* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 20 - mwsu-wiki
Breast development wikipedia , lookup
Norepinephrine wikipedia , lookup
Menstrual cycle wikipedia , lookup
Mammary gland wikipedia , lookup
Xenoestrogen wikipedia , lookup
History of catecholamine research wikipedia , lookup
Neuroendocrine tumor wikipedia , lookup
Triclocarban wikipedia , lookup
Hormone replacement therapy (male-to-female) wikipedia , lookup
Endocrine disruptor wikipedia , lookup
Bioidentical hormone replacement therapy wikipedia , lookup
Hyperthyroidism wikipedia , lookup
Hyperandrogenism wikipedia , lookup
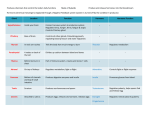
Chapter 20 Mechanisms of Hormonal Regulation Mechanisms of Hormonal Regulation Huether, S.E. (2006). Mechanisms of hormonal regulation. Found in McCance, K.L. & Huether, S.E. Pathophysiology: The Biologic Basis for disease in Adults and Children (5th ed.) St.Louis: MO: ElSevier. - Endocrine glands respond to specific signals by synthesizing and releasing hormones into the circulation - Shared general characteristics of hormones: 1. Hormones have specific rates and rhythms of secretion a. diurnal patterns b. pulsatile and cyclic patterns c. dependent on circulating substrates 2. Hormones operate within feedback system (positive or negative) 3. Hormones affect only cells with certain receptors 4. Kidney excrete hormones, Liver metabolizes hormones - Hormones classified according to their structure, gland of origin, effects, and chemical composition. (Table 20-1, p 656) Regulation of Hormone Release - Hormone release is regulated by chemical factors, endocrine or hormonal factors (hormone from one endocrine gland controlling another endocrine gland), and neural control. - Negative feedback is the most common type of feedback system Important in maintaining hormones within physiologic ranges Hormone Transport - Hormones are released into the circulatory system by the endocrine glands; they are circulated throughout the body. - Peptide (protein) hormones are water soluble and circulate in free form - Lipid-soluble hormones are primarily circulated bound to carrier or binding proteins ( Table 20-2, p 658) - Water-soluble hormones bind to one of four classes of cell surface receptors, whereas lipid-soluble hormones bind to plasma membrane receptors or diffuse through the plasma membrane and bind to cytosolic or nuclear receptors. Cellular Mechanism of Hormone Action - Target cell is a cell that is receptive to a specific hormone - Target cell’s have 2 main functions 1. Recognize and bind with high affinity to their particular hormones 2. Initiate a signal to appropriate intracellular effectors - Binding with receptors general stimulates 3 general types of responses by: 1. Acting on pre-existing channel forming proteins to alter membrane channel permeability 2. Activating pre-existing proteins through a second messenger system 3. Activating genes to cause protein synthesis - Up-regulation - low concentration of hormone increase the number of receptors per cell - Down-regulation - high concentrations of hormone decrease the number of receptors - Direct effect - are the obvious changes in cell functions that specifically result from stimulation by a particular hormone - Permissive effects are less obvious hormone-induced changes that facilitate the maximal response or functioning of a cell Hormone Receptors - Hormone receptors may be located in or on the plasma membrane or in the intracellular compartment of the target cell. Plasma Membrane Receptors and Signal Transduction - Receptor for most water soluble hormones are located on the plasma membrane of a target cell. - Sometimes a hormone or ligand that binds to a receptor is referred to a first messenger. The hormone binding to is specific receptor represents the fist signal within an elaborate signal transduction cascade - Transduction cascade is the process by which extracellular signals are communicated into a cell (series of steps) - Cell surface receptors usually are classified according to their functions 1. G protein-linked receptors 2. Ion-channel receptors 3. Enzyme-linked receptors (Table 20-4, p 661) Steroid (Lipid-Soluble) Hormone - The lipid-soluble hormones are classified as steroid hormones; small hydrophobic molecules (synthesized from cholesterol) - Recent studies indicate there are steroid hormone receptors in the plasma membrane associated with rapid response that have nongenomic and genomic effects. Structure and Function of the Endocrine Gland Hypothalamic-Pituitary Axis - One of the most important and prominent portions of the endocrine system - Communication