* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Guidelines for Management of Skin and Soft Tissue Infection
Cryptosporidiosis wikipedia , lookup
Toxoplasmosis wikipedia , lookup
West Nile fever wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Herpes simplex wikipedia , lookup
Hookworm infection wikipedia , lookup
Gastroenteritis wikipedia , lookup
Marburg virus disease wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Trichinosis wikipedia , lookup
Sarcocystis wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Onchocerciasis wikipedia , lookup
Hepatitis C wikipedia , lookup
Schistosomiasis wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
Methicillin-resistant Staphylococcus aureus wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Hepatitis B wikipedia , lookup
Oesophagostomum wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Candidiasis wikipedia , lookup
Anaerobic infection wikipedia , lookup
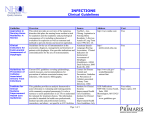
Guidelines for Management of Skin and Soft Tissue Infection Infectious Diseases Section VA Greater Los Angeles Healthcare System Updated April 2015 Table of Contents: General management principles for skin and soft tissue infection Criteria to determine complicated versus uncomplicated skin and soft tissue infection Uncomplicated skin and soft tissue infections: o Uncomplicated cellulitis o Uncomplicated cutaneous abscess/furunculosis o Mild diabetic foot infection Complicated skin and soft tissue infections: o Complicated cellulitis o Complicated cutaneous abscess/furunculosis o Moderate diabetic foot infection o Severe diabetic foot infection o Necrotizing fasciitis o Surgical site infection References [TOP] General Management Principles for Skin and Soft Tissue Infection: If the patient is febrile, obtain two sets of blood cultures. Obtain wound culture of drainage or purulence to determine if MRSA is present and tailor therapy accordingly. If isolated, S. aureus (MSSA or MRSA) almost always requires therapy. Treatment of gram negative and anaerobic pathogens is most important in the setting of devitalized, necrotic or ischemic tissues. Consider discontinuing MRSA-directed therapy if MRSA is not recovered from purulent wound drainage. Fluoroquinolones have very little activity against MRSA isolates at the VA Greater Los Angeles Healthcare System, and resistance can develop rapidly. Beta-lactam antibiotics are uniformly active against beta-hemolytic streptococci and inactive against MRSA (with the exception of ceftaroline). Doxycycline (100mg po bid) and trimethoprim-sulfamethoxazole (typically 1 DS tab bid) have very good activity against mild-moderate infections caused by MRSA that are suitable for oral therapy, but do not cover beta-hemolytic streptococci well. Clindamycin (300-600mg po tid) provides excellent activity against beta-hemolytic streptococci, but is effective against only about 80% of MRSA at GLA. [TOP] Criteria to Determine Complicated Versus Uncomplicated Skin and Soft Tissue Infection: A skin or soft tissue infection (SSTI) is considered complicated if it meets ANY of the following characteristics (otherwise it is deemed to be uncomplicated): Evidence for deep-seated infection Requirement for surgical intervention Presence of signs of systemic inflammatory response, including temperature > 38° C or < 36°C, heart rate > 90/min, respiratory rate > 20/min or PaCO2 < 32 mm Hg, and WBC > 12,000 or < 4000 cells/uL or ≥ 10% immature (band) forms Severe complicating co-morbidities and/or neutropenia Accompanying tissue ischemia/necrosis [TOP] UNCOMPLICATED SKIN AND SOFT TISSUE INFECTIONS: Uncomplicated cellulitis: Uncomplicated cellulitis is a diffuse, superficial, spreading skin infection that is NOT associated with collections of pus or purulent drainage and meets the criteria of uncomplicated SSTI above [link]. Cellulitis can be associated with lymphangitis and inflammation of the regional lymph nodes. Betahemolytic streptococci (mostly groups A and B) are the most common etiologic agents of cellulitis; staphylococci