* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Changes in spatial extent and peak double optical density of human
Spectral density wikipedia , lookup
Optical amplifier wikipedia , lookup
Fiber-optic communication wikipedia , lookup
Vibrational analysis with scanning probe microscopy wikipedia , lookup
Astronomical spectroscopy wikipedia , lookup
Preclinical imaging wikipedia , lookup
Photon scanning microscopy wikipedia , lookup
Ultrafast laser spectroscopy wikipedia , lookup
Nonlinear optics wikipedia , lookup
Optical rogue waves wikipedia , lookup
Anti-reflective coating wikipedia , lookup
Ellipsometry wikipedia , lookup
Nonimaging optics wikipedia , lookup
Hyperspectral imaging wikipedia , lookup
Super-resolution microscopy wikipedia , lookup
Magnetic circular dichroism wikipedia , lookup
Silicon photonics wikipedia , lookup
Optical tweezers wikipedia , lookup
Retroreflector wikipedia , lookup
Passive optical network wikipedia , lookup
3D optical data storage wikipedia , lookup
Optical coherence tomography wikipedia , lookup
Chemical imaging wikipedia , lookup
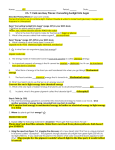
A. M. G. Baptista and S. M. C. Nascimento Vol. 31, No. 4 / April 2014 / J. Opt. Soc. Am. A A87 Changes in spatial extent and peak double optical density of human macular pigment with age António M. G. Baptista* and Sérgio M. C. Nascimento Center of Physics, University of Minho, Campus de Gualtar, 4715-303 Braga, Portugal *Corresponding author: [email protected] Received September 30, 2013; accepted December 6, 2013; posted December 13, 2013 (Doc. ID 198611); published January 21, 2014 The purpose of the present work was to estimate the changes in spatial distribution and optical density of macular pigment (MP) with age. A fundus imaging system with high spatial and spectral resolution was adapted to form an indirect ophthalmoscope. The double optical density at 490 nm of the MP as a function of the location in the retina was obtained for 33 healthy subjects (ages: 21–60 years). There was an increase in spatial extent and decrease in double optical density with age. Furthermore, the spatial distribution of MP showed central areas with irregular shapes and a tendency toward asymmetry. © 2014 Optical Society of America OCIS codes: (330.4460) Ophthalmic optics and devices; (330.6100) Spatial discrimination; (330.6180) Spectral discrimination; (330.7323) Visual optics, aging changes; (330.7327) Visual optics, ophthalmic instrumentation. http://dx.doi.org/10.1364/JOSAA.31.000A87 1. INTRODUCTION The macular pigment (MP) is a yellow pigment found in the human fovea in both the inner and outer layers of the retina, and located along the axons of the cone photoreceptors [1]. It is mainly composed of two xanthophylls, lutein and zeaxanthin [2]. MP has a peak absorption wavelength at 460 nm but nearly no absorption of light at wavelengths longer than 530 nm [3,4]. The function of MP is not fully understood but appears to be fundamental for maintaining normal retinal function. It is thought to play an important role in the protection of photoreceptors from short-wavelength radiation damage and as an antioxidant [5]. It may serve to reduce the effects of chromatic aberration and light scatter on visual performance [6]. There is also evidence that low levels of MP may be related to a higher risk of developing age-related macular degeneration [7–9]. Macular pigment optical density (MPOD) has been demonstrated to increase after diets rich in zeaxanthin and lutein [10–16]. Measurements of MPOD as a function of age have been carried out using different techniques. Some studies using fundus reflectance spectroscopy found that MPOD for older subjects was higher than that for younger subjects [16–18] while others have found no age-dependence [19–21]. Similar variability has also been obtained in psychophysical studies, where an agerelated decline was found in some studies [8,22–25], but not others [15,26,27]. The effect of age on MP spatial distribution has been recognized [16,19]; however, this has generally not been analyzed as an important variable of MP. The precise characterization of the optical density of MP and, in particular, its spatial extent, is still an open issue. The amount