or anatomic connection (blood vessel & neural tract) between the hypothalamus and anterior and posterior pituitary is elaborate - Hypothalamus is connected to the anterior pituitary by way of portal hypophysical blood vessels - Hypothalamus is connected to the posterior pituitary by way of a nerve tract (hypothalamohypophysial tract) - Connections are vital to the functioning of the hypothalamus-pituitary system (feedback loop) Hypothalamus - Divided into several nuclei and nuclear areas located at the base of the brain - ADH (Antidiuretic hormone) and Oxytocin are synthesized ti hypothalamic neurons but are stored and secreted by the posterior pituitary - Several releasing/inhibitory hormones such as corticotrophin-releasing hormone (CRH) are synthesized in the hypothalamus and control the release of tropic hormones (ACTH from the anterior pituitary) - Other releasing/inhibitory hormones synthesed in the hypothalamus that influence the release of anterior pituitary tropic hormones include thyrotropin-releasing hormone (TRH), growth hormone-releasing hormone (GHRH), gonadotropin-releasing hormone (GnRH), somatostatin, dopamine, and substance P (Hypophysiotropic hormones) Pituitary Gland - The anterior Pituitary (adenohypopysis) composed of 3 regions 1. Pars Distalis - major component of the anterior pituitary and the source of the anterior pituitary hormones 2. Pars Tuberalis - thin layer of cells on the anterior and lateral portion of the pituitary stalk 3. Pars Intermedia - lies between the two lobe of the pituitary gland - The posterior Pituitary (neurohypophysis) consist of 3 parts 1. The median eminence located at the base of the hypothalamus (a) composed largely of the nerve endings that arise in the ventral hypothalamus (b) contains at lease 10 biologically active hypothalamic releasing hormones, dopamine, norepinephrine, serotonin, acetylcholine, and histamine (c) may be therefore considered part of the hypothalamus 2. The pituitary stalk (a) connects the pituitary gland to the brand 3. The infundibular process (Par nervosa or neural lobe) (a) secretes the hormones of the posterior pituitary Hormones of the Posterior Pituitary - Antidiuretic hormone (ADH) also called arginine vasopressin - Controls of plasma osmolality - Acts to increase the permeability of renal collecting ducts - increasing permeability leading to increase in water reabsorption and production of more concentrated urine - Called vasopressin because in extremely high doses it does cause vasoconstriction and a resulting increase in arterial blood pressure - Regulated primarily by the osmoreceptors of the hypothalamus - ADH secretions is increased by changes in intravascular volume. - Mechanoreceptors in the left atrium and in the caroticd and aortic arches. -ADH secretion decreases with a decrease in plasma osmolality, and increase in intravascular volume, hypertension, estrogen, progesterone, Angiotensin II, and alcohol ingestion - Oxytocin - primarily responsible for contractions of the uterus and milk ejection in lactating women - has an antidiuretic effect similar to that of ADH - studied more in women than men - used to induce uterine contractions - naturally more pominant toward the end of labor thought to enhance the effectiveness of contractions and promote delivery of the placenta and to prevent excessive post-partum bleeding - Peptide hormones are similar in structure differing by only two amino acids - Posterior pituitary can be seen as storage and releasing site for hormones synthesized in the hypothalamus Hormones of the Anterior Pituitary - Two main cell types 1. Chromophobes - nonsecretory 2. Chromophils - secretory cells of the adenohypophysis - Tropic hormones secreted by the anterior pituitary include ACTH, melanocyte-stimulating hormone (MSH), LH, GH, prolactin, FSH, and TSH - Regulation of the anterior pituitary hormones is achieved by: 1. feedback of hypothalamic releasing/ inhibitory hormones and factors 2. feedback from target gland hormones 3. direct effects of neurotransmitters. Thyroid and Parathyroid Glands Thyroid Gland - located in the neck just below the larynx, produces hormones that control metabolic rate processes throughout the body - composed of 2 lobes on either side of the trachea and inferior to the thyroid cartilage - joined by the isthmus - which crosses the anterior surface of the trachea and larynx at the cridoid cartilage - composed of follicles - follicular cells that surround a viscous substance called colloid - Acetycholine, catecholamines, and other peptides directly affect secretory activity of the follicular cells and thyroid