* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiac resynchronization therapy for pediatric heart failure
Remote ischemic conditioning wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Myocardial infarction wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
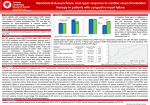
VIEWPOINT Cardiac resynchronization therapy for pediatric heart failure Jennifer N. Avari, MD, Edward K. Rhee, MD* From the Division of Pediatric Cardiology, Washington University School of Medicine/St. Louis Children’s Hospital, St. Louis, Missouri, and *Eller Congenital Heart Center, Heart Lung Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona. Introduction Pre-CRT implant/patient selection Cardiac resynchronization therapy (CRT) has been studied extensively and has been shown to improve quality of life and to increase survival in both ischemic and nonischemic adult heart failure patients. It has become the standard of care for symptomatic heart failure patients (New York Heart Association class III–IV) with depressed systemic ventricular function (ejection fraction ⬍35%) and wide QRS (⬎120 ms) despite optimal medical therapy. The pediatric heart failure population is a heterogeneous population comprising cardiomyopathy and congenital heart disease patients.1 The growing number of patients surviving surgical interventions has contributed to this heterogeneity. Current guidelines for CRT implantation in pediatric patients are broadly based on adult criteria. Pediatric patients receiving appropriate medical therapy for heart failure who have persistently poor cardiac function (measured by systemic ventricular ejection fraction) and wide QRS for age typically are referred for CRT evaluation as an alternative to cardiac transplantation. The CRT evaluation can be divided into three steps: (1) preimplant, (2) implant, and (3) postimplant. Appropriate patient selection preimplant is critically important given that use of current adult criteria for CRT implantation results in a nonresponder rate of 25% to 30%.2 Lead site selection studies, primarily conducted in adults with left bundle branch block, have shown that most patients can be successfully resynchronized from a lateral left ventricular (LV) lead. This issue has not been addressed in the pediatric population, in which isolated left bundle branch block is rare but chronic right ventricular (RV) apical pacing is common.1 Postimplant issues regarding CRT optimization, both atrioventricular (AV) and ventriculoventricluar (VV), in adult and pediatric patients have been discussed, with no clear consensus. This viewpoint addresses concerns facing the pediatric electrophysiologist at each time point. For children with two ventricles and a systemic LV, the established adult criteria for CRT implantation are applicable, with minor adjustments for QRS duration. However, when confronted with complex congenital heart disease (systemic RV or univentricular hearts), there are no coherent guidelines.1 Studies suggest that the echocardiographic presence of mechanical dyssynchrony preimplant, rather than QRS duration, is an indicator for CRT response.1–3 Mechanical dyssynchrony is assessed using two-dimensional echocardiography with M-mode and more frequently with tissue Doppler imaging.2 In 2008, the American Society of Echocardiography published their consensus statement on the use of echocardiography for CRT and concluded that the preferred approach is color-coded tissue Doppler for both the assessment of LV dyssynchrony and the prediction of outcome.2 The largest multicenter study to date on the role of echocardiography in evaluating dyssynchrony is PROSPECT (Predictors of Response to CRT; abstract presented at the European Society of Cardiology Congress, September 2007).2,4 Although final results are pending, preliminary data showed that no echocardiographic measure of mechanical dyssynchrony could be used to improve patient selection. In addition, very high levels of interobserver variability (6.5%–72%) indicate a need for further refinement of both technique and methodology as a modality for diagnosing dyssynchrony. Real time three-dimensional echocardiography also has been used in the evaluation of mechanical dyssynchrony.5 Early reports demonstrate that this imaging modality may correctly identify segments of late contraction; however, this technology is limited by low spatial and temporal resolution, with frame rates of approximately 20 to 30 frames per second.2 Using these echocardiographic measures of dyssynchrony for patients with structurally normal hearts is challenging, even more so when evaluating patients with complex cardiac anatomy and geometry. We have used noninvasive electrocardiographic imaging (ECGI) as an objective means for measuring electrical dyssynchrony. ECGI uses 250 body surface ECGs and a patient-specific heart– torso anatomy derived from ECG-gated thoracic computed KEYWORDS Congenital heart disease; Cardiomyopathy; Cardiac resynchronization therapy; Pediatric patients (Heart Rhythm 2008;5:1476 –1478) Address reprint requests and correspondence: Dr. Jennifer N. Avari, Division of Pediatric Cardiology, Washington University/St. Louis Children’s Hospital, NWT, Campus Box 8116, St. Louis, Missouri 63110. E-mail address: [email protected]. 