and distribution of MP have been assessed by fundus reflectance spectroscopy. This optical approach is based on models considering the physical interactions (e.g., absorption, scattering, and reflectance) between light and ocular structures as a function of wavelength [28,29]. The fundus 1084-7529/14/040A87-06$15.00/0 imaging systems based on lasers, such as the scan laser ophthalmoscope, or wavelength filters, such as a beam splitter combined with narrow band-path filters, are restricted to the number of wavelengths that can be used [11,30]. The multispectral imaging system may overtake this restriction because the filter can be tuned to a wide range of wavelengths. Several groups in the last decade have used this technique to study retinal structures, including macular pigment [31,32]. The main purpose of the present work was to estimate the changes in spatial distribution and peak double optical density of MP with age from measurements made with a high spatial resolution, multispectral system, adapted to an indirect ophthalmoscope. 2. METHODS A. Apparatus The imaging system was based on an indirect ophthalmoscope, adapted with a xenon lamp coupled to a fast tunable liquid–crystal filter (VariSpec, model VS-VIS2-10HC-35-SQ, Cambridge Research & Instrumentation, Inc., MA, USA), and with a low-noise Peltier-cooled digital camera (Hamamatsu, model C4742-95-12ER). The lamp was a 150 W xenon short-arc lamp (Hamamatsu, type L2274) with a stable light emission from 400 to 800 nm, and was provided with a stabilized power supply (Hamamatsu, type C2577) for a stable light flux output. The liquid–crystal filter could be electronically tuned to any wavelength in the range from 400 to 720 nm with a spectral resolution of 1 nm, and had a nominal FWHM of 10 nm at 550 nm. The CCD camera had a spatial resolution of 1344 H × 1024 V pixels, 6.45 μm × 6.45 μm pixel size, 12 bit output. A 2 × 2 binning acquisition mode was used for increased sensitivity. The area of the retina illuminated by the system was of about 20 deg visual angle. The light uniformity was tested against a BaSO4 surface and the variations were less than 12% between the extremes © 2014 Optical Society of America A88 J. Opt. Soc. Am. A / Vol. 31, No. 4 / April 2014 A. M. G. Baptista and S. M. C. Nascimento of the observation field, which was about 11 deg. The estimated spatial resolution at the retina was about 1 min ×1 min. The light reflected at the cornea and lens was minimized by separating the entrance from the exit pupil of the system. B. Procedure Subjects were dilated with tropicamide and phenylephrine to obtain pupil diameters larger than 7 mm. To reduce the effect of the visual pigments as a variable parameter, the fundus was bleached immediately before image acquisition using a bright white light source (halogen lamp with a correlated color temperature of 3150 K) of 5.57 log and lasting 80 s. This bleaching procedure removes more than 90% of the visual pigments [33]. Pixels were converted to visual angle using pairs of images, acquired when the subject fixated at target points separated by 2 deg. For each subject, two images of the retina were sequentially acquired, corresponding to retinal illuminations with monochromatic light of 490 and 540 nm. Let each of these images be represented by Sλ, where λ is the wavelength of the illumination. The second peak of MPOD (at about 490 nm) was selected instead of the first (at about 460 nm), to minimize the effect of eye movement by reducing total acquisition time (by lowering ocular media absorption) to about 2 s. The remaining effects of small eye movements were compensated for by aligning the retinal images obtained for the two wavelengths, with retinal blood vessels used as references. For each Sλ, corresponding white S w λ and dark S d λ references were also acquired. S w λ was obtained using an artificial eye with a power of 60 diopters and with its fundus coated with fresh BaSO4 . S d λ was obtained with the same device coated with a dark coating. The three images were acquired with the same exposure times for each wavelength. [19], was used here to obtain the double-passed optical density of MP δ at 490 nm. The pigments of the absorbing layers correspond to