blood flow. - C-cells secrete various polypeptides including calcitonin and somatostatin - Calcitonin (throcalcitonin) - acts to lower serum calcium levels by inhibition of bone-resorbing osteoclasts. High levels of calcitonin are required for these effects, and deficiencies of calcitonin do not lead to hypocalcemia Regulation of Thyroid Hormone Secretion - Thyroid hormone is regulated through a negative-feedback loop involving the hypothalamus , the anterior pituitary, and the thyroid gland - Thyrotropin-releasing hormone (TRH) is stored and synthesized in the hypothalamus. - TRH is released into the hypothalamic-pituitary portal system and circulates to the anterior pituitary, where it stimulates TSH. TRH is increased with exposure to cold, stress, and decreased levels of thyroxine - TSH is a glycoprotein hormone synthesized and stored within the anterior pituitary - The effects of TSH on the thyroid include 1. immediate increase in the release of stored thyroid hormones 2. increase in iodide uptake and oxidation 3. increase in TH synthesis 4. increase in the synthesis and secretion of protaglandins by the thyroid Synthesis of Thyroid Hormone - Thyroid Hormone Synthesis 1. Uniodinated thyroglobulin is produced by endoplasmic reticulum of follicular cells 2. Tyrosine is incorporated into the thyroglobulin as it is synthesized 3. Iodide is actively transferred from the blood into the colloid by carried proteins - active transport - iodide trap is efficient at locating trace amounts of iodide 4. Iodide attaches to tyrosine within the thyroglobulin molecule 5. Coupling of iodinated tyrosine forms thyroid hormones - T3 and T4 formation 6. Thyroid hormones are stored attached to thyroglobulin within the colloid until it is released into the circulation - TH affects many body tissues, primarily by affecting growth and maturation of tissues. Similar to some steroid hormones, thyroid hormones bind to intracellular receptors complexes and then influence the genetic expression of specific proteins Parathyroid Glands - parathyroid glands are located near the posterior side of the thyroid - function to control calcium levels in the blood - two pair located behind the upper pole of the thyroid gland and behind the lower pole - parathyroid hormone (PTH) is regulated primarily by the level of ionized plasma calcium, although how these regulatory mechanisms work is not precisely clear. - calcium also increase intraparathyroid destruction of PTH but does not affect the rate of PTH synthesis - Magnesium and phosphate levels also affect PTH secretion. Hypomagnesemia decreases PTH secretion leading to hypocalcemia. - PTH is secreted into the circulatory system unbound and attaches to plasma membrane receptors at the target cell - PTH acts directly on bone and on the kidneys to regulate serum calcium levels - PTH decreases proximal tubule reabsorption of bicarbonate. - PTH stimulates the synthesis of biologically active form of vitamin D, a potential stimulator of calcium and phosphate absorption in the intestine Endocrine Pancreas - the pancreas is both and endocrine gland that produces hormones and an exocrine gland that produces digestive enzymes - responsible for much of the metabolism that occurs within the body - located behind the stomach, between the spleen and duodenum - houses islets of Langerhans -secretion of glucagons and insulin - alpha cells - secrete glucagons - beta cells- secrete insulin - delta cells- secrete somatostatin and gastrin - parasympathetic nervous system stimulates hormonal secretion - sympathetic nervous system inhibits secretions Insulin - insulin secretion is promoted by increased blood levels of glucose, amino acids (arginine and lysine), serum fat free acids, and gastrointestinal hormones, and by parasympathetic stimulation of the beta cell - insulin secretion diminishes in response to hypoglycemia, high levels of insulin (negative feedback), and sympathetic stimulation of the alpha cells -- prostaglandin also inhibits insulin secretion - insulin facilitates the uptake of glucose into the cells within the body - anabolic hormone that promotes the synthesis of proteins, lipids, and nucleic acids -major sites of insulin-promoted synthesis include; the liver, muscle and adipose tissue - net effect of insulin is to stimulate cellular metabolism - facilitates the intracellular transport of potassium Glucagon - produced in the alpha cells of the pancreas and by a number of cells in the GI tract - primarily acts in the liver and increases blood glucose levels by stimulating glycogenolysis and gluconeogenesis - also acts as an antagonist