are unlikely in the absence of focal purulence or fluctuance. Treatment directed against S. aureus is typically not needed but can be considered for cellulitis associated with: Penetrating trauma (especially from illicit drug use) Concurrent evidence of S. aureus infection elsewhere. For simple cellulitis, treatment duration can be as short as 5 days if the patient responds well to initial therapy; otherwise consider a 10-14d course. Empiric oral antibiotic treatment options include: Cephalexin 500mg po qid (add minocycline or doxycycline 100mg po bid or TMP-SMX 1 DS tab po bid if risk for MRSA as above) Dicloxacillin 500mg po qid (add minocycline or doxycycline 100mg po bid or TMP-SMX 1 DS tab po bid if risk for MRSA as above) Clindamycin 300mg po tid [TOP] Uncomplicated cutaneous abscess/furunculosis: Cutaneous abscesses are collections of pus within the dermis and deeper skin tissues. Furuncles, more specifically, are infections of the hair follicle in which suppuration extends through the dermis into the subcutaneous tissue, forming an abscess. The most common etiology for skin abscesses is S. aureus, and the most important step in management is incision and drainage whenever possible (and sending the purulent drainage for culture). Warm compresses should be given for smaller lesions not amenable to drainage. Antibiotic therapy plays a secondary role to incision and drainage and is usually not necessary if the lesion is successfully drained and patient does not have signs of systemic infection. If the lesion cannot be drained fully or if the patient has impaired host defenses or signs of systemic infection, empiric antimicrobial therapy (typically 5-10d) should be directed against MRSA but should be narrowed based on cultures whenever possible. Empiric oral antibiotic options include: Doxycycline 100mg po bid OR TMP-SMX 1 DS tab po bid OR Clindamycin 300mg po tid [TOP] Mild Diabetic Foot Infection: Mild diabetic foot infection is defined as local infection involving only the skin and the subcutaneous tissue without involvement of deeper tissues and WITHOUT signs of systemic inflammatory response (temperature < 38° C and > 36°C, heart rate < 90/min, respiratory rate < 20/min or PaCO2 > 32 mm Hg, and WBC < 12,000 or > 4000 cells/µL or ≤ 10% immature (band) forms). Mild diabetic foot infection is typically be treated with oral agents, with inclusion of MRSA coverage if the patient has a current or recent wound culture positive for MRSA (deep wound cultures are preferable to superficial cultures). Antibiotic duration is generally 7-14d. Empiric antibiotic options include: MRSA coverage not warranted: Amoxicillin-clavulanate 875mg po bid Cephalexin 500mg po qid MRSA coverage warranted: Doxycycline 100mg po bid TMP-SMX 1 DS tab po bid Clindamycin 300mg po tid [TOP] COMPLICATED SKIN AND SOFT TISSUE INFECTION (Criteria for complicated SSTI are listed above [link]) These are serious infections that require the rapid application of appropriate diagnostic studies and therapeutic interventions. Complicated cellulitis: Complicated cellulitis is a diffuse, superficial, spreading skin infection that can be associated with lymphangitis and inflammation of the regional lymph nodes. Systemic manifestations of complicated cellulitis can include fever, tachycardia, confusion, hypotension, and leukocytosis (and can occur shortly before the skin abnormalities). By definition, complicated cellulitis is NOT associated with collection of pus or purulent drainage. Beta-hemolytic streptococci are the most common etiologic agents of cellulitis; staphylococci are less common in the absence of focal purulence or fluctuance. Treatment directed against MRSA is typically not needed but can be considered for cellulitis associated with: Penetrating trauma (especially from illicit drug use) Concurrent evidence of MRSA infection elsewhere. For complicated cellulitis, treatment duration should be for 7-14d. Intravenous antibiotics for empiric therapy of cellulitis include: Cefazolin 1gm IV q8h OR Vancomycin 