ocular media, macular pigment, and melanin with optical densities D1 , D2 , D3 , respectively, and the reflectance layer corresponds to the retinal pigment epithelium (RPE) with reflectance r and assumed independent of the wavelength and retinal position. The contributions of the ocular media were also assumed independent of the retinal position. Applying the Beer Lambert law to the simplified model, the eye reflectance Rλ can be expressed: Rλ r × 10−2D1 λ2D2 λ2D3 λ : Applying Eq. (2) to 490 and 540 nm, assuming D2 540 0 and defining 2D2 490 as δ: δ log10 D. Computations The reflectance factor of each pixel of the retina region was estimated by Rf λ Sλ − S d λ : S w λ − S d λ 1 1 − β log10 A; R490 R540 (3) where β D3 490 ; D3 540 (4) and D 490 A β− 1 2D1 540 1 − βlog10 r: D1 540 (5) As the reflectance factor Rf differs from the reflectance R by a multiplicative constant k δ log10 C. Subjects A total of 33 Caucasian subjects were selected from a group of volunteers. The exclusion criteria were narrow angle between cornea and iris, tonometry repeatedly over 22 mmHg, ocular diseases, heart problems, refractive errors higher than 3 (positive or negative) diopters or astigmatism higher than 1.5 diopters, cloudy ocular media, fixation or behavioral problems, ptosis, food supplements, particular diets such as vegetarian, and smokers. The 33 subjects were divided into 3 groups: group A with 12 subjects (10 female and 2 male) with a mean age of 22.3 years and range of 21–25 years; group B with 12 subjects (2 female and 10 male) with a mean age of 36.0 years and range of 30 to 45 years; and group C with 9 subjects (6 female and 3 male) with a mean age of 55.2 years and range of 50 to 60 years. Informed consent was obtained from all participants and the research was conducted according to the guide lines promoted by the Declaration of Helsinki. (2) 1 1 − β log10 A B; Rf 490 Rf 540 (6) where 1 1 B log10 − β log10 : k k (7) Taking into account the reflectance factor obtained in the peripheral retina x0 ; y0 , where δ 0, and assuming that A and B are independent of the retinal position, then δx;y log10 1 1 − β log10 Rf x;y 490 Rf x;y 540 − log10 1 Rf x0 ;y0 490 − β log10 1 Rf x0 ;y0 540 ; (8) where β is assumed to be 1.12 [34]. The spatial distribution δx;y was derived for each pixel using Eq. (8). For Rf x0 ;y0 , the average over an area of about 0.5 deg2 centered on a point at an eccentricity of about 5 degrees, where MPOD is negligible, was used [35–37]. To minimize pixel noise, a low pass filter was applied to the data resulting from Eq. (8). (1) The model of van Norren and Tiemeijer [28], simplified by considering three absorbing layers and one reflective layer 3. RESULTS Figure 1 shows macular pigment distribution for two subjects. The retinal area represented is about 11 deg. Qualitatively, it A. M. G. Baptista and S. M. C. Nascimento Fig. 1. Macular pigment distribution for two subjects (S 1 and S 2 ). can be seen that the distributions show higher values in a central area, declining to around zero in the periphery; also, the distributions are asymmetric and have central areas with irregular shapes. It can also be seen that low values extend laterally over the limits of the observation field. Data for the other observers show similar features. Vol. 31, No. 4 / April 2014 / J. Opt. Soc. Am. A A89 The mean peak double optical density (optical density corresponds to 0.5 × δ) of MP δ standard deviation was 0.23 0.07, 0.25 0.07, and 0.16 0.05, ranging from 0.13– 0.40, 0.16–0.36, and 0.08–0.22 for groups A (the youngest), B and C (the oldest), respectively. After the ANOVA oneway test (df 2, F 6.253, p 0.005), multiple comparisons (Tukey) between groups showed statistically significant differences between the groups A and C (p 0.049) and groups B and C (p 0.004). To characterize the spatial distribution of the MP, the FWHM of horizontal and vertical profiles was computed for each subject. To specify further the asymmetries of the distributions, a rectangle of a · b dimensions enclosing the section at half-maximum was obtained. Figure 2, resulting from connecting 377 points between 3 deg with straight lines, shows the vertical and horizontal profiles for double optical density and section