* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Electrophysiology Part 2 Worksheet Answers
Quantium Medical Cardiac Output wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
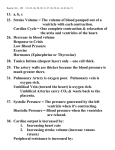
Heart failure wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Myocardial infarction wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Coronary artery disease wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Electrocardiography wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Electrophysiology Worksheet 2 Answers 1. SA node- 60-100 Atrial foci- 60-80 AV junction- 40-60 Purkinje fibers- 20-40 (generally referred to as the ventricular rate). Through overdrivesuppression the SA node should be the heart’s pacemaker, causing these other foci to fire at the SA node’s rate (so you only see the SA node firing). 2. We typically look at lead II. In lead II EKG placement you have a negative lead right arm, positive lead left leg, grounding lead right leg. 3. An EKG printout is a graphical representation of your EKG rhythm. It often uses heat sensitive paper, so if you leave it in a hot area the paper might darken or you may not have a visible printout. The paper has 1mm x 1 mm boxes, with darker big boxes every 5x5. The monitor requires calibration so that vertically each 1 mV = 10 mL. It also requires calibration so that the EKG paper paper moves through machine at 25 mm/sec, to create a small box (horizontal) 1mm = 0.04 seconds (or, 30 large boxes = 6 seconds). 4. P wave- <0.11 wide and <2.5 mm tall in lead II. They should all be upright and shaped similarly to each other with a nice curve. Variations indicate atrial hypertrophy, hyperkalemia, premature atrial beats, or rhythms originating from outside of the SA node. PR interval- 0.12-0.20 sec wide. (3-5 squares)If it’s short, consider WPW or muscular dystrophy (Duchenne). If it’s long, it is a 1 degree HB. QRS- <0.12 sec wide (3 small squares). If it’s wide, see #7. ST segment- Has no elevation or depression. If 1 or more small squares elevated it indicates AMI, BBB, pericarditis, ventricular pacemaker, or a normal finding especially in athletes. If 1 or more small squares depressed it indicates myocardial ischemia, dig effects, BBB, posterior AMI, pulmonary embolus, ventricular hypertrophy. T wave- Height should be <5 mm in the limb leads and <15 mm in the precordial leads. Should be upright except in aVR and sometimes V1. Peaked (sharp looking) T waves often indicate hyperkalemia. Broad asymmetrically peaked T waves often indicate early AMI or coronary artery vasospasm (Prinzmetal angina). Inverted T waves may be normal, especially in kids (juvenile T wave pattern). These are typically <3 mm deep and might continue into adulthood, especially with Afro-Caribbean women. T waves may also indicate ischemia, PE, cardiac hypertrophy, increased ICP, BBB. Inversion in lead III may be normal- but if there is a change it is not. R-R interval- varies based on HR QT interval- should be less than half of the R-R interval. The actual calculation is dividing the QT interval by the square root of the preceding R-R interval. Prolonged QT may indicate AMI, metabolic derangement, cerebral bleeding, drugs (amiodarone), genetics. It is associated with increased risk of sudden death. A very short QT interval may indicate severe hypercalcemia. 5. The SA node impulse begins before the P waves (it doesn’t appear on the EKG). Depolarization of the atria happens with the P wave. The PR interval represents the impulse depolarizing from the SA node all the way through the ventricles. The QRS is the depolarization of the ventricles. The ST segment is the length of time from the end of ventricular depolarization to the beginning of ventricular repolarization. The T wave represents the repolarization of the ventricles. 6. ST segment elevation of greater than 1 small box (=1 mm = 0.1 mV) in two contiguous leads 7. A widened QRS indicates an impulse that is ventricular in origin (including ventricular implanted pacemakers) or an aberrantly conducted beat/rhythm (like from a block, hypothermia, WPW, LVH, RVH…). It sometimes happens with hyperkalemia and other metabolic derangement/drugs that cause aberrant conduction. 8. SA and AV nodes are supplied by the RCA (usually). The RCA also supplies part of the bundle branches. Sometimes the SA node is supplied by the circumflex artery, which branches off of the left coronary artery. The LAD supplies most of the interventricular septum, so it also usually supplies most of the bundle branches. With the circumflex artery, it also supplies the anterior papillary muscles. The circumflex and RCA both supply the posterior papillary muscles. 9. The LCA supplies the left atrium, left ventricle, interventricular septum, and part of the right ventricle. It also supplies the pulmonary artery and aortic root. The LCA divides into the LAD and the circumflex artery. The LAD supplies the anterior, lateral, and apical wall of the left ventricle and the interventricular septum. The LAD is responsible for up to 50% of MIs- it is the most common site for an MI. The circumflex artery supplies the posterior and lateral wall of the left ventricle and is responsible for 15-20% of MIs. The RCA supplies the right atrium, right ventricle, part of the interventricular septum (surrounding part of the bundle branches), and part of the left ventricle. It divides into the RAD and the marginal branch of the RCA. The RCA supplies the right ventricle (in most people) and the posterior and inferior heart. The RCA as a whole is responsible for 30-40% of MIs. Coronary arteries supply 200-250 mL blood to the heart every minute, of which the LCA transports 85%. Anastomoses may develop so that the heart has collateral circulation- this may or may not be pathological. 10. Sinus rhythms originate in the SA node. On the EKG the beats have P waves before every beat that are upright and look the same. The QRS is narrow unless there is underlying pathology (not relevant yet). Normal sinus rhythm is regularly regular at a rate of 60-100. Sinus bradycardia is regularly regular with a rate of less than 60. ST is regularly regular with a rate of over 100. Sinus dysrhythmia is not regularly regular. It is often (but not always) changing with respirations, getting faster with inhalation and slowing with exhalation. The difference should be 10 bpm to meet this criteria but may be as many as 30. 11. SB- Beta blocker or other medication use, sometimes normal (especially in athletes), at times related to disease process, severe HTN, head injury, electrolyte derangement, shock (late), and many other causes. ST- stress, coffee, sympathomimetic use, hypoxia, shock (early), sepsis, hypotension, and many other causes. Sinus dysrhythmia- usually normal in kids and young adults. In older adults it may be normal or associated with lung disease. 12. Low voltage is a QRS amplitude in the limb leads of <5 mm or in the precordial leads of <10 mm. It might occur when there is a lot of space (like fat or air) between the heart and the electrodes (look out of pericardial or pleural effusion, pneumothorax, or emphysema!), after a big MI, or with pericarditis, dilated cardiomyopathy, sarcoidosis, or scleroderma. 13. High voltage QRS has a lot of criteria that people use for determination. The most common is the Sokolov-Lyon criteria, where you look at the S wave depth in V1, add that to the tallest R wave height in V5/V6, and have a positive result if your number is >35. It might be normal, especially in young people or athletes, or might indicate LVH. 14. Electrical alternans is when normally conducted (not premature or escape beats) QRS vary in height. It is typically caused by the movement back and forth in the body of a heart that has a major pericardial effusion, which creates a triad of electrical alternans, low voltage, and tachycardia.