* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiovascular Alterations
Cardiovascular disease wikipedia , lookup
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Rheumatic fever wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Aortic stenosis wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Coronary artery disease wikipedia , lookup
Congenital heart defect wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
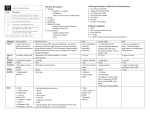
Cardiovascular Alterations NUR 264 Pediatrics Angela J. Jackson, RN, MSN Cardiovascular Alterations: Developmental Differences Heart sounds are higher pitched Pulse rate is higher Chest wall is thinner because of lack of subcutaneous tissue and muscle Cardiac output is dependent on heart rate until 5 years old Systolic murmur maybe present with fever and anemia without heart disease Fetal Circulation Foramen ovale closes shortly after birth Ductus venosus closes when umbilical cord is clamped Ductus arteriosus closes within 24 hours of birth Congenital Heart Defects: Acyanotic Disorders Acyanotic: oxygenated blood shunts from left to right where it mixes with unoxygenated blood Atrial septal defect Ventricular septal defect Patent ductus arteriosus Atrioventricular canal Coarctation of the aorta Aortic stenosis Pulmonic stenosis Congenital Heart Defects: Cyanotic Disorders Cyanotic: unoxygenated blood shunts from right to left where it mixes with oxygenated blood. Blood pumped through aorta to peripheral tissues has decrease oxygen resulting in cyanosis Tetralogy of Fallot Tricuspid atresia Transposition of great arteries Truncus arteriosus Hypoplastic left heart syndrome Congenital Heart Defects: General Clinical Manifestations Chest enlargement or asymmetry Abnormal heart sounds: murmurs Abnormal B/P readings Increased pulse and respirations Weak, muffled cry in infants Poor exercise tolerance, especially with feedings Posturing dyspnea with activity or stress Cyanosis: mucous membranes, nail beds, lips, extremities, decreased cap refill, doesn’t pink with O2 administration Congenital Heart Defects: General Clinical Manifestations Clubbing of fingers and toes @ 1-2 years of age in response to hypoxia CHF: early signs – tachypnea, dyspnea, retractions, grunting, tachycardia, diaphoresis on upper lip and forehead late signs – hepatomegaly, edema. Risk of left-sided heart failure Polycythemia Poor feeding, poor growth Squatting Frequent respiratory infections Congenital Heart Defects: Nursing Care Monitor vital signs Provide O2 to keep saturations at prescribed level Adequate nutrition: Infants: small frequent feedings, burp frequently, provide extra calories (24 calories /oz), soft nipple for bottle feeding, bottle for 20 minutes then tube feed rest of formula, feed before hungry to avoid crying. Children: avoid empty calorie foods, well-balanced meals, healthy snacks Congenital Heart Defects: Nursing Care Prevent cold stress Decrease energy expenditure: plan nursing care to allow for rest, prevent crying Skin care: decreased blood flow to periphery Medication administration: cardiac drugs, diuretics, anticoagulants, antibiotic prophylaxis Position: knee-chest, DO NOT interfere with squatting Prepare family and client for diagnostic studies, surgery Promote growth and development Teach parents to treat child normally, use discipline, don’t overprotect Congenital Heart Defects: Nursing Care Cardiac Catheterization Care: Cardiac Cath may be performed to obtain pressure gradients, O2 concentrations Pre-op: NPO 4-6 hours prior to procedure, obtain consent, check pulse strength, educate parents/child about procedure Post-op care: keep extremity straight, check pressure dressing on site, check pulse distal to site, NO BP on extremity, do neurovascular checks on extremity, monitor for dysrhythmias, hematoma, thrombus formation, infection. Monitor I&O as contrast medium may cause diuresis Cardiovascular Alterations: Atrial Septal Defect (ASD) Abnormal connection between the right and left atria Accounts for approximately 7% of all congenital heart disease ASD: Pathophysiology Normal increased pressure on the left side of the heart causes blood to flow from left to right through the ASD Leads to increased volume on the right side of the heart Increase in right atrial, right ventricular and pulmonary artery size ASD: Clinical Manifestations Usually asymptomatic May have a soft systolic murmur May have a widely split S2, unaffected by respiratory pattern (increased blood flow prolongs right ventricular emptying, causing a delay in pulmonic valve closure) ASD: Diagnosis Physical exam (detection of a murmur) Chest x-ray (increased heart size) Echocardiogram identifies the location and size of the defect ASD: Treatment Diuretics may be given preoperatively for symptoms of CHF The defect may close spontaneously during the first 2 years of life Surgery is performed in the preschool