1gm IV q12h (if risk for MRSA as above) [TOP] Complicated cutaneous abscess/furunculosis: Cutaneous abscesses are collections of pus within the dermis and deeper skin tissues. Furuncles, more specifically, are infections of the hair follicle in which suppuration extends through the dermis into the subcutaneous tissue, forming an abscess. Complicated cutaneous abscesses and furunculosis are defined by the criteria for complicated SSTI above [link]. The most common etiology for skin abscesses and furunculosis is S. aureus, and the most important step in management is incision and drainage whenever possible (and sending the purulent drainage for culture). Empiric therapy for complicated cutaneous abscess/furunculosis should be directed against MRSA but should be narrowed based on cultures whenever possible. Empiric antibiotic option: Vancomycin 1gm IV q12h [TOP] Moderate diabetic foot infection: Moderate diabetic foot infection is defined as local infection involving the skin and subcutaneous tissue with erythema > 2 cm, or involving deeper structures (e.g. abscess, osteomyelitis, septic arthritis, fasciitis) AND WITHOUT signs of systemic inflammatory response (temperature < 38° C and > 36°C, heart rate < 90/min, respiratory rate < 20/min or PaCO2 > 32 mm Hg, and WBC < 12,000 or > 4000 cells/µL or ≤ 10% immature (band) forms). Moderate diabetic foot infection may be treated with initial intravenous antimicrobial therapy with transition to oral agents when local signs of acute infection have resolved (i.e. erythema, warmth, tenderness, pain, and induration). Wound cultures should be performed on initial presentation whenever possible (deep wound cultures are preferable to superficial cultures). Duration of treatment is on the order of 7-14 days; longer therapy with oral agents would be needed if there is underlying osteomyelitis that is not resected. Consider podiatry consultation for assistance in surgical management and/or debridement and infectious diseases consultation for advice regarding antimicrobial management. Initial intravenous antibiotic options for moderate diabetic foot infection: Ampicillin-sulbactam 3gm IV q6h Ceftriaxone 2gm IV qd PLUS metronidazole 500mg po tid OR PLUS Vancomycin 1gm IV q12h [TOP] Severe diabetic foot infection: Severe diabetic foot infection is defined as local infection involving the skin and subcutaneous tissue and/or involving deeper structures (e.g. abscess, osteomyelitis, septic arthritis, fasciitis) WITH signs of systemic inflammatory response, including temperature > 38° C or < 36°C, heart rate > 90/min, respiratory rate > 20/min or PaCO2 < 32 mm Hg, and WBC > 12,000 or < 4000 cells/uL or ≥ 10% immature (band) forms). Wound cultures should be performed on initial presentation whenever possible (deep wound cultures are preferable to superficial cultures). Antibiotic choice will depend on whether there is concern for necrotizing infection. Podiatry/surgery consultation for assistance in surgical management and/or debridement and infectious diseases consultation for advice regarding antimicrobial management are STRONGLY recommended. Initial intravenous antibiotic options for severe diabetic foot infection: Vancomycin 1gm IV q12h PLUS Ertapenem 1gm IV q24h If life- or limb-threatening infection suspected: Vancomycin 1gm IV q12h PLUS Piperacillin-tazobactam 4.5gm IV q6h OR meropenem 1gm IV q8h [TOP] Necrotizing skin and soft tissue infections: Necrotizing skin and soft tissue infections are deeper infections that typically involve the fascial and/or muscle compartments, causing major tissue destruction and a high rate of mortality if not aggressively managed. They can extend from an initial skin lesion that may be trivial in nature and are accompanied by systemic toxicity (high fever, altered mental status), with local cutaneous inflammation, edema, and discoloration/gangrene. Subcutaneous tissue can often have a “woody” induration and may be associated with crepitance and/or substantial new tissue necrosis. Monomicrobial necrotizing infections