* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
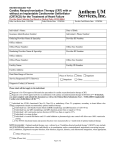
Download Indications for Cardiac Resynchronization Therapy: 2011
Coronary artery disease wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Heart failure wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Myocardial infarction wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiac surgery wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Journal of Cardiac Failure Vol. 18 No. 2 2012 HFSA CRT Guideline Update Indications for Cardiac Resynchronization Therapy: 2011 Update From the Heart Failure Society of America Guideline Committee WILLIAM G. STEVENSON, MD,1 ADRIAN F. HERNANDEZ, MD,2 PETER E. CARSON, MD,3 JAMES C. FANG, MD,4 STUART D. KATZ, MD,5 JOHN A. SPERTUS, MD, MPH,6 NANCY K. SWEITZER, MD, PhD,7 W.H. WILSON TANG, MD,8 NANCY M. ALBERT, RN, PhD, CNS,9 JAVED BUTLER, MD,10 CHERYL A. WESTLAKE CANARY, RN, PhD,11 SEAN P. COLLINS, MD, MSc,12 MONICA COLVIN-ADAMS, MD,13 JUSTIN A. EZEKOWITZ, MBBCh,14 MICHAEL M. GIVERTZ, MD,1 RAY E. HERSHBERGER, MD,15 JOSEPH G. ROGERS, MD,2 JOHN R. TEERLINK, MD,16 MARY N. WALSH, MD,17 WENDY GATTIS STOUGH, PharmD,18 AND RANDALL C. STARLING, MD, MPH8 Boston, Massachusetts; Durham and Buies Creek, North Carolina; Washington, DC; Cleveland, Ohio; New York, New York; Kansas City, Missouri; Madison, Wisconsin; Atlanta, Georgia; Azusa and San Francisco, California; Nashville, Tennessee; Minneapolis, Minnesota; Edmonton, Canada; Miami, Florida; and Indianapolis, Indiana ABSTRACT Cardiac resynchronization therapy (CRT) improves survival, symptoms, quality of life, exercise capacity, and cardiac structure and function in patients with New York Heart Association (NYHA) functional class II or ambulatory class IV heart failure (HF) with wide QRS complex. The totality of evidence supports the use of CRT in patients with less severe HF symptoms. CRT is recommended for patients in sinus rhythm with a widened QRS interval ($150 ms) not due to right bundle branch block (RBBB) who have severe left ventricular (LV) systolic dysfunction and persistent NYHA functional class II-III symptoms despite optimal medical therapy (strength of evidence A). CRT may be considered for several other patient groups for whom evidence of benefit is clinically significant but less substantial, including patients with a QRS interval of $120 to !150 ms and severe LV systolic dysfunction who have persistent mild to severe HF despite optimal medical therapy (strength of evidence B), some patients with atrial fibrillation, and some with ambulatory class IV HF. Several evidence gaps remain that need to be addressed, including the ideal threshold for QRS duration, QRS morphology, lead placement, degree of myocardial scarring, and the modality for evaluating dyssynchrony. Recommendations will evolve over time as additional data emerge from completed and ongoing clinical trials. (J Cardiac Fail 2012;18:94e106) Key Words: Heart failure, cardiac resynchronization therapy, guidelines. Minneapolis, Minnesota; 14Division of Cardiology, University of Alberta, Edmonton, Alberta, Canada; 15Department of Medicine, Division of Cardiology, University of Miami, Miami, Florida; 16Department of Medicine, University of California, San Francisco, California; 17The Care Group, Indianapolis, Indiana and 18Department of Clinical Research, Campbell University College of Pharmacy and Health Sciences, Buies Creek, North Carolina. Reprint requests: Randall C. Starling, MD, MPH, Vice Chairman, Cardiovascular Medicine, Cleveland Clinic, 9500 Euclid Avenue, Cleveland, OH 44195. Tel: 216-444-2268. E-mail: [email protected] This paper was reviewed and approved on December 9, 2011 by the Heart Failure Society of America Executive Council, whose members are listed in the Acknowledgment. See page 104 for disclosure information. 1071-9164/$ - see front matter Ó 2012 Elsevier Inc. All rights reserved. doi:10.1016/j.cardfail.2011.12.004 From the 1Department of Medicine, Division of Cardiology Brigham and Women’s Hospital, Boston, Massachusetts; 2Department of Medicine, Division of Cardiology, Duke University Medical Center, Durham, North Carolina; 3Georgetown University and Washington DC Veterans Affairs Medical Center, Washington, DC; 4Harrington-McLaughlin Heart and Vascular Institute, University Hospitals Case Medical Center, Case Western Reserve University School of Medicine, Cleveland, Ohio; 5Leon H. Charney Division of Cardiology, New York University School of Medicine, New York, New York; 6Mid-America Heart Institute of St Luke’s Hospital and University of MissourieKansas City, Kansas City, Missouri; 7 Department of Medicine, University of Wisconsin, Madison, Wisconsin; 8 Department of Cardiovascular Medicine, Cleveland Clinic, Cleveland, Ohio; 9Heart and Vascular Institute, Cleveland Clinic, Cleveland, Ohio; 10 Department of Medicine, Division of Cardiology, Emory University, Atlanta, Georgia; 11School of Nursing, Azusa Pacific University, Azusa, California; 12Department of Emergency Medicine, Vanderbilt University, Nashville, Tennessee; 13Cardiovascular Division, University of Minnesota, 94 Current Indications for CRT in Heart Failure Cardiac resynchronization therapy (CRT), achieved by biventricular (left ventricular [LV] and right ventricular [RV]) pacing has been shown to improve survival, morbidity, symptoms, quality of life, exercise capacity, and cardiac structure and function in patients with New York Heart Association (NYHA) functional class III or ambulatory class IV heart failure with wide QRS complex.1e6 CRT improves morbidity and mortality in this population, both with and without an implantable cardioverter defibrillator (ICD).7,8 As a result of these data, national and international guidelines, including those of the Heart Failure Society of America (HFSA), uniformly recommend CRT for patients with appropriate clinical characteristics when on optimal pharmacologic heart failure therapy.9e12 Although a substantial body of evidence supports the use of CRT in NYHA functional class III or ambulatory class IV patients with heart failure, clinical trial data for CRT in patients with mild (NYHA functional class I and II) heart failure symptoms were only beginning to emerge at the time the 2010 HFSA Guideline update was being written. Data have now been published for NYHA functional class I or II patients13e15 that may be sufficient to justify a modification of existing HFSA guideline recommendations. The purpose of this paper is to examine the recent evidence for CRT in patients with mild heart failure symptoms and reduced LV ejection fraction (LVEF), to reevaluate the indications for CRT in this population, and to provide guidance for clinicians on how to integrate this evidence into their clinical practice. This manuscript has been developed by the HFSA Guidelines Committee and reviewed and approved by the Executive Council. Pathophysiology of Dyssynchrony and Mechanism of Cardiac Resynchronization Therapy Conduction delays occur commonly in patients with heart failure and lead to electrical and mechanical dyssynchrony. Electrical dyssynchrony is defined by a QRS duration of $120 ms. An estimated 20%e30% of patients with heart failure meet this criterion.1,16e18 Inter- and intraventricular mechanical dyssynchrony lead to less efficient LV contractile performance, increased LV end-systolic volume (LVESV), increased left atrial pressure, and valvular dysfunction.1,6e8,19 By restoring synchrony, CRT reverses LV remodeling as evidenced by increases in LV filling time and LVEF and decreases in LV end-diastolic and end-systolic volumes, mitral regurgitation, and septal dyskinesis.1,15,19,20 There is no evidence to date that CRT provides a benefit in terms of functional status21 or mortality and morbidity in patients with narrow QRS and mechanical dyssynchrony.22 Until such evidence develops, CRT is not recommended for patients with a narrow QRS. Ongoing clinical trials are addressing this important question.23,24 Stevenson et al 95 Review of the Evidence for Cardiac Resynchronization Therapy in Patients With Mild Heart Failure Symptoms and Reduced Ejection Fraction CRT reduced mortality and morbidity among patients with NYHA functional class III-IV heart failure and dyssynchrony in several randomized controlled clinical trials.7,8,25 These data, in conjunction with evidence of reverse remodeling, led to the hypothesis that CRT may be effective at delaying or reversing disease progression in a heart failure population with mild symptoms through LV reverse remodeling. Three large randomized controlled trials of CRT in