at half-maximum, within the rectangle a · b for the two subjects. Table 1 lists mean values of vertical and horizontal FWHM, the standard deviations (SD), and maximum– minimum range for each age group. Table 2 shows similar data for a and b. For all age groups, considerable inter-individual variability (min, max, and SD) was found both in the values of the FWHM and in the sizes a and b. On the other hand, the distributions Fig. 2. Vertical and horizontal profiles and respective section at half-maximum, within the rectangle a · b for two subjects (S 1 and S 2 ). A90 J. Opt. Soc. Am. A / Vol. 31, No. 4 / April 2014 A. M. G. Baptista and S. M. C. Nascimento Table 1. FWHM (deg visual angle) Data for the Three Age Cohorts Group Mean Min Max SD FWHM (horizontal meridian) 1.75 3.40 0.47 1.27 3.80 0.69 2.29 5.01 0.88 FWHM (vertical meridian) 2.30 1.73 2.81 0.36 2.19 0.96 3.10 0.62 3.14 1.58 4.54 0.97 A B C 2.64 2.55 3.26 A B C ANOVA df 2 F 3.139 p 0.058 df 2 F 6.092 p 0.006a Statistically significant differences (p < 0.05) a Table 2. MP Distribution (deg visual angle) in Terms of Enclosing Rectangle a · b for the Three Age Cohorts Group Mean A B C 2.75 2.72 3.65 A B C 2.48 2.35 3.39 Min Max a (horizontal) 1.80 3.54 1.27 3.84 2.56 5.32 b (vertical) 1.80 3.11 1.04 3.46 2.25 4.83 SD ANOVA 0.53 0.74 0.94 df 2 F 5.083 p 0.013a 0.45 0.69 0.92 df 2 F 6.742 p 0.004a Statistically significant differences (p < 0.05) a are clearly asymmetric, with larger extent in the horizontal direction than in vertical direction. More than 87% of the subjects present a (horizontal) larger than b (vertical). Inter-group comparisons, after the ANOVA one-way test (Tables 1 and 2), showed statistically significant differences between groups A and C and between groups B and C, for vertical FWHM and sizes a and b (Tukey, all p ≤ 0.024). 4. DISCUSSION The optical and antioxidant properties of MP play an important role in maintaining the health and function of macula through life. Quantification of MP levels and distributions might help, for example, to identify individuals potentially at risk for visual disability from age-related macular degeneration [5]. This work measured MP distributions for three age groups using high spatial resolution. Large inter-subject variability in terms of peak density and spatial distribution was found. Even so, there were significant differences in peak densities at 490 nm between the oldest group and the other two groups, A and B, with the former showing smaller values. Moreover, a clear asymmetry was found for the horizontal and vertical directions, with a larger extent in the horizontal direction. Generically, the effect of aging was found significant in both directions, revealing a larger spatial extent for the older group. Studies of macular pigment using fundus reflectance spectroscopy have produced values for MPOD (MPOD 0.5 × δ) varying from 0.13 [38] to 0.54 [29]. High inter-study variability is also found with psychophysical and auto-fluorescence techniques, where values from 0.21 [39] to 0.87 [40] and from 0.22 [41] to 0.48 [17], have been recorded, respectively. The range of values obtained in this work are similar to other reflectance studies [17,19,41,42] and, in particular, to a recent study using a similar technique, which obtained 0.15 0.05 for 6 subjects with a mean age 32.8 12.1 [32] (it should be emphasized that computations here were carried out to obtain MPOD at 490 nm rather than at the usual 460 nm, where the 490 nm has values about 17% less than that at 460 nm [4]; thus, the corresponding scaling has to be applied for comparison). A decrease in MPOD with age was also found by a previous study [41] using reflectance spectroscopy; however, in comparing the reflectance data with the auto-fluorescence data, they attributed this decrease to reflectance artifacts caused by the lens and the inner limiting membrane. Chen and colleagues [19], using reflectance spectroscopy and the same optical model as that used here, did not find any significant variation in MPOD for older subjects. Similar conclusions were obtained by Berendschot and van Norren [21]. On the other hand, according to Pipis and colleagues, also using reflectance spectroscopy, MPOD appears to increase