to insulin - stimulates lipolysis - ketogenic effect caused by metabolism of free fatty acids in liver Somatostatin - produced by the delta cells - essential in carbohydrate, fat, and protein metabolism - little is known about pancreatic somatostatin - likely involved in the regulation of alpha and beta cell function - inhibits both glucagon and insulin secretion - prevent excess secretion of insulin by pancreas Adrenal Glands - paired, pyramid-shaped organs located behind the peritoneum and close to the upper pole of each kidney -each gland is surrounded by a capsule, embedded in fat, well supplied with blood - adrenal cortex divided into 3 zones - zona glomerulosa - outer layer -production of mineralocorticoid aldosterone - zona fasciculate - middle layer - zona reticularis - inner layer - secrete other mineralocorticoids, adrenal androgens, estrogens, glucocorticoids - adrenal medulla - secretes the catecholamines epinephrine (adrenaline) and norepinephrine Adrenal Cortex - adrenal cortex secretes several steroid homones - cells must be stimulated by hypophysiotropic hormone - adrenocorticotropic hormone (ACTH) for cholesterol to be used in steroidogenisis Glucocorticoids - have metabolic, anti-inflammatory, and growth suppressing effects - influence of level of awareness and sleep patterns - glucocorticoid- refers to those steroid hormones that have direct effects on carbohydrate metabolism - glucocorticoids act primarily to stimulate glucose formation and synthesis of enzymes that mediate glucocorticoid effects - affecting protein breakdown - glucocorticoids act at several sites to influence immune and inflammatory reactions - depressing proliferation of T lymphoctes - decreasing natural killer cell activity - promotes microphage phagocytosis - suppresses the synthesis, secretion, and actions of chemical mediatiors involved in the immune response - stimulate anti-inflammatory cytokines - suppress inflammatory response - blocking phospholipase A2 - synthesis of prostaglandins - thromboxanes - leukotrienes - inhibit inflammatory gene expression - increasing circulating erythrocytes - leading to polycythemia - increasing appitite - promotion of fat deposits in the face and cervical area - increasing uric acid excretion - decrease serum calcium levels - potentates the effects of catecholamines, thyroid hormone, and GH on adipose tissue - metabolite of cortisonl acts like barbiturate and depresss nerve cell function to brain - Cortisol is regulated primarily by the hypothalamus and the anterior pituitary gland - Factors involved in regulation the secretion of ACTH 1. High circulating levels of cortisol and synthetic glucocorticoid suppress both CRH and ACTH - low levels of cortisol stimulate their secretion 2. Diurnal rhythms affect ACTH and cortisol levels ACTH peaks 3-5 hrs after sleep begins ACTH declines throughout the day 3. Stress has been shown to increase ACTH secretion leading to increase cortisol levels Mineralocorticoids: Aldosterone - directly affect ion transport by epithelial cells, causing sodium retention and potassium and hydrogen loss - Aldosterone is the most potent of the naturally occurring mineralocorticoids and acts to conserve sodium by increasing the activity of the sodium pump of the epithelial cells - Aldosterone synthesis and secretion is stimulated by Angiotensin II. The conversion of angiotension I to angiotensis II in stimulated by the enzyme angiotensisn I - converting enzyme - renin secretion is stimulated primarily by sodium and water depletions or a diminished effective blood volume or increased potassium - 50-75% of the secreted aldosterone binds to plasma proteins, including albumin, transcortin and an ά2acid glycoprotein (AAG) - in the kidneys aldosterone primarily acts on the epithelial cells of the nephron collecting duct to increase sodium ion reabsorption and increase potassium and hydrogen ion excretion. Adrenal Estrogens and Androgens - estrogen secretion by the normal adrenal cortex is so minimal as to be considered physiologically unimportant - secretions of androgens - such as testosterone - increased capacity for peripheral conversion of adrenal androgens to estrogens occur in particular cases including ageing, obesity, liver, disease, and hyperthyroidism -ACTH appears to be the major regulator rather than the gonadotropins Adrenal Medulla - Chromaffin cells (pheochomocytes) are the cells of the adrenal medulla - Major products of chromaffin cells - catecholamines epinephrine (adrenalin) and norepinephrine, although the medulla is only a minor source of norepinephrine - Epinephrine is about 10 times more