patients with mild heart failure symptoms have been completed (Tables 1 and 2). Resynchronization Reverses Remodeling in Systolic Left Ventricular Dysfunction (REVERSE) Patients were eligible to participate in REVERSE if they had American College of Cardiology (ACC)/American Heart Association (AHA) stage C heart failure with NYHA functional class I (history of symptoms but currently asymptomatic) or class II symptoms for $3 months before enrollment.13 Other eligibility criteria included LVEF #40%, QRS duration $120 ms, and LV enddiastolic diameter (LVEDD) $55 mm. Patients were excluded if they had NYHA functional class IIIeIV symptoms or a heart failure hospitalization #3 months before enrollment. All patients underwent CRT implantation and were subsequently randomized 2:1 to CRT-ON or CRTOFF for 12 months in the North American cohort and for 24 months in the European cohort. The primary end point was a clinical composite score of worsened (death, hospitalization, treatment crossover or discontinuation attributed to worsening heart failure, worsening NYHA functional class, or worsening patient global assessment of symptoms), unchanged, or improved (no worsening, and improvement in NYHA functional class or patient global assessment of symptoms) status. The secondary end point was absolute change in LV end-systolic volume index (LVESVI) from baseline to 12 months. A total of 419 patients were randomized to CRT-ON and 191 to CRT-OFF. The proportion of patients who worsened over the 12-month study period was 16% in the CRT-ON group and 21% in the CRT-OFF group, a difference that was not statistically significant (P 5 .1). The odds ratio for worsening in the clinical composite score was 0.7 (95% confidence interval [CI] 0.45e1.07), and its direction was consistent across multiple subgroups. The only statistically significant effect of CRT on the risk of worsening was in the QRS duration $152 ms subgroup (odds ratio [OR] 0.42, 95% CI 0.22e0.81) and in the nonischemic subgroup (OR 0.49, 95% CI 0.24e0.99). Appropriate caution must be taken when evaluating positive subgroup findings in circumstances where the test of the primary hypothesis was not significant. CRT delayed the time to first heart failure hospitalization (hazard ratio [HR] 0.47; P 5 .03). No Trial n Population Trials in Patients with Mild Heart Failure Symptoms n 5 191 CRT- ACC/AHA stage C; NYHA REVERSE13 OFF; I or II; sinus rhythm; n 5 419 CRTQRS $120 ms; LVEF #40; ON LVEDD $55 mm n 5 82 CRT- ACC/AHA stage C; NYHA I or II; REVERSEOFF; sinus rhythm; QRS $120 ms; Europe20 n 5 180 CRTLVEF #40; LVEDD $55 mm ON Mean QRS, ms 154 6 23 156 6 23.5 MADIT CRT15 n 5 731 ICD; NYHA I or II, sinus rhythm, n 5 1,089 LVEF #30, QRS $130 ms CRT-D 64.7% with QRS $150 ms RAFT14 n 5 904 ICD; NYHA II or III (revised to n 5 894 include only II; 80% were II); CRT-D LVEF #30 QRS $120 (paced QRS $200 ms) Sinus or perm AF 157.5 6 24 Trials in Patients with Moderate to Severe Heart Failure Symptoms COMPANION n 5 308 OPT; NYHA III or IV, LVEF #35%, 159 n 5 617 CRT; QRS $120 ms, PR O150 ms n 5 595 CRT-D CARE-HF n 5 404 Med; NYHA III or IV despite standard tx; Median 160 n 5 409 LVEF !35%, LVEDDI O30 mm, (IQR 152e CRT þ Med QRS O120 ms (those with 180) 120e149 ms had to meet 2 of 3 other criteria for dyssynchrony) Mean LVEF Background Therapy 26.2 6 7.1 ACEI or ARB 96.5%; BB 95%; CRT-D 83.5% Baseline 6-Min Walk Distance, m 393.5 6 128.5 Mean Age (y) Comorbidities 62.4 6 11.1 Ischemic 53.5%; diabetes 23% Control Control Group HF Group Hospitalization Mortality Rate (Length of (Length of Follow-Up) Follow-Up) 1.6% (12 mo) 28 6 6.5 ACEI or ARB 99.5%; 436 6 103.5 61.1 6 10.6 Ischemic 42.5%; 8.6% (24 mo) BB 92.5%; CRT-D previous MI 69% 34%; diabetes 15.5%; HTN 35%; PVD 4/5% 24 6 5 ACEI 77%; 361 6 108 64.5 6 11 Ischemic (NYHA I) 7.3% (2.4 y) ARB 20.5%; 14.8%; BB 93%; Ald ischemic (NYHA ant 31.5% II) 40.2%; nonischemic (NYHA II) 45.1%; NYHA III/IV O3 mos before 10%; HTN 63.5%; AF 11.9%; diabetes: 30.4% 22.6 6 5.3 ACEI or ARB 96.5%; 353 6 108 66.2 6 9.4 Ischemic 66.8%; 26.1% (40 BB 89.5%; spiron nonischemic mo) 42% 33.2%; HTN 44.5%; Diabetes: 33.7%; PVD 10%; HF hosp preceding 6 mo 25.7% 21% ACEI or ARB 89.5%; BB 67%; loop 95.5%; spiron 54% Median 25% ACEI or ARB 95%; (IQR 21e BB 72%; spiron 29) 56.5%; high-dose loop 43.5%; digoxin 42.5% 259 67 No data Median 66.5% Ischemic 56.5%; diabetes 42% Ischemic 38% 14/191 (7%) (12 mo) 14/82 (17.1%) (24 mo) 22.8% (2.4 y) 26.1% (5 y) 19% (annual) 12.6% (annual) 33% (29.4 mo) 96 Journal of Cardiac Failure Vol. 18 No. 2 February 2012 Table 1. CRT in Patients With Heart Failure: Study Populations Current Indications for CRT in Heart Failure difference in all-cause mortality was observed between study groups. The European cohort included 24-month follow-up on blinded therapy in 262 patients (CRT-ON: n 5 180; CRTOFF: n 5 82).20 Compared with the overall cohort, the European patients were younger, had a longer mean QRS duration, and were less likely to have ischemic or hypertensive heart disease. At 24 months, the heart failure clinical composite score worsened in 19% of CRT-ON patients compared with 34% of CRT-OFF patients (P 5 .01). The direction and magnitude of benefit for CRT on the heart failure clinical composite score was consistent across multiple subgroups. In the NYHA functional class I subgroup, the point estimate favored CRT-OFF, but the confidence interval was quite large, reflecting the small number (n 5 44) of subjects in this subgroup. Therefore, definitive conclusions cannot be drawn from this observation. Although the effect size appeared to be larger in the QRS duration $152 ms subgroup, no statistically significant heterogeneity was detected. CRT was beneficial and significantly increased the time to first heart failure hospitalization or death (P 5 .003) and time to first hospitalization alone (P 5 .01). Multicenter Automatic Defibrillator Implantation Trial With Cardiac Resynchronization Therapy (MADIT-CRT) MADIT-CRT randomized 1,820 patients with NYHA functional class I or II ischemic cardiomyopathy or NYHA functional class II nonischemic cardiomyopathy, LVEF #30%, and a QRS duration of $130 ms to CRT with defibrillator (CRT-D) or ICD only.15 The primary end point was all-cause mortality or nonfatal heart failure events (signs and symptoms of heart failure responsive to intravenous decongestive therapy on an outpatient basis or augmented decongestive therapy during an inpatient stay). Recurrent heart failure events were analyzed as secondary end points, and echocardiographic parameters of remodeling were evaluated as tertiary end points. The trial was stopped early by the data safety monitoring board after the prespecified efficacy boundary was crossed. Mean follow-up was 2.4 years. Background medical therapy was excellent, with the majority of patients on inhibitors of the renin-angiotensin-aldosterone system and betablockers. All-cause death or nonfatal heart failure events occurred in 187 patients (17.2%) randomized to CRT-D and to 185 (25.3%) randomized to ICD only (HR 0.66, 95% CI 0.52e0.84; P 5 .001). The effect was driven by a reduction in heart failure events (mortality 3.3% CRT-D vs 2.5% ICD only; nonfatal heart failure 13.9% CRT-D vs 22.8% ICD only). Results from a prespecified MADIT-CRT substudy showed that CRT-D was associated with a significant reduction in the risk of a first heart failure event (as defined above; HR 0.54, 95% CI 0.44e0.67; P ! .001) and subsequent heart failure events (HR 0.62, 95% CI 0.45e0.85; P 5 .003).26 Stevenson et al 97 The MADIT-CRT results illustrate the importance of individually reporting the components of composite end points so that the weight of evidence can be fully evaluated, particularly when ‘‘softer’’ end points are used (eg, outpatient intravenous diuretics for worsening heart failure). Such data underscore the importance of prespecified subgroup analyses that show the impact of the intervention on hospitalizations and nonhospitalization ‘‘heart failure events.’’ The hazard ratio for the primary end point was similar in ischemic and nonischemic patients. The findings were consistent across most prespecified subgroups, although subgroup treatment interactions were observed by sex (the effect size in women was larger than in men; P 5 .01) and QRS duration, where a reduction in the primary end point for CRT was observed only in the $150 ms subgroup (P 5 .001).15 Resynchronization-Defibrillation for Ambulatory Heart Failure Trial (RAFT) The primary objective of RAFT was to determine if CRT added to an ICD and optimal evidence-based pharmacologic therapy would decrease mortality and hospitalization for heart failure compared with ICD and optimal pharmacologic therapy alone.14 Initially, patients with NYHA functional class II or III symptoms were eligible, but the protocol was modified to include only class II patients after a mortality benefit was demonstrated in other studies of CRT for NYHA functional class III. Overall, 80% of patients were NYHA functional class II. Additional eligibility requirements included LVEF #30% and intrinsic QRS duration $120 ms or paced QRS duration $200 ms. A total of 1,798 patients were enrolled; 904 were randomized to ICD and 894 to CRT-D. Death or hospitalization for heart failure occurred in 33.2% of patients in the CRT-D group and 40.3% of patients in the ICD group (HR 0.75, 95% CI 0.64e0.87; P ! .001). All-cause mortality was 20.8% in the CRT-D group compared with 26.1% in the ICD group (HR 0.75, 95% CI 0.62e0.91; P 5 .003). The individual secondary end points of cardiovascular death and heart failure hospitalization were also significantly lower for patients randomized to the CRT-D group compared with ICD alone. Mean follow-up was 40 6 20 months. The findings of the primary analysis were consistent across multiple prespecified subgroups. The direction and magnitude of benefit was similar for patients with ischemic or nonischemic etiology and among patients with NYHA functional class II or III symptoms. A significant treatment interaction was noted for QRS duration (P 5 .003), indicating that patients with QRS duration $150 ms received greater benefit from CRT-D than the QRS !150 ms or paced QRS $200 ms subgroups. A weak interaction between treatment and QRS morphology was also observed, suggesting that CRT-D conferred a greater benefit in patients with left bundle-branch block (LBBB) than other types of conduction delay. Trial n Primary End Point Definition Mean Length of FollowUp REVERSE13 n 5 191 CRT-OFF; HF clinical composite response at n 5 419 CRT12 mo (worsened, unchanged, ON improved) 12 mo REVERSE Europe20 n 5 82 CRT-OFF; HF clinical composite response n 5 180 CRTat 12 mo (worsened, ON unchanged, improved) 24 mo MADIT CRT15 n 5 731 ICD; Death from any cause or n 5 1,089 CRTnonfatal HF events (signs/sx D of CHF responsive to IV outpt decongestive tx or augmented decongestive tx during inpt stay) n 5 904 ICD; Death from any cause or n 5 894 CRT-D HF leading to hosp 2.4 y RAFT14 Primary End Point Worsened: 21% CRT OFF vs 16% CRT-ON (P 5 .1); Improved/unchanged: 79% CRT-OFF vs 84% CRT-ON Mortality: 2.2% CRT-ON vs 1.6% CRT-OFF; P 5 .63 HF hosp: 17/419 CRT-ON vs 15/191 CRT-OFF HR for time to first HF hosp for CRT-ON vs CRT-OFF 5 0.47; P 5 .03 Worsened: 34% CRT OFF vs 19% Mortality (24 mo): 5.7% CRT-ON (P 5 .01); CRT-ON vs 8.6% Improved: 29% CRT-OFF vs 54% CRT-OFF (HR 0.4; P 5 .09) CRT-ON; HR for time to first Unchanged: 37% HF hosp for CRT-ON vs CRT-OFF vs 27% CRT-ON CRT-OFF 5 0.39; P 5 .01 187 (17.2%) CRT-D vs 185 (25.3%) All-cause mortality: 74 (6.8%) ICD; HR 0.66 (0.52e0.84), CRT-D vs 53 (7.3%) P 5 .001 ICD; HR 1.00, 95% CI 0.69e1.44; P 5 .99 40 6 20 364 (40.3%) ICD; 297 (33.2%) mo CRT-D; HR 0.75, 95% CI 0.64e0.87; P ! .001 COMPANION n 5 308 OPT; All-cause death or all-cause hosp 11.9e16.2 68% OPT; 56% CRT (HR 0.81, n 5 617 CRT; mo 95% CI 0.69e0.96; n 5 595 CRT-D P 5 .014); 56% CRT-D (HR 0.80, 95% CI 0.68e0.95; P 5 .01) CARE-HF n 5 404 Med; All-cause death or unplanned n 5 409 CRT þ hosp for CV event Med Additional Clinical Outcomes 29.4 (range 39% CRT vs 55% Med; 18e HR 0.63, 95% CI 0.51e0.77; 44.7) mo P ! .001 Subgroup Findings Consistent across subgroups; more benefit for QRS $152 ms vs !152 ms but interaction not significant Consistent across subgroups; more benefit for QRS $152 ms vs !152 ms but interaction not significant Subgroup treatment interactions: CRT-D benefit in men and women, but greater in women (P 5 .01); CRT-D better in QRS $150 ms; significant benefit not detected for QRS !150 ms (P 5 .001) Interaction for QRS !150 ms vs QRS $150 ms: P 5 .003; All-cause mortality: 236 (26.1%) ICD, 186 (20.8%) CRT-D; HR 0.75, 95% CI 0.62e0.91; P 5 .003 All-cause mortality (12 mo): 19% Consistent across subgroups, but progressive OPT, 15% CRT, 12% CRT-D; lowering of HR with increasing QRS CRT vs OPT: HR 0.76, 95% CI 0.58e1.01; P 5 .059 CRT-D vs OPT: HR 0.64, 95% CI 0.48e0.86, P 5 .003) All-cause mortality: 20% CRT, 30% Consistent across subgroups Med; HR 0.64, 95% CI 0.48e 0.85; P ! .002 98 Journal of Cardiac Failure Vol. 18 No. 2 February 2012 Table 2. CRT in Patients With Heart Failure: Clinical Outcomes Current Indications for CRT in Heart Failure Meta-Analyses A recent meta-analysis sought to evaluate the effect of CRT on all-cause mortality and included all CRT trials regardless of heart failure symptom severity.27 The overall analysis included 7,538 patients enrolled in 12 trials. A total of 4,054 patients were enrolled in 4 trials that included NYHA functional class I and II patients. Among patients with mild heart failure symptoms, 195/2,301 receiving CRT-D died compared with 212/1,753 patients receiving an ICD alone (risk ratio [RR] 0.80, 95% CI 0.67e0.96). This finding was similar to the effect in the total population (RR 0.83, 95% CI 0.72e0.96).27 Al-Majed et al evaluated the effect of CRT on morbidity and mortality in a meta-analysis of 25 trials including 9,082 patients.28 Among the 6 trials enrolling predominantly NYHA functional class I and II patients (n 5 4,572), CRT reduced all-cause mortality by 17% (RR 0.83, 95% CI 0.72e0.96; P 5 .01). Virtually all of the effect was due to RAFT. This effect was consistent with the risk reduction observed in the 19 trials enrolling predominantly NYHA functional class III and IV patients (n 5 4,510) (RR 0.78, 95% CI 0.67e0.91; P 5 .001). CRT was also associated with a decreased risk of heart failure hospitalization in NYHA functional class I and II patients (RR 0.71, 95% CI 0.57e0.87; P 5 .001) and in the NYHA functional class III and IV patients (RR 0.65, 95% CI 0.50e0.86; P 5 .002).28 The importance of QRS duration was recently explored in a meta-analysis by Sipahi et al.29 They hypothesized that patients with significantly prolonged QRS duration ($150 ms) derived greater benefit from CRT than those with shorter QRS duration (120e150 ms). The authors examined 5 prospective randomized CRT trials including 581 patients (in all NYHA functional classes) that reported clinical outcomes according to QRS duration. A reduction in death and hospitalizations with CRT was observed in patients with QRS duration $150 ms (RR 0.60, 95% CI 0.53e0.67; P ! .001). In contrast, no benefit of CRT was detected in patients with QRS !150 ms (RR 0.95, 95% CI 0.82e1.10; P 5 .49). There was a significant relationship between baseline QRS duration and risk ratio (P ! .001), with benefit of CRT appearing at a QRS $ 150 ms. The differential response of the 2 QRS groups was evident for all NYHA functional classes. This analysis supports the HFSA Guideline Committee’s approach to incorporate the magnitude of QRS prolongation into clinical decisions about appropriateness of CRT in chronic heart failure. Impact of New Evidence on Guideline Recommendations and Clinical Practice Guideline recommendations are based on the strength of evidence, which determines the strength of the recommendation.12 The HFSA uses 4 levels of strength in its guideline recommendations. These include ‘‘is recommended,’’ Stevenson et al 99 indicating that the therapy should be part of routine care and exceptions minimized; ‘‘should be considered,’’ indicating that the majority of patients should receive the intervention; ‘‘may be considered,’’ indicating that patient individualization is needed in the application of therapy; and ‘‘is not recommended,’’ indicating that the therapy should not be used.12 The 2010 HFSA Guideline contains the following recommendation regarding CRT in patients with mild heart failure symptoms: ‘‘9.10 Biventricular pacing therapy may be considered in patients with reduced LVEF and QRS duration $150 ms who have NYHA functional class I or II heart failure symptoms; strength of evidence 5 B.’’12 This recommendation reflects the lowest recommendation strength (‘‘may be considered’’) and a moderate strength of evidence (B). This recommendation was based on evidence from REVERSE and MADIT-CRT, studies that were available at the time of the last guideline update. The RAFT study contributes importantly to the totality of evidence and provides justification for a reexamination of the role of CRT in patients with heart failure and self-reported mild symptoms. Likewise, systematic reviews