1547-5271/$ -see front matter © 2008 Heart Rhythm Society. All rights reserved. doi:10.1016/j.hrthm.2008.05.024 Avari and Rhee Cardiac Resynchronization Therapy for Pediatric Heart Failure tomography to create epicardial activation isochrones throughout the ventricle(s). The electrical dyssynchrony index is computed from the ECGI maps as the standard deviation of activation times at 500 epicardial sites on the systemic ventricle. ECGI has been successfully and reproducibly used in heart failure patients6 and in pediatric patients with complex congenital heart disease and has been verified by invasive catheter mapping.7 At our institution, patients referred for CRT evaluation routinely undergo ECGI as part of the screening process. By identifying those patients with a high electrical dyssynchrony index (indicating significant electrical dyssynchrony), we attempt to objectively preselect patients who may benefit from CRT. Implicit in this approach is the assumption that the observed mechanical dyssynchrony is largely the result of the antecedent electrical dyssynchrony. We have termed the interval between electrical activation and regional myocardial contraction as “electromechanical latency.” Using electrical dyssynchrony as a surrogate for mechanical dyssynchrony is possible only if electromechanical latency is constant throughout the ventricle. Implant/lead site selection Select placement on the LV lead at the site of latest contraction has been shown to result in greater improvement in ejection fraction and cardiopulmonary workload.8 In a study by Becker et al,8 optimal lead location was defined as the site of or the site immediately neighboring the location of the latest contraction (as determined by speckle tracking) before CRT. Lead site selection in the pediatric population is complicated by their smaller hearts and complex coronary venous anatomy, which often accompany complex congenital heart disease. Implantation of CRT devices is complicated, especially when dealing with small hearts and complex anatomy, and often requires a team approach that includes a pediatric electrophysiologist and a pediatric cardiothoracic surgeon. Many pediatric centers electively place epicardial systemic ventricular leads. Historically, leads have been placed in a left lateral position or, if a pacing system is in place, 180° apart from the existing ventricular lead.1 Pre-CRT ECGI can be used to identify segments of late electrical depolarization as well as scar, lines of slow conduction, and block.6 In 2006, Jia et al6 demonstrated that ECGI was helpful not only in determining areas of late electrical depolarization but also in identifying these other important electrophysiologic properties of the ventricle. Identifying these regions preimplant can aid in selecting a suitable location for resynchronization pacing to promote electrical synchronicity. However, electrical synchrony does not always correlate with mechanical synchrony.6 The delay from epicardial activation to endocardial activation, or intramural delay, may be significant in advanced heart disease and has not been systematically studied. Electromechanical latency may account for those patients who are electrically synchronous but remain mechanically dyssynchronous as described by Jia et al.6 Although tissue Doppler 1477 imaging appears to be the ideal modality for assessing this parameter, technical obstacles and high interobserver variability have limited the utility of tissue Doppler imaging in guiding CRT lead placement. Cardiac magnetic resonance imaging also appears to be a promising imaging modality for assessing regional ventricular mechanical dyssynchrony; however, given the current state of pacemaker–magnetic resonance imaging compatibility, this modality is limited to only the preimplant phase. Postimplant/optimization Adult studies have demonstrated that many patients implanted with CRT and subsequently optimized have performed better than those patients not optimized.9 However, methods of optimization remain unclear and are institutional dependent. AV optimization is routinely performed using mitral valve Doppler inflow.2 Measuring mitral inflow E and A waves allows for selection of the optimal AV interval, which allows for completion of atrial systole (resulting in maximal preload) while preventing mitral diastolic regurgitation. This technique has been modified for patients with congenital heart disease by measurement of systemic AV valve inflow. Interventricular (VV) optimization has remained more ambiguous. Use of tissue Doppler imaging and tissue strain imaging to minimize segmental mechanical dyssynchrony is common, but both methods are subject to image acquisition and acoustic windows. At our institution, we first acquire 12-lead ECGs under various conditions, including single ventricular site pacing (RV only, LV only) and different VV timings, to determine those intervals with more fused QRS signals. Subsequently, tissue Doppler imaging and tissue strain imaging are performed during the subset of fused VV intervals to select the interval that minimizes segmental mechanical