* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download (12) Endocrine System
Survey
Document related concepts
Transcript
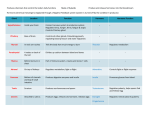
Endocrine System Dr. Carmen Rexach Physiology Mt San Antonio College Relationship between endocrine and neural physiology • Both neurons and endocrine cells can secrete into the blood stream • Endocrine cells and neurons generate electrical potentials when depolarized • Peptides produced by endocrine cells have neurotransmitter function & can act as hormones • A single cell can produce biogenic amine neurotransmitters and peptide hormone molecules • A single gene can be transcribed/translated to produce either peptide neurotransmitter or hormone Structural classification of hormones • Amino Acid derivatives • Peptide hormones • Lipid derivatives Amino Acid Derivatives • Derivatives of Tyrosine – Catecholamines • epinephrine and norepinephrine (adrenal medulla) • dopamine (hypothalamus) – Thyroid hormones • T3, T4 • Derivatives of Tryptophan – Melatonin (pineal gland) Peptide Hormones • Short polypeptides (<200 amino acids) – ADH, ACTH, insulin, PTH, Calcitonin, ANF, GI tract hormones and others • Proteins – TSH,LH, FSH, erythropoietin, renin, inhibin Lipid derivatives • Steroid hormones – cholesterol derivatives – androgens, estrogens, progestins, hormones of adrenal cortex, and others • Eicosanoids – arachadonic acid derivatives – prostaglandins, leukotrienes, thromboxanes, prostacyclins, etc. Lipid derivatives Prohormones and prehormones • Prohormones – long chained precursor – cut and spliced to produce endproduct(s) • Prehormones – produced in inactive form – require modification to become active – examples • T4 T3 at target cell • testosterone • Vitamin D3 Response at the target cell • Hormone must be recognized by specific cell receptor • Hormone/receptor complex must be coupled to signal-transduction mechanism • The generated signal must cause a change in intracellular processes by changing the activity or concentration of enzymes, carrier proteins, etc. Hormone interactions • Synergistic and permissive effects – synergistic: working together • additive (epinephrine, norepinephrine on heart) • complementary (FSH/LH on spermatogenesis) – permissive: potentiation • increased response of target cell to a 2nd hormone • increased activity of second hormone • Antagonistic effects: opposition – insulin/glucagon Hormone concentration • Half-life of hormone – Time required for the blood [hormone] to be reduced to ½ reference level • Minutes to days • Concentration – physiological level • amount necessary for normal function – pharmacological level • too much – incidental binding to protein receptors with similar structure but less affinity – secondary conversion into other products – Results: varying effects in body Upregulation and downregulation • Upregulation (Priming effect) – chronically low levels of hormone in ECF leads to increase of number and sensitivity of protein receptors for that hormone • Downregulation (Desensitization) – chronically high levels of hormone in the ECF leads to decrease in the number and sensitivity of protein receptors for that hormone – Prevented by pulsatile secretions Relationship to NIDDM • Non-insulin dependent diabetes mellitus – obesity – increased sugar consumption leads to increase in circulating insulin – chronic increase in insulin levels leads to downregulation of insulin receptors on cell surfaces – cells become refractory to insulin – can result in atrophy of the β cells and insulin dependence Mechanisms of hormone action • Same category = similar mechanism • Determined by: – location of receptor – cellular response to receptor activation • Location of Receptor – Nonpolar hormones • in nucleus of target cell • in cytoplasm of target cell – Polar hormones • on outer surface of plasma membrane Steroid and thyroid hormones • Nonpolar – into plasma attached to carrier proteins – dissociate in blood near target – hormone