potent than norepinephrine in producing direct metabolic effects - Secretion is increased by ACTH and glucocorticoids - the catecholamines apparently exert a direct inhibiting influence on their own secretion by decreasing the formation of the reate-limiting enzyme tyrosine hydroxylase - Catecholamines may bind t various target cells, may be taken up by neurons for storage in new cytoplasmic granules, or may be metabolically inactivated and excreted in the urine - “fight or flight” response Neuroendocrine Response to Stressors - the endocrine system acts together with the nervous system to respond to stressors -- the integrated response to stressors also includes the immune system - hypothalamus receives input from a variety of areas within the brain and ultimately directs the neuroendocrine response to stress thourgh the actions of corticotrophin-releasing hormone (CRH), the locus ceruleus-norepinephrine autonomic (sympathetic) nervous system, and the pituitary-adrenal axis. Tests of Endocrine Function - Measurement of hormone level is accomplished by radioimmunoassay, by enzyme-linked immunosorbent assey, and less commonly by bioassay - Radiouimmunoassay (RIA) is a technique for measuring the minute quantities of hormones in the blood. - Enzyme-linked immunosorbent assays (ELISAs) also are used to determine circulating hormone levels. Similar to RIA but less expensive and easier to conduct - Bioassay involves the use of graded doses of hormone in a reference preparation and then comparison of the results with an unknown sample. The most commonly used clinical test - Major problems in evaluating the endocrine system include: 1. complexity of the clinical presentation because of multiple organ system involvement 2. nonspecific nature of complaints frequently associated with endocrine dysfunction 3. inappropriate us of laboratory test interpretations. Aging and the Endocrine System Theories About Effects of Aging - Cellular Damage - adverse cellular conditions that produce the biologic effects associated with aging - Stress & Adaption - suggest that body structures wear out from overuse or are not longer able to adapt to the cumulative effects of physiologic stress - Programmed Change - concerned with genetic control of cell functions; cells genetically programmed to secrete hormones for a prescribed period of time - Dynamic Equilibrium - the endocrine may be affected by altered secretion of neroutransmitters within certain areas of the brain, affecting hypothalamic and pituitary function Effects of Aging on Specific Glands Thyroid Gland -Structurally some glandular atrophy and fibrosis occurs with nodularity and increasing inflammatory infiltrates - Changes relative to thyroid hormone and its function are more difficult to assess - Evidence supports the following age-related changes Overall TSH secretion is diminished Responsiveness of plasma TSH concentration to TRH administration is reduced (men) T4 secretion and turnover are decreased Plasma levels of T3 decline (men) Hypothroidism is seen with increasing frequency with increased age Parathyroid Glands - PTH secretion proposed to explain alterations in calcium homeostasis that have been noted in older adults - Calcium intake, especially in women, tends to decrease with aging and may contribute to osteoporosis - Older adults show decreased intestinal adaptation to variations in calcium intake. Hyperparathyroidism may be secondary to calcium malabsorptiona and hypocalcemia with increased bone remodeling that results in cortical bone thinning and porosity. - The decrease in calcium intake, and age-related decrease in circulating vitamin D, and a blunted response of older persons to PTH may explain these changes seen in aging Adrenal Glands - The adrenal cortex loses some weight and has more fibrous tissue after age 50. - Metabolic clearance of cortisole decreases with an age-related decline in liver and kidney function - Less cortisol appears to be used by the body when aging is accompanied by a loss of lean body mass Posterior Pituitary - Hyponatremia is a common finding in older persons, it appears related to changes in renal function rather than to ADH- related mechanisms - ADH secretion is augmented when stimulated by changes in osmotic concentrations. whereas baroreceptor-medicatied ADH secretion is reduced Anterior Pituitary - Increase in fibrosis, focal necrosis, iron deposits, and micradenoma formation and moderate decrease in size - Growth hormone may be reduced in the elderly and accounts for increased visceral fat, decrease in lean body mass and decreased bone density Summary of Hormones