are most commonly caused by group A streptococci and S. aureus, but other organisms should be suspected in patients with certain risk factors, including Aeromonas hydrophila (fresh water exposure) or Vibrio vulnificus (salt water/shellfish exposure). Gas gangrene and myonecrosis caused by clostridial species can be seen in the presence of recent trauma or surgery, neutropenia, or gastrointestinal malignancy. Polymicrobial necrotizing infections (in which multiple Gram-negative and anaerobic pathogens may be involved) are most commonly associated with infections involving or near the GI tract and/or perineum or injection sites in illicit drug users. Extremely severe pain, out of proportion to actual physical findings, is often present in certain necrotizing infections. Urgent/emergent surgical consultation for assistance in surgical management and/or debridement is essential and infectious diseases consultation for advice regarding antimicrobial management of necrotizing skin and soft tissue infections is STRONGLY recommended. Initial empiric intravenous antibiotic options for necrotizing skin and soft tissue infections include: Empiric therapy directed against Gram-positive organisms: Vancomycin 1gm IV q12h PLUS Clindamycin 900mg IV q8h (if streptococcal or clostridial etiology suspected) Empiric therapy directed against Gram-negative organisms and anaerobes (add to empiric Gram-positive coverage if polymicrobial infection is suspected) Piperacillin-tazobactam 4.5gm IV q6h OR Meropenem 1gm IV q8h OR Ciprofloxacin 400mg IV q8h AND metronidazole 500mg IV q8h PLUS Amikacin 7.5mg/kg IV q12h If there is concern for resistant Gram-negative bacillary infection [TOP] Surgical site infection: Fever is common within the first 2-4 days following surgery and is typically not associated with wound infection during this time frame. If, however, the patient is systemically ill with wound drainage or marked local signs of inflammation in this early time frame, wound infection with clostridia or streptococci may be present and should be evaluated with Gram stain and culture, debridement, and empiric therapy directed against these pathogens. Fever > 4 days following surgery should prompt a search for infectious sources: wound erythema and/or induration should prompt culture of any purulent material, evaluation for debridement, and antimicrobial therapy. Initial empiric intravenous antibiotic options for surgical site infections include: Severe, necrotizing infection suspected (ID consult strongly recommended): Empiric therapy directed against Gram-positive organisms: Vancomycin 1gm IV q12h PLUS Clindamycin 900mg IV q8h (if streptococcal necrotizing fasciitis suspected) Empiric therapy directed against Gram-negative organisms and anaerobes (add to empiric Gram-positive coverage if polymicrobial infection is suspected) Amikacin 7.5mg/kg IV q12h PLUS one of the following: Piperacillin-tazobactam 4.5gm IV q6h OR Meropenem 1gm IV q8h OR Cefepime 2gm IV q8h AND metronidazole 500mg IV q8h OR Ciprofloxacin 400mg IV q8h AND metronidazole 500mg IV q8h Surgery of intestinal or genitourinary tract or perineum: Pseudomonas suspected: Piperacillin-tazobactam 4.5gm IV q6h OR Meropenem 1gm IV q8h OR Cefepime 2gm IV q8h AND metronidazole 500mg IV q8h OR Ciprofloxacin 400mg IV q8h AND metronidazole 500mg IV q8h PLUS Vancomycin 1gm IV q12h (if MRSA suspected) Pseudomonas not suspected: Ceftriaxone 2gm IV qd PLUS metronidazole 500mg po tid OR Ertapenem 1gm IV qd PLUS Vancomycin 1gm IV q12h (if MRSA suspected) Surgery of trunk or extremity: Cefazolin 1gm IV q8h OR Vancomycin 1gm IV q12h (if MRSA suspected) [TOP] References: 1. Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis 2014;59(2):e10-52. [link] 2. Lipsky BA, Berendt AR, Cornia PB, et al. 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis 2012;54:e132-173. [link] 3. Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis 2011;52(3):e18-55. [link] 4. Dryden MS. Complicated skin and soft tissue infection. J Antimicrob Chemother 2010; 65(Suppl3):iii35-44. [TOP]