with age [16]. The values for the FWHM (horizontal meridian) obtained by reflectance spectroscopy ranged from about 2.4 deg [36,38] to 3.2 deg [19]. The mean value obtained in this work of 2.8 deg is in good agreement with these studies. The present work showed that, in more than 87% of the subjects, the spatial extent of MP in the horizontal meridian is larger than in the vertical meridian. A slight tendency toward this asymmetry was also found by others [36,43]; although not by Bour and colleagues [38], who found no substantial deviation from circular symmetry in young subjects. In this study, the asymmetry in MP spatial distribution was further demonstrated by an irregular topography and by the fact that, for some subjects, low values of δ extend laterally over the limits of the observation field. Furthermore, macular pigment appears to form more eccentric profiles with increased age [16]. The differences in spatial distribution between the oldest group and the other two groups, corresponding to an increase in spatial extent with age, were also found by Chen and colleagues [19] for the horizontal meridian. Possible factors other than age effects for these changes, both in the amount and distribution between studied populations, are diet and lifestyle [44,45]. The comparison between the fovea and peripheral retina minimizes the effect of the background noise and avoids the use of pigment density and RPE reflectance values from the literature. However, MPOD seems to have small values at 6–8 deg, which could contribute to an underestimation of the MPOD and the FWHM, since it was assumed to be zero at 5 deg [46,47]. The model applied here did not consider the effect of pre-retinal and intra-retinal scatter, which again might underestimate the MPOD and the FWHM [48]. However, the increase in spatial extent with age and the relation between MP distribution in the horizontal and vertical meridians is independent of these approximations. The remaining visual pigment and possible light gradients in fundus illumination could also introduce artifacts not considered in the present study. Another factor that could influence the results from fundus reflectance spectroscopy is that longer wavelengths penetrate the retinal tissue to greater depths than do shorter wavelengths [49,50]; therefore, the MP could not be A. M. G. Baptista and S. M. C. Nascimento completely revealed by short wavelength light. Thus, using 490 nm instead of 460 nm for imaging could be more effective for MP study. ACKNOWLEDGMENTS This work was supported by the Center of Physics of Minho University, Braga, Portugal. The empirical data analyzed in this paper was reported in part at the 18th Symposium of International Colour Vision Society. We are grateful to Alberto J. Díaz-Rey for clinical assistance. REFERENCES 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. D. M. Snodderly, P. K. Brown, F. C. Delori, and J. D. Auran, “The macular pigment. 1. absorbance spectra, localization, and discrimination from other yellow pigments in primate retinas,” Invest. Ophthalmol. Vis. Sci. 25, 660–673 (1984). R. A. Bone, J. T. Landrum, and S. L. Tarsis, “Preliminary identification of the human macular pigment,” Vis. Res. 25, 1531–1535 (1985). R. A. Bone, J. T. Landrum, and A. Cains, “Optical-density spectra of the macular pigment in vivo and in vitro,” Vis. Res. 32, 105–110 (1992). G. Wyszecki and W. S. Stiles, eds., Color Science: Concepts and Methods, Quantitative Data and Formulae (Wiley, 1982). P. S. Bernstein, F. Khachik, L. S. Carvalho, G. J. Muir, D. Y. Zhao, and N. B. Katz, “Identification and quantitation of carotenoids and their metabolites in the tissues of the human eye,” Exp. Eye Res. 72, 215–223 (2001). V. M. Reading and R. A. Weale, “Macular pigment and chromatic aberration,” J. Opt. Soc. Am. 64, 231–234 (1974). D. M. Snodderly, “Evidence for protection against age-related macular degeneration by carotenoids and antioxidant vitamins,” Am. J. Clin. Nutr. 62, 1448S–1461S (1995). J. M. Nolan, J. Stack, O. O’Donovan, E. Loane, and S. Beatty, “Risk factors for age-related maculopathy are associated with a relative lack of macular pigment,” Exp. Eye Res. 84, 61–74 (2007). S. Kaya, G. Weigert, B. Pemp, S. Sacu, R. M. Werkmeister, N. Dragostinoff, G. Garhoefer, U. Schmidt-Erfurth, and L. Schmetterer, “Comparison of macular pigment in patients with age-related macular degeneration and healthy control subjects—a study using spectral fundus reflectance,” Acta Ophthalmol. 