into target • moves into cell and binds to intracellular receptor • alterations allow for direct binding to DNA • Result: genetic transcription (mRNA synthesis) Steroid hormones Result: turn a key metabolic pathway on or off Steroid Hormones: In nucleus • DNA-binding domain of receptor binds to specific HRE of the DNA. • Dimerization occurs. – Process of 2 receptor units coming together at the 2 half-sites. • Stimulates transcription of particular genes. Thyroid hormones T4 T3 Result: turn key enzymes in a metabolic pathway on or off Mechanism of Thyroid Hormone Action • T4 passes into cytoplasm and is converted to T3. • Receptor proteins located in nucleus. – T3 binds to ligand-binding domain. – Other half-site is vitamin A derivative (9-cisretinoic) acid. • DNA-binding domain can then bind to the half-site of the HRE. – Two partners can bind to the DNA to activate HRE. • Stimulate transcription of genes. Peptide hormones • Polar = restricted to cell surface • Utilize second messenger system Second messenger = cAMP α G-protein Protein kinase Adenylate cyclase ATP PO43- cAMP +Pi Result: Turn key enzyme in a metabolic pathway on or off Second messenger = Ca++ epi α adrenergic receptor PLC Ca++ DAG PIP2 IP3 Ca++ Protein kinase calmodulin Epi Can Act Through Two 2nd Messenger Systems Remember • Different hormones have different effects on same target cell • Response of target cell to same second messenger can differ in different cells Endocrine glands and their products Pituitary gland structure Anterior pituitary • Trophic effects: – High blood [hormone] causes target organ to hypertrophy. – Low blood [hormone] causes target organ to atrophy. Hormones of anterior pituitary • GH = somatotropin – Generalized growth promoting effects • TSH = thyrotropin – Regulates activity of thyroid gland • ACTH = corticotropin – Regulates activity of adrenal cortex • PRL = prolactin – Mammary growth, development, lactogenesis • Gonadotropins – FSH = folliculotropin – LH = leutotropin Pituitary hormones: pars intermedia & posterior • Pars intermedia – MSH – Beta (β)-endorphins • Posterior pituitary – ADH – oxytocin Hypothalamic Control of Posterior Pituitary • Hypothalamus neuron cell bodies produce: – ADH: supraoptic nuclei. – Oxytocin: paraventricular nuclei. • Transported along the hypothalamohypophyseal tract. • Stored in posterior pituitary. • Release controlled by neuroendocrine reflexes. Hypothalamic control of anterior pituitary • Hypothalamopituitary portal vessel • releasing hormones: polypeptides released by the hypothalamus – TRH TSH – CRH ACTH – GnRH FSH/LH – GHRH GH • inhibiting hormones – PIH PRL – Somatostatin GH Negative feedback loops Hypothalamus Increased secretion hormone #1 stimulus - - - Increased plasma hormone #1 Anterior pituitary Increased secretion hormone #2 Increased plasma hormone #2 3rd Endocrine gland Increased secretion hormone #3 Increased plasma hormone #3 Target cells of hormone #3 Respond to hormone #3 Positive feedback effect • Amplifies initial biological effect of hormone estradiol LH Pituitary gland disorders Identical twins Acromegaly Acromegaly vs. Gigantism Influence of higher brain functions • Emotions • Stress • Circadian rhythms – somatotropin released in greatest quantities during first 90 minutes of sleep – estradiol on GnRH response Adrenal gland Functions of the adrenal cortex • Mineralocorticoids – zona glomerulosa – aldosterone = Na+/K+ regulation • Glucocorticoids – zona fasciculata – cortisol and corticosterone – protein and carbohydrate metabolism • Sex steroids – zona reticularis – androgens and estrogens = maintenance of secondary sex characteristics Adrenal Cortex Stress and the adrenal gland • Stimulate pituitary-adrenal axis due to chronic controlled stress – increased secretions of ACTH – increased secretions of glucocorticoids • Sympathetic response – stimulation of adrenal medulla – response to physical challenge or physically challenging stressors Stress and the Adrenal Gland • Three