age child Defect is stitched closed or patched Insertion of an implantable umbrella through a large femoral vessel may also be an option Main complications of repair are atrial arrhythmias or heart block Ventricular Septal Defect (VSD) An abnormal connection between the right and left ventricles May be located in various positions along the septum Most common congenital heart defect VSD: Pathophysiology Normally increased pressure on the left side of the heart causes blood shunt from left to right through the VSD The blood recirculates through the pulmonary artery to the lungs Increased pulmonary blood flow leads to left heart enlargement and pulmonary venous congestion The degree of shunting depends on the size of the defect and pulmonary resistance VSD: Clinical Manifestations An infant with a small VSD may be asymptomatic Moderate to large defects result in CHF Tachypneic Diaphoretic Easily fatigued Underweight for age Poor feeding (tires before a feeding is completed) VSD: Diagnosis Physical exam Loud, harsh pansystolic murmur heard best at the left lower sternal border Chest x-ray reveals cardiomegaly with an increase in pulmonary blood flow Echocardiogram identifies the size and location of the defect VSD: Treatment 75-80% of small VSD close in the first two years of life Large defects are unlikely to close Treated medically for first few months Digoxin and diuretics for symptoms of CHF High calorie formula for growth May need NGT feedings Surgical repair Performed between 3 and 12 months of life Earlier in infants with failure to thrive Defect is closed with a patch of the child’s own pericardium Patent Ductus Arteriosus (PDA) The ductus arteriosus remains open Incidence in preterm infants: 45% Incidence in term infants: 5-10& PDA: Pathophysiology Left to right shunt Blood from high pressure aorta flows directly to low pressure pulmonary artery Degree of shunting depends on size of defect, as well as pulmonary vascular resistance Increased pulmonary blood flow can contribute to CHF PDA: Clinical Manifestations and Diagnosis Clinical manifestations Small PDA: asymptomatic Large PDA: signs and symptoms of CHF Diagnosis Continuous murmur best heard below the left clavicle Normal chest x-ray Diagnosed with echocardiogram PDA: Treatment May be closed with infusion of indomethacin in preterm infants Surgical closure in full-term, symptomatic infants Elective closure in older, asymptomatic children before age 5 Pulmonary Stenosis Narrowing of the pulmonary valve and obstruction to blood flow from the right ventricle to the lungs Obstruction may be: At the valve (Valve Before the valve After the valve stenosis) (subvalve stenosis) (supravalve stenosis) Pulmonary Stenosis: Pathophysiology Right ventricular pressure increases because of obstruction of blood flow from the RV to the pulmonary artery. This may result in RV failure Decreased amount of blood flow is able to get to the lungs Increased exertion may result in cyanosis Pulmonary Stenosis: Clinical Manifestations and Diagnosis Clinical Manifestations Mild to moderate PS may be asymptomatic Severe PS: dyspnea upon exertion, fatigue, cyanosis Murmur discovered on physical exam Diagnosis Physical exam Chest x-ray normal (severe PS may have cardiomegaly) Echocardiogram demonstrates size and function of RV and anatomy of pulmonary valve Pulmonary Stenosis: Treatment Neonates with critical PS require infusion of prostaglandins to maintain patency of the ductus arteriosus in order to provide adequate blood flow to the lungs until surgery can be performed Surgical repair Balloon valvuloplasty performed in the cardiac catheterization lab Surgical valvotomy Tetralogy of Fallot Made up of four components VSD Pulmonary stenosis Right ventricular hypertrophy Overriding aorta Degree of pulmonary stenosis is the most important component Most common cyanotic heart defect Tetralogy of Fallot: Pathophysiology Large VSD leads to equal pressures in right and left ventricles Amount of pulmonary blood flow and the amount of cyanosis is dependant on the degree of pulmonary stenosis Tetralogy of Fallot: Clinical Manifestations and Diagnosis Clinical Manifestations Dependant upon degree of PS, may be mildly or profoundly cyanotic Loud systolic murmur noted at birth Hypercyanotic spells (“tet spells”) may be brought on by crying, feeding or defecating Diagnosis Echocardiogram Chest x-ray often normal. May exhibit bootshaped heart Tetralogy of Fallot: Treatment Preoperative management of hypercyanotic spells: Place infant in knee-chest position. (Older children will squat) this decreases systemic venous return of unoxygenated blood and increases systemic vascular resistance, reducing right to left shunting and allowing more blood flow to the lungs Children in the hospital may be treated with morphine to relieve symptoms of agitation and break the cycle of hyperpnea. Other treatment includes: IV fluids to