indicate that CRT is beneficial for patients with reduced LVEF, symptoms of heart failure, and prolonged QRS, regardless of NYHA functional class.27 Clearly, CRT trials are limited by the difficulty of correctly classifying the patient’s NYHA functional class, both as an entry criterion and as an assessment of efficacy. Therefore, it should be acknowledged that clinical benefit based on NYHA functional classification should be interpreted with caution. Is the Evidence Adequate to Justify an Increase in Recommendation and/or Evidence Strength? After evaluating the totality of evidence and based on the general consistency across clinical trials, the HFSA Guideline Committee determined that CRT is recommended for patients in sinus rhythm with a widened QRS interval ($150 ms) that is not due to right bundle branch block who have severe LV systolic dysfunction (LVEF #35%) and persistent mild-to-moderate heart failure (NYHA functional class IIeIII) despite optimal medical therapy (strength of evidence A). CRT may be considered for ambulatory NYHA functional class IV patients with QRS interval $150 ms and severe LV systolic dysfunction (LVEF #35%) (strength of evidence B). CRT may be considered for patients with a QRS interval of $120 to !150 ms and severe LV systolic dysfunction (LVEF #35%) who have persistent mild to severe heart failure (NYHA functional class II to ambulatory class IV) despite optimal medical therapy (strength of evidence B; Table 3). The evidence supporting the QRS thresholds in these recommendations is based primarily on findings from subgroup analyses (usually prespecified) and systematic reviews rather than on the boundaries of eligibility criteria used in the trials. It is acknowledged that subgroup analyses are generally limited by the potential for chance findings. However, the observation that the majority of benefit exists in the QRS duration $150 ms subgroup has been 100 Journal of Cardiac Failure Vol. 18 No. 2 February 2012 Table 3. Current HFSA Guideline Recommendations12 Existing Recommendation (2010 Guideline) 9.7 Biventricular pacing therapy is recommended for patients in sinus rhythm with a widened QRS interval ($120 ms) and severe LV systolic dysfunction LVEF (#35%) who have persistent moderate to severe HF (NYHA III) despite optimal medical therapy (strength of evidence A) 9.9 Selected ambulatory NYHA IV patients in sinus rhythm with QRS $120 ms and LV systolic dysfunction may be considered for biventricular pacing therapy (strength of evidence B) Add new recommendation 9.8 Biventricular pacing therapy may be considered for patients with atrial fibrillation with a widened QRS interval ($120 ms) and severe LV systolic dysfunction LVEF (#35%) who have persistent moderate to severe HF (NYHA III) despite optimal medical therapy (strength of evidence B). 9.10 Biventricular pacing therapy may be considered in patients with reduced LVEF and QRS $150 ms who have NYHA I or II HF symptoms (strength of evidence B) 9.11 In patients with reduced LVEF who require chronic pacing and in whom frequent ventricular pacing is expected, biventricular pacing may be considered (strength of evidence C) Summary of Change Potential Change in Recommendation and/or Strength of Evidence Change biventricular pacing to CRT throughout all recommendations Change QRS to $150, add not due to right 9.7 CRT is recommended for patients in sinus bundle branch block, add NYHA II rhythm with a widened QRS interval ($150 ms) that is not due to right bundle branch block who have severe LV systolic dysfunction LVEF (#35%) and persistent mild to moderate HF (NYHA functional class IIeIII) despite optimal medical therapy (strength of evidence A) Becomes 9.8; Change QRS to $150 ms 9.8 CRT may be considered for ambulatory NYHA functional class IV patients with QRS $150 ms and LV systolic dysfunction (LVEF #35%) despite optimal medical therapy (strength of evidence B) Becomes 9.9 9.9 CRT may be considered for patients with a QRS interval of $120 to !150 ms and severe LV systolic dysfunction (LVEF #35%) who have persistent mild to severe HF (NYHA functional class II to ambulatory class IV) despite optimal medical therapy (strength of evidence B) Becomes 9.10; Expand to include NYHA II 9.10 CRT may be considered for patients with atrial fibrillation with a widened QRS interval ($120 ms) and severe LV systolic dysfunction LVEF (#35%) who have persistent mild to moderate HF (NYHA functional class IIeIII) despite optimal medical therapy (strength of evidence B). Delete, covered under 9.7 Deleted No change a consistent finding across multiple clinical trials, and it has been confirmed in meta-analyses.29,30 Therefore, the guideline committee thought that the totality of evidence supported the QRS duration thresholds discussed above and in Table 3. The HFSA Guideline Committee also considers it their charge to place recommendations in the context of safety, efficacy, appropriateness, and cost-effectiveness. Patient Selection and Optimizing Response CRT is associated with a nonresponse rate of w30%.8 The ability to predict response or nonresponse is increasingly important for interventions that are costly, invasive, or associated with unique risks. There is considerable debate as to what clinical, echocardiographic, biochemical, or electrical outcome should be used, and at what time point, to assess response. Therefore, caution should be used when interpreting a single variable or study to identify a patient group that may respond more or less often to CRT. Although the totality of evidence supporting CRT in patients with mild heart failure symptoms is compelling, it is the HFSA’s view that consideration should be given to 9.11 In patients with reduced LVEF who require chronic pacing and in whom frequent ventricular pacing is expected, CRT may be considered (strength of evidence C) factors that influence responsiveness in an effort to ensure the optimal benefit and application of these data.31,32 Defining Mild Heart Failure. Categorizing patients into NYHA functional classifications IeIV is a subjective process. Therefore, it is helpful to quantitatively evaluate the severity of illness of patients enrolled in clinical trials so that the study results can be accurately applied to patient-level care.33 Control group mortality rates are useful indicators of illness severity. In the trials of CRT in patients with mild heart failure symptoms, control group mortality was 1.6% (12-month follow-up, REVERSE),13 8.6% (24-month follow-up, REVERSE-Europe),20 7.3% (2.4-year followup, MADIT-CRT),15 and 26.1% (40-month follow-up, RAFT).14 The use of background evidence-based therapies was similar across studies (Table 1). In comparison, the annual control group mortality in COMPANION (Comparison of Medical Therapy, Pacing, and Defibrillation in Heart Failure) was 19%8 and in CARE-HF (Cardiac Resynchronization Heart Failure Study) 12.6%,7 but these studies included NYHA functional class IV patients, who did not receive ICD, so they are not directly comparable with REVERSE, MADIT-CRT, and RAFT. The 1-year mortality rate in the Current Indications for CRT in Heart Failure CRTarm of CARE-HF was 9%, whereas it was w7.8% in the CRT-D arm of RAFT. These mortality rates suggest that the patient groups in REVERSE, MADIT-CRT, and RAFT were indeed less severely ill compared with earlier studies, with RAFT patients perhaps approaching a moderate severity of illness. It should be noted that !20% of patients enrolled in REVERSE (107 [17.5%]) and MADIT-CRT (265 [14.5%]), and no patients enrolled in RAFT, were NYHA functional class I. In REVERSE, it was stipulated that NYHA I patients had been symptomatic NYHA II before enrollment. In REVERSE-Europe, the point estimate for the effect of CRT on the composite clinical score in NYHA I favored CRT-OFF, but with an extremely wide confidence interval.20 In MADIT-CRT, the subgroup analysis of ischemic NYHA I also revealed an inconclusive finding for the effect of CRT on the end point of death or heart failure.15 Definitive conclusions cannot be drawn from these subgroup analyses. However, the findings, in conjunction with the small numbers of NYHA I patients enrolled, indicate that data are insufficient to support the broad application of CRT therapy in NYHA I patients at this time. In the mildly symptomatic heart failure population, objective evaluation of symptoms and functional capacity is critical, as is an assessment of optimal medical therapy before the implementation of CRT. Trials seeking to assess symptoms should use validated heart failureespecific tools and submaximal exercise testing.34e36 