90, e399–e403 (2012). B. R. Hammond, E. J. Johnson, R. M. Russell, N. I. Krinsky, K. J. Yeum, R. B. Edwards, and D. M. Snodderly, “Dietary modification of human macular pigment density,” Invest. Ophthalmol. Vis. Sci. 38, 1795–1801 (1997). T. Berendschot, R. A. Goldbohm, W. A. A. Klopping, J. van de Kraats, J. van Norel, and D. van Norren, “Influence of lutein supplementation on macular pigment, assessed with two objective techniques,” Invest. Ophthalmol. Vis. Sci. 41, 3322–3326 (2000). H. H. Koh, I. J. Murray, D. Nolan, D. Carden, J. Feather, and S. Beatty, “Plasma and macular response to lutein supplement in subjects with and without age-related maculopathy: a pilot study,” Exp. Eye Res. 79, 21–27 (2004). W. Schalch, W. Cohn, F. M. Barker, W. Kopcke, J. Mellerio, A. C. Bird, A. G. Robson, F. F. Fitzke, and F. J. G. M. van Kuijk, “Xanthophyll accumulation in the human retina during supplementation with lutein or zeaxanthin—the LUXEA (LUtein Xanthophyll Eye Accumulation) study,” Arch. Biochem. Biophys 458, 128–135 (2007). R. A. Bone, J. T. Landrum, Y. Cao, A. N. Howard, and F. Alvarez-Calderon, “Macular pigment response to a supplement containing meso-zeaxanthin, lutein and zeaxanthin,” Nutr. Metab. 4, 12–20 (2007). A. Iannaccone, M. Mura, K. T. Gallaher, E. J. Johnson, W. A. Todd, E. Kenyon, T. L. Harris, T. Harris, S. Satterfield, K. C. Johnson, S. B. Kritchevsky, and A. B. C. S. Health, “Macular pigment optical density in the elderly: findings in a large biracial midsouth population sample,” Invest. Ophthalmol. Vis. Sci. 48, 1458–1465 (2007). Vol. 31, No. 4 / April 2014 / J. Opt. Soc. Am. A A91 16. A. Pipis, E. Touliou, and A. J. Augustin, “Macular pigment optical density in a Central European population,” Ophthalmic Surg. Lasers Imaging Retina 44, 260–267 (2013). 17. F. C. Delori, D. G. Goger, B. R. Hammond, D. M. Snodderly, and S. A. Burns, “Macular pigment density measured by autofluorescence spectrometry: comparison with reflectometry and heterochromatic flicker photometry,” J. Opt. Soc. Am. A 18, 1212–1230 (2001). 18. T. Berendschot, J. J. M. Willemse-Assink, M. Bastiaanse, P. de Jong, and D. van Norren, “Macular pigment and melanin in age-related maculopathy in a general population,” Invest. Ophthalmol. Vis. Sci. 43, 1928–1932 (2002). 19. S. F. Chen, Y. Chang, and J. C. Wu, “The spatial distribution of macular pigment in humans,” Curr. Eye Res. 23, 422–434 (2001). 20. T. Berendschot and D. van Norren, “Objective determination of the macular pigment optical density using fundus reflectance spectroscopy,” Arch. Biochem. Biophys. 430, 149–155 (2004). 21. T. T. Berendschot and D. van Norren, “On the age dependency of the macular pigment optical density,” Exp. Eye Res. 81, 602–609 (2005). 22. B. R. Hammond, B. R. Wooten, and D. M. Snodderly, “Density of the human crystalline lens is related to the macular pigment carotenoids, lutein and zeaxanthin,” Optom. Vis. Sci. 74, 499– 504 (1997). 23. B. R. Hammond and M. Caruso-Avery, “Macular pigment optical density in a southwestern sample,” Invest. Ophthalmol. Vis. Sci. 41, 1492–1497 (2000). 24. S. Beatty, I. J. Murray, D. B. Henson, D. Carden, H. H. Koh, and M. E. Boulton, “Macular pigment and risk for age-related macular degeneration in subjects from a Northern European population,” Invest. Ophthalmol. Vis. Sci. 42, 439–446 (2001). 25. J. Yu, E. J. Johnson, F. Shang, A. Lim, H. Zhou, L. Cui, J. Xu, T. Snellingen, X. Liu, N. Wang, and N. Liu, “Measurement of macular pigment optical density in a healthy Chinese population sample,” Invest. Ophthalmol. Vis. Sci. 53, 2106–2111 (2012). 26. J. S. Werner, S. K. Donnelly, and R. Kliegl, “Aging and human macular pigment density. Appended with translations from the work of Max Schultze and Ewald Hering,” Vis. Res. 27, 257–268 (1987). 27. R. A. Bone, J. T. Landrum, L. Fernandez, and S. L. Tarsis, “Analysis of the macular pigment by HPLC: retinal distribution and age study,” Invest. Ophthalmol. Vis. Sci. 29, 843–849 (1988). 