decrease blood viscosity, supplemental O2, IV phenylephrine to increase systemic vascular resistance. Infants with multiple hypercyanotic spells may need a palliative modified Blalock-Taussing (BT) shunt to assure pulmonary blood flow until complete surgical repair is performed Tetralogy of Fallot: Treatment Surgery: Performed between 6 and 12 months of age The pulmonary artery is widened and the VSD is closed If a BT shunt is in place, it is taken down or occluded at the time of the definitive repair Aortic Stenosis (AS) Narrowing of the aortic valve Causes obstruction to left ventricular outflow Increased afterload Increased ventricular work Left ventricular hypertrophy AS: Clinical Manifestations and Diagnosis Clinical Manifestations Infants usually grow normally, diagnosis made when older child is referred for evaluation of a murmur. Older children may also have: Exertional fatigue Dyspnea Angina Syncope with severe AS Diagnosis Physical exam Echocardiogram LV and aorta pressure gradients (less than 25 mm Hg are considered mild) Aortic Stenosis: Treatment Infants: administration of prostaglandins to keep the ductus arteriosus open Aortic valvotomy Children: Balloon valvuloplasty Valve replacement Hypoplastic Left Heart Syndrome (HLHS) Lack of development of the left ventricle secondary to mitral valve atresia or aortic atresia Small, hypoplastic left ventricle not capable of any cardiac function HLHS: Clinical Manifestations and Diagnosis Clinical Manifestations Cyanosis develops within hours of birth Hypotension, tachycardia, cyanosis, tachypnea One-third will present in cardiovascular collapse Diagnosis Physical exam Echocardiogram HLHS: Treatment Three treatment options No intervention Cardiac transplantation Palliative surgery Acute Rheumatic Fever Autoimmune reaction to an untreated or partially treated group A streptococcal pharyngitis Develops 2-6 weeks after infection Three organ systems affected: heart, central nervous system and the joints Acute Rheumatic Fever: Clinical Manifestations Valvulitis: inflammation of the heart valves – one of the most significant clinical features. New systolic murmur reflects mitral regurgitation Polyarthritis: most frequent benign major manifestation. Arthritis is migratory, there is tenderness, pain, swelling, heat and limitation of movement in the affected joints Erythema marginatum: fine, pink rash noted on the trunk and extremities, becomes more pronounced with heat. Always seen with carditis or polyarthritis Subcutaneous nodules: firm, painless nodules over the extensor surfaces of the elbows, knees and wrists. Always accompany carditis Acute Rheumatic Fever: Diagnosis Physical examination Laboratory findings Elevated sed rate and C-reactive protein (inflammation) ASO titers, anti-DNAse B (detects strep infection) EKG ECHO: most sensitive tool for diagnosis of valvar disease Acute Rheumatic Fever: Treatment Penicillin for eradication of strep bacteria Aspirin as an anti-inflammatory agent Bedrest until inflammation has resolved Repeat ECHO Antibiotic prophylaxis Frequent follow-up Kawasaki Disease (Acute Systemic Vasculitis) Vasculitis of multiple systems in the body, especially the coronary arteries First 10 days of the disease: infiltration of vessel walls with inflammatory cells causing inflammation and hypertrophy of blood vessels. Day 10 to day 40, decrease in inflammation. Vessels have undergone destructive changes. Coronary artery aneurysm can develop After 40 days, progressive fibrosis and healing of coronary artery abnormalities occurs. Aneurysms and dilation usually regress in one to two years Kawasaki Disease: Clinical Manifestations Abrupt onset of high fever lasting more than 5 days Conjunctival infection, photophobia Diffuse red rash Red strawberry tongue, cracked red lips Hands and feet swollen, palms and soles red, tips of fingers and toes peel, progressing to palms and soles Cervical lymphadenopathy Tachycardia, gallop rhythm, CHF Irritability Painful joints, aseptic meningitis, sterile pyuria, diarrhea Kawasaki Disease: Diagnosis Physical exam Elevated WBC, sed rate, platelet count Pyuria Elevated liver function tests ECHO for coronary aneurysms Kawasaki Disease: Treatment IV immune globulin: 2gm/kg IV over 10-12 hours, may repeat with 1gm/kg) Aspirin 100mg/kg/day in 4 divided doses until fever subsides, then 3-5mg/dg daily for 6-8 weeks Solu-medrol may be used with IVIG Coumadin if aneurysms >8mm Thrombolytics for vessel occlusion Coronary angioplasty, coronary artery bypass and graft or heart transplant for severe coronary artery disease Kawasaki Disease: Nursing Considerations VS, I%O, daily weight Supportive treatment – analgesics, fever reduction, soft foods, fluids, monitor calories Assess for S/S of CHF IVIG administration, monitor VS and side effects Parental involvement Discharge planning for medication administration, follow-up with cardiologist Questions?