dyssynchrony. We do not limit the scope of the echocardiographic interrogation to the narrowest QRS complex. We have also used ECGI to assess post-CRT electrical dyssynchrony as well as changes in electrical dyssynchrony under different pacing conditions (Figure 1). This technique, first described in 2006,6 has repeatedly demonstrated that CRT clinical responders programmed to optimal CRT conditions have an electrical dyssynchrony index within the range of normal. Nominal CRT conditions have also shown a more normalized electrical dyssynchrony compared with single-site ventricular pacing (whether RV or LV), which consistently produces high electrical dyssynchrony indices indicating persistent dyssynchrony. Limitations One of the major limitations of ECGI is that it provides only epicardial data. Intramural delay and electromechanical latency may be quite significant, especially in diseased myocardium as seen in heart failure and structurally abnormal hearts, and may account for the population of patients who have electrical synchrony and persistent mechanical dyssyn- 1478 Heart Rhythm, Vol 5, No 10, October 2008 ure substrates, no studies have determined which substrates (if any) are more amenable to CRT. The long-term effects of pediatric CRT remain ambiguous due to the lack of longitudinal studies. The limitations of current echocardiographic techniques for patient selection, lead site selection, and optimization have been highlighted here and stress the importance of moving toward more objective methods. Noninvasive ECGI provides a safe, effective, and objective measure of electrical timing and underlying electrophysiologic substrate. In the future, the ability to create real-time patient activation isochrones may lead to a clinical role for ECGI in CRT optimization. References 1. 2. Figure 1 Noninvasive electrocardiographic image from a 6-year-old girl with complete congenital heart block who had undergone an upgrade from a dual-chamber pacemaker to cardiac resynchronization therapy (CRT) for dilated cardiomyopathy and heart failure. After the upgrade, she demonstrated dramatic improvement in clinical symptoms and echocardiographic findings (including increased ejection fraction from 29% to 55% and reverse remodeling of LV from an LV end-diastolic dimension z-score of 1.59 to 0.1 and end-systolic z-score of 4.09 to 1.06). The ECG image is shown for three different pacing conditions: C1 ⫽ CRT-optimal settings, C2 ⫽ left ventricular pacing only, and C3 ⫽ right ventricular pacing only. The greatest electrical synchrony is seen in C1, with more pronounced electrical dyssynchrony in both conditions C2 and C3. The patient’s electrical dyssynchrony (ED) indices demonstrated near normalization of ED index with CRT pacing and markedly abnormal ED indices in C2 and C3. chrony. Extension of ECGI to the endocardial surface will help overcome this difficulty. Future directions No dedicated trials to date have investigated patient selection, lead site location, or CRT optimization in the pediatric population. Given the heterogeneity of pediatric heart fail- 3. 4. 5. 6. 7. 8. 9. Dubin AM, Janousek J, Rhee E, et al. Resynchronization therapy in pediatric and congenital heart disease patients: an international multicenter study. J Am Coll Cardiol 2005;46:2277–2283. Gorcsan J 3rd, Abraham T, Agler DA, et al. American Society of Echocardiography Dyssynchrony Writing Group. Echocardiography for cardiac resynchronization therapy: recommendations for performance and reporting—a report from the American Society of Echocardiography Dyssynchrony Writing Group Endorsed by the Heart Rhythm Society. J Am Soc Echocardiogr 2008;21:191– 213. Jones BO, Davis AM, Alison J, et al. Cardiac resynchronization therapy in a child with severe anthracycline-induced congestive heart failure and normal QRS duration. J Heart Lung Transplant 2007;26:1333–1335. Cleland JG, Abdellah AT, Khaleva O, et al. Clinical trials update from the European Society of Cardiology Congress 2007: 3CPO, ALOFT, PROSPECT and statins for heart failure. Eur J Heart Fail 2007;9:1070 –1073. Marsan NA, Henneman MM, Chen J, et al. Real-time three-dimensional echocardiography as a novel approach to quantify left ventricular dyssynchrony: a comparison study with phase analysis of gated myocardial perfusion single photon emission computed tomography. J Am Soc Echocardiogr 2008;21:801– 807. Jia P, Ramanathan C, Ghanem RN, et al. Electrocardiographic imaging on cardiac resynchronization therapy in heart failure: observation of variable electrophysiologic responses. Heart Rhythm 2006;3:296 –310. Ghosh S, Avari JN, Rhee EK, et al. Noninvasive electrocardiographic imaging (ECGI) of a univentricular heart with Wolff-Parkinson-White syndrome. Heart Rhythm 2008;5:605– 608. Becker M, Franke A, Breithardt OA, et al. Impact of left ventricular lead position on the efficacy of cardiac resynchronization therapy: a two-dimensional strain echocardiography study. Heart 2007;93:1197–1203. Toggweiler S, Zuber M, Kobza R, et al. Improved response to cardiac resynchronization therapy through optimization of atrioventricular and interventricular delays using acoustic cardiography: a pilot study. J Card Fail 2007;13:637– 642.