QRS Duration. As described above, a significant treatment interaction with QRS duration was observed in MADIT-CRT and RAFT, and a trend toward an interaction was observed in REVERSE (Table 1). QRS subgroup findings, along with results from meta-analyses, suggest that the effect of CRT on the study primary end point was limited to those patients with a QRS duration $150 ms.29 Based on the totality of evidence, the recommendation has been revised based on QRS duration and NYHA functional class, as presented in Table 3. In addition to the optimal QRS duration threshold, the optimal measurement technique for dyssynchrony or if it is even necessary is debated.37,38 Because CRT aims to correct mechanical dyssynchrony, the utility of QRS duration to predict response to CRT may be imperfect. Echocardiographic measures of dyssynchrony have been proposed as alternatives to QRS duration, but the reliability of current approaches have not been confirmed in clinical trials.21,39 Minimal research in this area has been done specifically in the mildly symptomatic heart failure population. Currently, mechanical dyssynchrony is not recommended as a means to identify patients who should receive CRT. QRS Morphology. Subgroup analyses from MADITCRT demonstrated that patients with LBBB benefit from CRT, whereas the effect of CRT was neutral among patients with other types of conduction delay.40 The LBBB subgroup was not prespecified, but the data were considered to be sufficient by the US Food and Drug Administration to justify adding LBBB to the indication labeling for Stevenson et al 101 CRT-D in NYHA functional class II or ischemic class I heart failure. In RAFT, patients with LBBB who were randomized to CRT-D had a lower risk of death or hospitalization for heart failure, whereas no benefit was observed in the right bundle branch block, nonspecific intraventricular conduction delay, or paced subgroups, with an interaction P value of .046.14 Although not definitive, patients with LBBB appear to derive the most benefit from CRT, and it may be a useful marker to guide patient selection. It should be noted that patients with RBBB appear to derive minimal to no benefit from CRT, regardless of QRS duration. Sex. Although both men and women benefit from CRT, some data suggest that women may benefit to a greater degree than men. In MADIT-CRT, the point estimate for benefit in women was larger than that for men, with a treatment interaction of P 5 .01.15 On further analysis, women had significantly greater reductions in death or heart failure, heart failure alone, and all-cause mortality compared with men.41 Additionally, women experienced greater improvements in echocardiographic measures of reverse remodeling.41 Current evidence does not support differences in practice or delivery of care for men and women. More research is needed to further evaluate potential gender differences in response to CRT. Lead Placement. The position of the LV pacing lead influences patient responsiveness to CRT.42 The impact of LV lead placement on clinical outcomes was analyzed in 799 patients enrolled in the MADIT-CRT study.43 Lead placement was characterized as anterior, lateral, or posterior position for the short axis and basal, midventricular, or apical for the long axis. No difference in the primary end point (all-cause mortality or nonfatal heart failure) was observed between leads placed in the posterior, anterior, or lateral regions (unadjusted P 5 .652). LV leads positioned in the apical region were associated with a higher risk of death or nonfatal heart failure events after adjustment for covariates (HR 1.72, 95% CI 1.09e2.71; P 5 .019) and a higher risk of mortality alone (HR 2.91, 95% CI 1.42e5.97; P 5 .004). Based on present data, physicians should avoid implanting a CRT lead in the apical region of the LV.43 When transvenous placement of an LV lead is not possible, surgical epicardial placement may be feasible. The accompanying surgical risks warrant careful individualized consideration.44 Atrial Fibrillation. More evidence is needed to guide the appropriate use of CRT in patients with atrial fibrillation. In patients with a CRT device and atrial fibrillation, atrioventricular (AV) node ablation should be considered when rapid AV conduction in atrial fibrillation prevents consistent CRT pacing despite attempted pharmacologic rate control.45 Other Patient Selection Criteria. Other factors may also influence response to CRT.46 The extent of myocardial scarring may play a role and may be associated with reduced CRT responsiveness. Data are insufficient to support a specific recommendation, but clinicians should weigh the 102 Journal of Cardiac Failure Vol. 18 No. 2 February 2012 risks and potential benefits of CRT implantation in patients with extensive myocardial scar, particularly in the location of the LV lead placement. Optimization Techniques and Follow-Up Management. CRT responsiveness may be influenced also by LV lead location and the specific programmed settings for pacing. The programmed AV delay is an important factor in determining whether LV capture occurs sufficiently early to promote synchrony, and it also influences ventricular filling. However, in a randomized trial of 1,014 patients, routine use of echocardiographic optimization of CRT pacing parameters at rest did not improve ventricular volume, 6-minute walk, or NYHA functional class compared with a fixed empirical AV delay or an electrocardiogram-based algorithm for assigning AV delay.47 Anecdotal and nonrandomized data suggest that some patients who fail to improve with CRT may benefit from reprogramming the device to ensure LV capture and improve AV timing.48 Thus, there is insufficient evidence to support any specific protocols or routine implementation of optimization techniques at this time beyond comprehensive heart failure disease management.12 After implantation of CRT, it is essential to assure utilization and monitoring of heart failure core therapies at recommended dosages, based on evidence-based guidelines.49 Furthermore, patients must understand that CRT implantation is not a substitute for adhering to self-care behaviors. Patients should continue to follow their pre-CRT plan of care for monitoring worsening signs and symptoms of heart failure and self-management behaviors. Safety Implementation of CRT requires an invasive procedure that carries risks. Upgrading an existing ICD or pacing system requires the addition of a new lead, which increases procedure risk. Replacing an existing ICD or pacemaker has also been associated with greater risk of infection. Lead dislodgment is generally the most commonly reported adverse event, and it occurred in 7% of RAFT patients, 4% of MADIT-CRT patients, and 10% of REVERSE patients (Table 4).13e15,20 Reoperation for repositioning is often required and may lead to significant morbidity. Among ICD patients in the National Cardiovascular Data Registry, lead dislodgements were associated with a significantly increased risk of cardiac arrest, cardiac tamponade, device infection, pneumothorax, and in-hospital mortality.50 Risk scores may be helpful to identify patients who are at high-risk of postprocedural complications.51 The long-term safety risks associated with CRT in patients with heart failure and mild symptoms have not been fully quantified. Patients with mild heart failure symptoms will likely survive with the CRT device for a longer period of time than patients in NYHA class III/IV, creating a greater opportunity for adverse events to occur. Complications due to pulse generator or lead failure requiring surgery are likely to be a greater concern for patients in NYHA functional class I or II compared with class III or IV, because the expected duration of therapy is longer in patients with fewer symptoms. Although generator replacement is generally benign, lead extraction or revision may be associated with greater risk. In the REPLACE (Implantable Cardiac Pulse Generator Replacement Registry), the major complication rate among patients in whom the addition of a lead was planned was 15.3% (95% CI 12.7e18.1%); the rate was 2.4% during the periprocedural period (cardiac perforation, pneumothorax, hemothorax, hemodynamic instability, cardiac arrest, respiratory arrest, coronary sinus dissection) and 14% out to 6 months.52 The major complication rate was 18.7% (95% CI 15.1e22.6%) among patients who underwent an upgrade to or revision of a CRT device, and this event rate differed significantly from the major complication rate among patients undergoing an upgrade or revision of a single-chamber