28. D. van Norren and L. F. Tiemeijer, “Spectral reflectance of the human eye,” Vis. Res. 26, 313–320 (1986). 29. J. van de Kraats, T. Berendschot, and D. van Norren, “The pathways of light measured in fundus reflectometry,” Vis. Res. 36, 2229–2247 (1996). 30. S. H. Hardarson, A. Harris, R. A. Karlsson, G. H. Halldorsson, L. Kagemann, E. Rechtman, G. M. Zoega, T. Eysteinsson, J. A. Benediktsson, A. Thorsteinsson, P. K. Jensen, J. Beach, and E. Stefansson, “Automatic retinal oximetry,” Invest. Ophthalmol.Vis. Sci. 47, 5011–5016 (2006). 31. V. Nourrit, J. Denniss, M. M. Muqit, I. Schiessl, C. Fenerty, P. E. Stanga, and D. B. Henson, “High-resolution hyperspectral imaging of the retina with a modified fundus camera,” J. Fr. Ophtalmol. 33, 686–692 (2010). 32. A. A. Fawzi, N. Lee, J. H. Acton, A. F. Laine, and R. T. Smith, “Recovery of macular pigment spectrum in vivo using hyperspectral image analysis,” J. Biomed. Opt. 16, 106008 (2011). 33. M. Alpern, F. Maaseidv, and N. Ohba, “Kinetics of cone visual pigments in man,” Vis. Res. 11, 539–549 (1971). 34. W. Hunold and P. Malessa, “Spectrophotometric determination of melanin pigmentation of human ocular fundus in vivo,” Ophthalmic Res. 6, 355–362 (1974). 35. U. Stabell and B. Stabell, “Variation in density of macular pigmentation and in short-wave cone sensitivity with eccentricity,” J. Opt. Soc. Am. 70, 706–711 (1980). 36. P. E. Kilbride, K. R. Alexander, M. Fishman, and G. A. Fishman, “Human macular pigment assessed by imaging fundus reflectometry,” Vis. Res. 29, 663–674 (1989). 37. J. D. Moreland, A. G. Robson, N. Soto-Leon, and J. J. Kulikowski, “Macular pigment and the colour-specificity of visual evoked potentials,” Vis. Res. 38, 3241–3245 (1998). 38. L. J. Bour, L. Koo, F. C. Delori, P. Apkarian, and A. B. Fulton, “Fundus photography for measurement of macular pigment A92 39. 40. 41. 42. 43. 44. J. Opt. Soc. Am. A / Vol. 31, No. 4 / April 2014 density distribution in children,” Invest. Ophthalmol. Vis. Sci. 43, 1450–1455 (2002). T. A. Ciulla, J. Curran-Celantano, D. A. Cooper, B. R. Hammond, R. P. Danis, L. M. Pratt, K. A. Riccardi, and T. G. Filloon, “Macular pigment optical density in a Midwestern sample,” Ophthalmology 108, 730–737 (2001). P. L. Pease and A. J. Adams, “Macular pigment difference spectrum from sensitivity measures of a single cone mechanism,” Am. J. Optom. Physiol. Opt. 60, 667–672 (1983). H. Wustemeyer, A. Moessner, C. Jahn, and S. Wolf, “Macular pigment density in healthy subjects quantified with a modified confocal scanning laser ophthalmoscope,” Graef. Arch. Clin. Exp. 241, 647–651 (2003). F. C. Delori and K. P. Pflibsen, “Spectral reflectance of the human ocular fundus,” Appl. Opt. 28, 1061–1077 (1989). T. Berendschot and D. van Norren, “Macular pigment shows ringlike structures,” Invest. Ophthalmol. Vis. Sci. 47, 709–714 (2006). S. Richer, J. Devenport, and J. C. Lang, “LAST II: differential temporal responses of macular pigment optical density in patients with atrophic age-related macular degeneration to dietary A. M. G. Baptista and S. M. C. Nascimento 45. 46. 47. 48. 49. 50. supplementation with xanthophylls,” Optometry 78, 213–219 (2007). J. M. Stringham and B. R. Hammond, “Macular pigment and visual performance under glare conditions,” Optom. Vis. Sci. 85, 82–88 (2008). R. L. van der Veen, T. T. Berendschot, M. Makridaki, F. Hendrikse, D. Carden, and I. J. Murray, “Correspondence between retinal reflectometry and a flicker-based technique in the measurement of macular pigment spatial profiles,” J. Biomed. Opt. 14, 064046 (2009). M. L. Bieber and J. S. Werner, “The spatial distribution of human macular pigment,” in Vision Science and Its Applications, Vol. 1 of 1998 OSA Trends in Optics and Photonics (Optical Society of America, 1998), pp. 10–13. Y. Chang, F. L. Lee, S. J. Chen, and S. F. Chen, “Optical measurement of human retinal macular pigment and its spatial distribution with age,” Med. Phys. 29, 2621–2628 (2002). L. C. Norden, “Spectral reflectance photography of the ocular fundus,” Am J. Optom. Physiol. Opt. 56, 586–591 (1979). F. C. Delori, E. S. Gragoudas, R. Francisco, and R. C. Pruett, “Monochromatic ophthalmoscopy and fundus photography: normal fundus,” Arch. Ophthalmol. 95, 861–868 (1977).