi Fowler’s Dressing or Tubing Change: Flat or Trendelenburg CVP Reading and Monitoring: Flat, Supine, or Dorsal Recumbent Air Embolism: Left Side Lying CVP 1. Maintain zero point of manometer always at level of right atrium (intersection between midaxillary line and 4th ICS, also referred to as the phlebostatic axis) 2. Determine patency of catheter by opening IV infusion line 3. Turn stopcock to allow IV solution to run into manometer to a level of 10-20cm above expected pressure reading 4. Turn stopcock to allow IV solution to flow from manometer into catheter; fluid level in manometer fluctuates with respiration 5. Stop ventilatory assistance during measurement of CVP 6. After CVP reading, return stopcock to IV infusion position 7. Record CVP reading and position of client (angle of recline) PERICARDIOCENTESIS Pericardial effusion Puncture Pericardial sac Pericardial fluid PERICARDIOCENTESIS PRE-PROCEDURE P erform blood analysis E CG R estriction of food and water is recommended for six hours before the test. I V line for sedation PERICARDIOCENTESIS A B C D INTRA-PROCEDURE vail emergency resuscitative equipment at bedside ed is elevated to 45 to 60 degrees ardiac activity monitoring one in emergency room, ICU, or at the bedside PERICARDIOCENTESIS POST-PROCEDURE A pical pulse monitoring B lood pressure C VP D etect complications: Ventricular or coronary artery puncture, dysrhythmias, pleural laceration, gastric puncture, myocardial trauma • THANK YOU