pacemaker or ICD to a dual-chamber pacemaker (11.1%) or among those who did not ultimately receive a new lead (4.4%).41 The available follow-up data from clinical trials of CRT in patients with mild heart failure symptoms are too short to accurately characterize the long-term risk profile of the devices. Given the limited data currently available to describe long-term safety, the potential risks and potential benefits must be carefully evaluated for each patient. Patients and caregivers should be engaged in this process and informed about what is known and unknown regarding the benefits and risks of CRT in the setting of heart failure and mild symptoms to facilitate shared decision making among patients and their physicians. The potential for nonresponse should also be addressed. Cost Effectiveness of CRT in Patients With Mild Heart Failure Symptoms Among trials of CRT in patients with mild heart failure symptoms, the only cost-effectiveness analysis that has been published is from the REVERSE study.53 In that analysis, CRT was associated with a difference of 0.8 quality-adjusted life-years (QALY) over 10 years, corresponding to an incremental cost-effectiveness ratio of V14,278 per QALY gained (w$19,529). The number needed to treat to prevent 1 death was 4.9 at 10 years, and CRT became cost-effective after 4.5 years. These data are consistent with cost-effectiveness analyses of CRT in NYHA functional class IIIeIV patients. The incremental cost-effectiveness ratio was V18,017 (w$24,643) in CARE-HF, $43,000 in COMPANION, and $32,822 in an analysis of 5 CRT trials.19,53e56 Authors from REVERSE estimated that a relative mortality hazard ratio of 0.82 should enable CRT to be considered as cost-effective in patients with mild heart failure symptoms.53 The hazard ratio for mortality in RAFT was 0.75.14 It is important to recognize that because cost-effectiveness analyses consider both the incremental improvement in survival and the quality of that survival, the cost-benefit for patients with mild Current Indications for CRT in Heart Failure Stevenson et al 103 Table 4. Adverse Events Reported in Clinical Trials MADIT-CRT Pneumothorax (%) Infection (%) Pocket hematoma (%) Coronary venous dissection with pericardial effusion, n (%) LV coronary vein lead repositioned, n (%) Serious device-related adverse events RAFT Device- or implantation-related complications, n (%) Hemothorax or pneumothorax, n (%) Device pocket hematoma, n (%) Device pocket infection, n (%) Lead dislodgement, n (%) Device pocket problems, n (%) Coronary sinus dissection, n (%) REVERSE Pre/periprocedural complications Adverse drug reaction, n Pneumothorax, n Atrial fibrillation/flutter, n Coronary sinus dissection, n Pulmonary edema, n Ventricular fibrillation, n Complete heart block, n Cardiac tamponade, n Pericardial effusion, n Electromechanical dissociation, n Hypotension, n Increased defibrillation threshold, n Postimplantation complications LV lead dislodgement, n RV lead dislodgement, n Right atrial lead dislodgement, n Inappropriate device irritation of tissue, n Atrial fibrillation/flutter, n Implant site hematoma, n Hypotension, n Pericardial effusion, n COMPANION Moderate or severe AE from any cause, % AE related to implantation procedure, % Coronary venous dissection, % Coronary venous perforation, % Coronary venous tamponade, % CARE-HF Death from HF aggravated by lead displacement, n Death, septicemia, n Lead displacement, n Coronary sinus dissection, n Pocket erosion, n Pneumothorax, n Device-related infection, n Worsening HF, n Atrial arrhythmias or ectopy, n CRT-D ICD 1.7 1.1 3.3 5 (0.5) 44 (4) 4.5 per 100 device-months 0.8 0.7 2.5 118/888 (13.3%) 11 (1.2) 14 (1.6) 21 (2.4) 61 (6.9) 4 (0.5) 11 (1.2) 5.2 per 100 device-months 61/899 (6.8%) 8 (0.9) 11 (1.2) 16 (1.8) 20 (2.2) 1 (0.1) 26 procedure-/system-related complications in 642 patients (4%) 4 4 4 3 2 2 2 1 1 1 1 1 101/621 patients experienced 138 procedure-/system-related complications (16%) 41 15 10 14 8 5 4 4 69 (P 5 .03 vs OPT) 8 0.5 0.8 0.3 OPT: 61; CRT: 66 (P 5 .15 vs OPT) 10 0.3 1.1 0.5 1 (CRT) 1 (OPT after receiving a device) 24 10 8 6 3 OPT: 263; CRT: 191 (P ! .001) OPT: 41; CRT: 64 (P 5 .02) OPT, optimal pharmacologic therapy. symptoms may be realized by a reduction in future events through prevention of disease progression or an improvement in current symptoms. Reimbursement for device therapy often lags behind the evidence and/or guideline recommendations. Clinicians should be aware of reimbursement policies for CRT, and they should discuss this issue with patients as individually relevant. The potential for unreimbursed costs should be recognized and communicated to patients before CRT implantation. Remaining Evidence Gaps and Future Research Needs Further research is needed to clarify optimal strategies for selection and implementation of CRT in heart failure patients, because of the potential for heterogeneity in risks and benefits.57 Optimal patient selection is an area of key interest. Current patient selection is based on clinical trial eligibility criteria and findings from subgroup analyses, 104 Journal of Cardiac Failure Vol. 18 No. 2 February 2012 but identification of patients who will and will not respond to CRT needs to be further refined by rigorous scientific data.57 The evidence for CRT in NYHA functional class I patients is inconclusive, because these patients were underrepresented in the populations studied. However, in clinical practice, LV leads may be placed in patients who are likely to require frequent ventricular pacing, even if they have NYHA I symptoms. Although this practice occurs clinically, it is not data driven, and additional research in this area would be valuable. Identifying the most appropriate methodology for measuring dyssynchrony, defining optimal dyssynchrony thresholds, determining if CRT effects are consistent across all types of conduction delay, evaluating CRT effectiveness (responders vs nonresponders), and evaluating CRT in patients with atrial fibrillation are just some of the important patient selection questions that need to be addressed. Based on data currently available, patients with a narrow QRS complex derive no benefit from CRT. Whether there are patients with narrow QRS but mechanical ventricular dyssynchrony that would benefit from CRT is still under investigation, but CRT cannot be recommended at this time for that population.23 At present, QRS duration remains the best predictor of a favorable response to CRT.29 Furthermore, the clinical benefits of CRT for QRS durations between 120 and 150 ms remain unclear and can only be definitively addressed by prospective clinical trials. More research is needed to determine the future utility of measuring mechanical dyssynchrony in this setting, and adequate numbers of patients with mild symptoms (NYHA functional class II) should be studied to evaluate relevant differences across the spectrum of heart failure severity. The existing evidence to date involves de novo devices. Some patients who already have 1- or 2-lead ICDs experience changes in cardiac structure or function without an associated increase in symptoms. Whether or not these patients may benefit from an upgrade to CRT because of disease progression or chronic RV apical pacing is not well defined or understood, and further investigation of this issue is needed. Recent data have suggested that device upgrades may be associated with more risk than new implants.52,58e60 As CRT research moves into the mildly symptomatic heart failure population, where prevention of disease progression is a major concern, innovative research methodologies are needed. First, there needs to be an increased use of standardized assessments of patients’ symptoms, function, and quality of life, so that the results from clinical trials can be more readily translated to clinical care without the variability of interoperator reporting of NYHA functional class.61,62 Second, the use of functional status measures as outcomes that are clinically important to patients will improve the power of studies to define treatment benefit, given that event rates in these populations are lower than in the NYHA IIIeIV population. Third, functional status changes may trigger an order for an echocardiogram to assess LVEF, creating greater standardization in early identification of worsening LV systolic dysfunction that may meet criteria for CRT placement. The use of other surrogate end points, such as LVESV, LV end-diastolic volume, or dyssynchrony will be debated among scientist investigators and regulators. Conclusion The totality