phase response – 1) Alarm phase • Adrenal glands activated. – 2) Stage of resistance • Stage of readjustment. – 3) Stage of exhaustion • Sickness and/or death if readjustment is not complete. Adrenal gland disorders: Cushing’s syndrome Caused by excess production of ACTH Classic symptoms seen in this 23 y.o. female hirsutism (face) central obesity hyperpigmentation & striae Cushing’s syndrome Thyroid gland Thyroid Hormones • located just below the larynx • largest of the pure endocrine glands • Follicular cells secrete thyroxin • Parafollicular cells secrete calcitonin Production of thyroid hormones • 2I- + H2O2 I2 – iodide enters cell by secondary cotransport with Na+ • I2 + HO Tyrosine • DIT + DIT • MIT + DIT MIT CH2CHCOOH DIT NH2 Tetraiodothyronine T4 (thyroxine) T3 triiodothyronine Production and release • T3 and T4 produced. • TSH stimulates pinocytosis into the follicular cell. – Enzymes hydrolyze T3 and T4 from thyroglobulin. • Attached to TBG and released into blood. Secretion of T3/T4 • T4 circulates bound to protein • Protein allows for transport in the plasma and through the cytosol in the cell for access to nuclear receptors Binding proteins • three major binding proteins produced in the liver – thyroxine-binding pre-albumin (TBPA) • binds 70-75% of T4 – thyroxine-binding globulin (TBG) • binds 15-20% of T4 – albumin • 5-10% of T4 T3 vs T4 • Both of these are water insoluble, but certain binding proteins have greater affinity for T4 • T4 concentrations in humans 50x’s greater than T3 • Functions – T3 physiologically relevant hormone – T4 involved in negative feedback loop on pituitary production of TSH & production of TRH by the hypothalamus Effects • Protein synthesis • maturation of nervous system • increased BMR – during prolonged fasting plasma T3 levels decrease (ever wonder why it is harder to loose weight when you start dieting?? Your body is prolonging your survival by minimizing its energy usage!) • Thyroid diseases – Goiter – Graves disease – Cretanism/myxedema Diseases of the Thyroid • 1) Iodine-deficiency (endemic) goiter • 2) Abnormal growth of the thyroid gland. • 3) In the absence of sufficient iodine, cannot produce adequate amounts of T4 and T3. • 4) Lack of negative feedback inhibition. • 5) Stimulates TSH, which causes abnormal growth. Goiter Graves disease: hyperthyroidism exopthalmos Digital clubbing Myxedematous cretinism 20-year-old African male with three cretin women of the same age Characteristics: Mental retardation Severe growth retardation Delayed sexual maturation Incomplete maturation of features Puffy, thickened skin hypothyroidism Parathyroid gland Parathyroid hormone • Major regulator of Ca++ metabolism • Effect – increase plasma Ca++ by • stimulation of bone resorption • renal tubular Ca++ reabsorption • synthesis of 1,25-(OH)2-D3 – decrease plasma PO43- • Regulated by plasma Ca++ concentration RICKETS OSTEOMALACIA: 25 YO FEMALE Pancreas: Islets of Langerhans Islets of Langerhans • Four major cell types – Alpha (α) cells = glucagon – Beta (β) cells = insulin – Delta (δ) cells = somatostatin (inhibition of insulin, glucagon, and assimilation rate of nutrients in GI tract) – F cells = pancreatic polypeptide (inhibits pancreatic exocrine secretion) Pineal gland • Located in brain in roof of 3rd ventricle Pineal gland • Major site of melatonin synthesis – highest levels of secretion at night • Controversial effects – Alleviation of jet lag after transmeridial flights – Antigonadal effects = inhibition of melatonin is trigger for puberty onset • Continuous light leads to early onset of sexual development Thymus Thymus • Location: behind manubrium of sternum • attains weight of approximately 40 grams at puberty, then begins to involute • Function: development of immune response • Hormone: thymosin – T cell education GI tract, gonads, placenta • GI tract • Gonads – Androgens – Estrogens – Progestones • Placenta – – – – Estrogens Progesterone Human chorionic gonadotropin somatomamotropin