of evidence supports the use of CRT in heart failure patients with reduced LVEF across the spectrum of mild to severe symptoms. The evidence is most compelling among patients with QRS duration $150 ms and without RBBB. The guidance for clinicians offered in this document is based on an analysis of available evidence. However, many gaps exist in the data. Because these gaps are filled by the completion of ongoing and future studies, it is anticipated that recommendations will evolve to focus on optimizing patient selection and identifying factors that reliably predict a favorable response to CRT, ideally based on criteria that are clinically important to our patients. Acknowledgments The HFSA Guideline Committee acknowledges the administrative support of Cheryl Yano, Executive Director, HFSA, and Bart Galle, PhD. They also acknowledge the HFSA Executive Council for their careful review of this manuscript and their contributions to the document: Barry M. Massie, MD, Thomas Force, MD, Hani N. Sabbah, PhD, Mandeep R. Mehra, MD, Douglas L. Mann, MD, Inder S. Anand, MD, PhD, John C. Burnett, Jr, MD, John Chin, MD, Steven R. Houser, PhD, Sharon A. Hunt, MD, Mariell L. Jessup, MD, JoAnn Lindenfeld, MD, Sara C. Paul, RN, MSN, DNP, Mariann Piano, RN, PhD, Heather J. Ross, MD, James E. Udelson, MD, and Michael R. Zile, MD. Disclosures Randall C. Starling, MD, MPH, has received consulting fees/honoraria from Biocontrol, Medtronic, Novartis, Novella, and Thoratec and research grants from Biotronik (paid to the Cleveland Clinic); has equity interests/stock/ stock options with CardioMEMS; and is a board member of the United Network for Organ Sharing. James C. Fang, MD, has received consulting fees/honoraria from Boston Scientific and Medtronic and research grants from Medtronic (fellowship). Stuart D. Katz, MD, has received consulting fees/honoraria from Amgen, Bristol-Myers Squibb, and Terumo and is with the speaker’s bureau of Otsuka Pharmaceuticals. John A. Spertus, MD, MPH, receives a salary from Kansas City Cardiomyopathy Questionnaire. Nancy K. Sweitzer, MD, PhD, has received research grants from Medtronic as a site investigator. W. H. Wilson Tang, MD, has received consulting fees/honoraria from Medtronic and St Jude’s Medical and research grants from Abbott Laboratories. Javed Butler, MD, has received research grants from Medtronic, St Jude, and Boston Scientific as Current Indications for CRT in Heart Failure a site investigator. Sean P. Collins, MD, MSc, has received consulting fees/honoraria from Abbot Point-of-Care, PDL Biopharma, Astellas, Otsuka Pharmaceuticals, Bayer, Trevena, Novartis, The Medicine Company, and Corthera and research grants from Biosignetics, Inovise Medical, Abbott Point-of-Care, National Institutes of Health/National Heart, Lung, and Blood Institute, Corthera, and BRAHMS. Joseph G. Rogers, MD, has received consulting fees/honoraria from Thoratec. John R. Teerlink, MD, has received consulting fees/honoraria and research grants from Amgen, CardioMEMS, Corthera, Cytokinetics, Geron, Momentum Research, Novartis, Scios/Johnson & Johnson, and St Jude and research grants from the National Institutes of Health. Mary N. Walsh, MD, has received consulting fees/honoraria from Medtronic and United Health Care. All of the other authors report no potential conflicts of interest. References 1. Abraham WT, Fisher WG, Smith AL, Delurgio DB, Leon AR, Loh E, et al. Cardiac resynchronization in chronic heart failure. N Engl J Med 2002;346:1845e53. 2. Young JB, Abraham WT, Smith AL, Leon AR, Lieberman R, Wilkoff B, et al. Combined cardiac resynchronization and implantable cardioversion defibrillation in advanced chronic heart failure: the MIRACLE ICD Trial. JAMA 2003;289:2685e94. 3. Sutton MG, Plappert T, Hilpisch KE, Abraham WT, Hayes DL, Chinchoy E. Sustained reverse left ventricular structural remodeling with cardiac resynchronization at one year is a function of etiology: quantitative Doppler echocardiographic evidence from the Multicenter InSync Randomized Clinical Evaluation (MIRACLE). Circulation 2006;113:266e72. 4. Higgins SL, Hummel JD, Niazi IK, Giudici MC, Worley SJ, Saxon LA, et al. Cardiac resynchronization therapy for the treatment of heart failure in patients with intraventricular conduction delay and malignant ventricular tachyarrhythmias. J Am Coll Cardiol 2003;42:1454e9. 5. Auricchio A, Stellbrink C, Sack S, Block M, Vogt J, Bakker P, et al. Long-term clinical effect of hemodynamically optimized cardiac resynchronization therapy in patients with heart failure and ventricular conduction delay. J Am Coll Cardiol 2002;39:2026e33. 6. Cazeau S, Leclercq C, Lavergne T, Walker S, Varma C, Linde C, et al. Effects of multisite biventricular pacing in patients with heart failure and intraventricular conduction delay. N Engl J Med 2001;344: 873e80. 7. Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med 2005;352: 1539e49. 8. Bristow MR, Saxon LA, Boehmer J, Krueger S, Kass DA, De MT, et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med 2004;350:2140e50. 9. Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J 2008;29:2388e442. Stevenson et al 105 10. Dickstein K, Vardas PE, Auricchio A, Daubert JC, Linde C, McMurray J, et al. 2010 Focused update of ESC guidelines on device therapy in heart failure: an update of the 2008 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure and the 2007 ESC guidelines for cardiac and resynchronization therapy. Developed with the special contribution of the Heart Failure Association and the European Heart Rhythm Association. Eur Heart J 2010;31:2677e87. 11. Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, et al. 2009 Focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines Developed in Collaboration with the International Society for Heart and Lung Transplantation. J Am Coll Cardiol 2009;53:e1e90. 12. Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, et al. HFSA 2010 comprehensive heart failure practice guideline. J Card Fail 2010;16:e1e194. 13. Linde C, Abraham WT, Gold MR, St John SM, Ghio S, Daubert C. Randomized trial of cardiac resynchronization in mildly symptomatic heart failure patients and in asymptomatic patients with left ventricular dysfunction and previous heart failure symptoms. J Am Coll Cardiol 2008;52:1834e43. 14. Tang AS, Wells GA, Talajic M, Arnold MO, Sheldon R, Connolly S, et al. Cardiac-resynchronization therapy for mild-to-moderate heart failure. N Engl J Med 2010;363:2385e95. 15. Moss AJ, Hall WJ, Cannom DS, Klein H, Brown MW, Daubert JP, et al. Cardiac-resynchronization therapy for the prevention of heartfailure events. N Engl J Med 2009;361:1329e38. 16. Farwell D, Patel NR, Hall A, Ralph S, Sulke AN. How many people with heart failure are appropriate for biventricular resynchronization? Eur Heart J 2000;21:1246e50. 17. Shenkman HJ, Pampati V, Khandelwal AK, McKinnon J, Nori D, Kaatz S, et al. Congestive heart failure and QRS duration: establishing prognosis study. Chest 2002;122:528e34. 18. Fonarow GC, Albert NM, Curtis AB, Stough WG, Gheorghiade M, Heywood JT, et al. Improving evidence-based care for heart failure in outpatient cardiology practices: primary results of the Registry to Improve the Use of Evidence-Based Heart Failure Therapies in the Outpatient Setting (IMPROVE HF). Circulation 2010;122:585e96. 19. McAlister FA, Ezekowitz J, Hooton N, Vandermeer B, Spooner C, Dryden DM, et al. Cardiac resynchronization therapy for patients with left ventricular systolic dysfunction: a systematic review. JAMA 2007;297:2502e14. 20. Daubert C, Gold MR, Abraham WT, Ghio S, Hassager C, Goode G, et al. Prevention of disease progression by cardiac resynchronization therapy in patients with asymptomatic or mildly symptomatic left ventricular dysfunction: insights from the European cohort of the REVERSE (Resynchronization Reverses Remodeling in Systolic Left Ventricular Dysfunction) trial. J Am Coll Cardiol 2009;54:1837e46. 21. Beshai JF, Grimm RA, Nagueh SF, Baker JH, Beau SL, Greenberg SM, et al. Cardiac-resynchronization therapy in heart failure with narrow QRS complexes. N Engl J Med 2007;357:2461e71. 22. Marwick TH, Starling RC. The riddle of determining cardiac resynchronization therapy response a physiologic approach to dyssynchrony therapy. J Am Coll Cardiol 2008;52:1410e2. 23. Holzmeister J, Hurlimann D, Steffel J, Ruschitzka F. Cardiac resynchronization therapy in patients with a narrow QRS. Curr Heart Fail Rep 2009;6:49e56. 24. Echocardiography-Guided Cardiac Resynchronization Therapy (EchoCRT). ClinicalTrials.gov identifier: NCT00683696. 25. Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, et al. Longer-term effects of cardiac resynchronization therapy on mortality in heart failure (the Cardiac ResynchronizationeHeart Failure [CARE-HF] trial extension phase). Eur Heart J 2006;27:1928e32. 26. Goldenberg I, Hall WJ, Beck CA, Moss AJ, Barsheshet A, McNitt S, et al. Reduction of the risk of recurring heart failure events with cardiac resynchronization therapy: MADIT-CRT (Multicenter Automatic 106 Journal of Cardiac Failure Vol. 18 No. 2 February 2012 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. Defibrillator Implantation Trial with Cardiac Resynchronization Therapy). J Am Coll Cardiol 2011;58:729e37. Wells G, Parkash R, Healey JS, Talajic M, Arnold JM, Sullivan S, et al. Cardiac resynchronization therapy: a meta-analysis of randomized controlled trials. CMAJ 2011;183:421e9. Al-Majed NS, McAlister FA, Bakal JA, Ezekowitz JA. Meta-analysis: cardiac resynchronization therapy for patients with less symptomatic heart failure. Ann Intern Med 2011;154:401e12. Sipahi I, Carrigan TP, Rowland DY, Stambler BS, Fang JC. Impact of QRS duration on clinical event reduction with cardiac resynchronization therapy: meta-analysis of randomized controlled trials. Arch Intern Med 2011;171:1454e62. Kramer DB, Josephson ME. Three questions for evidence-based cardiac electrophysiology. Circ Cardiovasc Qual Outcomes 2010;3:704e9. Tang WH, Francis GS. Cardiac resynchronization therapy in patients with class IeII heart failure and a wide QRS: a cautionary note. Circulation 2011;123:203e8. Reynolds CR, Gold MR. Cardiac resynchronization therapy for mild heart failure: the time has come. Circulation 2011;123:195e202. Kubo SH, Schulman S, Starling RC, Jessup M, Wentworth D, Burkhoff D. Development and validation of a patient questionnaire to determine New York Heart Association classification. J Card Fail 2004;10:228e35. Green CP, Porter CB, Bresnahan DR, Spertus JA. Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure. J Am Coll Cardiol 2000;35: 1245e55. Rector TS, Kubo SH, Cohn JN. Validity of the Minnesota Living with Heart Failure Questionnaire as a measure of therapeutic response to enalapril or placebo. Am J Cardiol 1993;71:1106e7. Normand SL, Rector TS, Neaton JD, Pina IL, Lazar RM, Proestel SE, et al. Clinical and analytical considerations in the study of health status in device trials for heart failure. J Card Fail 2005;11:396e403. Prinzen FW, Auricchio A. Is echocardiographic assessment of dyssynchrony useful to select candidates for cardiac resynchronization therapy? Echocardiography is not useful before cardiac resynchronization therapy if QRS duration is available. Circ Cardiovasc Imaging 2008;1:70e7. Abraham J, Abraham TP. Is echocardiographic assessment of dyssynchrony useful to select candidates for cardiac resynchronization therapy? Echocardiography is useful before cardiac resynchronization therapy if QRS duration is available. Circ Cardiovasc Imaging 2008;1: 79e84. Chung ES, Leon AR, Tavazzi L, Sun JP, Nihoyannopoulos P, Merlino J, et al. Results of the Predictors of Response to CRT (PROSPECT) trial. Circulation 2008;117:2608e16. Zareba W, Klein H, Cygankiewicz I, Hall WJ, McNitt S, Brown M, et al. Effectiveness of cardiac resynchronization therapy by QRS morphology in the Multicenter Automatic Defibrillator Implantation TrialeCardiac Resynchronization Therapy (MADIT-CRT). Circulation 2011;123:1061e72. Arshad A, Moss AJ, Foster E, Padeletti L, Barsheshet A, Goldenberg I, et al. Cardiac resynchronization therapy is more effective in women than in men: the MADIT-CRT (Multicenter Automatic Defibrillator Implantation Trial with Cardiac Resynchronization Therapy) trial. J Am Coll Cardiol 2011;57:813e20. Singh JP, Fan D, Heist EK, Alabiad CR, Taub C, Reddy V, et al. Left ventricular lead electrical delay predicts response to cardiac resynchronization therapy. Heart Rhythm 2006;3:1285e92. Singh JP, Klein HU, Huang DT, Reek S, Kuniss M, Quesada A, et al. Left ventricular lead position and clinical outcome in the Multicenter Automatic Defibrillator Implantation TrialeCardiac Resynchronization Therapy (MADIT-CRT) trial. Circulation 2011;123:1159e66. Miller AL, Kramer DB, Lewis EF, Koplan B, Epstein LM, Tedrow U. Event-free survival following CRT with surgically implanted LV leads versus standard transvenous approach. Pacing Clin Electrophysiol 2011;34:490e500. Brignole M, Botto G, Mont L. Cardiac resynchronization therapy in patients undergoing AV junction ablation for permanent atrial 46. 47. 48. 49. 50. 51. 52. 53. 54. 55. 56. 57. 58. 59. 60. 61. 62. fibrillation: a randomized trial [abstract]. Heart Rhythm Society Scientific Sessions, May 5, 2011, San Francisco, California. LB-05. Gorcsan J III. Finding pieces of the puzzle of nonresponse to cardiac resynchronization therapy. Circulation 2011;123:10e2. Ellenbogen KA, Gold MR, Meyer TE, Fernndez Lozano IF, Mittal S, Waggoner AD, et al. Primary results from the SmartDelay determined AV optimization: a comparison to other AV delay methods used in cardiac resynchronization therapy (SMART-AV) trial: a randomized trial comparing empirical, echocardiography-guided, and algorithmic atrioventricular delay programming in cardiac resynchronization therapy. Circulation 2010;122:2660e8. Mullens W, Grimm RA, Verga T, Dresing T, Starling RC, Wilkoff BL, et al. Insights from a cardiac resynchronization optimization clinic as part of a heart failure disease management program. J Am Coll Cardiol 2009;53:765e73. Adlbrecht C, Hulsmann M, Gwechenberger M, Strunk G, Khazen C, Wiesbauer F, et al. Outcome after device implantation in chronic heart failure is dependent on concomitant medical treatment. Eur J Clin Invest 2009;39:1073e81. Cheng A, Wang Y, Curtis JP, Varosy PD. Acute lead dislodgements and in-hospital mortality in patients enrolled in the national cardiovascular data registry implantable cardioverter defibrillator registry. J Am Coll Cardiol 2010;56:1651e6. Haines DE, Wang Y, Curtis J. Implantable cardioverter-defibrillator registry risk score models for acute procedural complications or death after implantable cardioverter-defibrillator implantation. Circulation 2011;123:2069e76. Poole JE, Gleva MJ, Mela T, Chung MK, Uslan DZ, Borge R, et al. Complication rates associated with pacemaker or implantable cardioverterdefibrillator generator replacements and upgrade procedures: results from the REPLACE registry. Circulation 2010;122:1553e61. Linde C, Mealing S, Hawkins N, Eaton J, Brown B, Daubert JC. Costeffectiveness of cardiac resynchronization therapy in patients with asymptomatic to mild heart failure: insights from the European cohort of the REVERSE (Resynchronization Reverses Remodeling in Systolic Left Ventricular Dysfunction). Eur Heart J 2011;32:1631e9. Feldman AM, de LG, Bristow MR, Saxon LA, De MT, Kass DA, et al. Cost effectiveness of cardiac resynchronization therapy in the Comparison of Medical Therapy, Pacing, and Defibrillation in Heart Failure (COMPANION) trial. J Am Coll Cardiol 2005;46:2311e21. Calvert MJ, Freemantle N, Yao G, Cleland JG, Billingham L, Daubert JC, et al. Cost-effectiveness of cardiac resynchronization therapy: results from the CARE-HF trial. Eur Heart J 2005;26:2681e8. Jessup M. MADIT-CRTdbreathtaking or time to catch our breath? N Engl J Med 2009;361:1394e6. Kent DM, Rothwell PM, Ioannidis JP, Altman DG, Hayward RA. Assessing and reporting heterogeneity in treatment effects in clinical trials: a proposal. Trials 2010;11:85. Bogale N, Witte K, Priori S, Cleland J, Auricchio A, Gadler F, et al. The European Cardiac Resynchronization Therapy Survey: comparison of outcomes between de novo cardiac resynchronization therapy implantations and upgrades. Eur J Heart Fail 2011;13:974e83. Krahn AD, Lee DS, Birnie D, Healey JS, Crystal E, Dorian P, et al. Predictors of short-term complications after implantable cardioverter-defibrillator replacement: results from the Ontario ICD Database. Circ Arrhythm Electrophysiol 2011;4:136e42. Landolina M, Gasparini M, Lunati M, Iacopino S, Boriani G, Bonanno C, et al. Long-term complications related to biventricular defibrillator implantation: rate of surgical revisions and impact on survival: insights from the Italian Clinical Service Database. Circulation 2011;123:2526e35. Bennett JA, Riegel B, Bittner V, Nichols J. Validity and reliability of the NYHA classes for measuring research outcomes in patients with cardiac disease. Heart Lung 2002;31:262e70. Raphael C, Briscoe C, Davies J, Ian WZ, Manisty C, Sutton R, et al. Limitations of the New York Heart Association functional classification system and self-reported walking distances in chronic heart failure. Heart 2007;93:476e82.