* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 20
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Coronary artery disease wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Electrocardiography wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Artificial heart valve wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac surgery wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
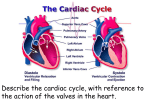
Chapter 20 The Heart I. Organization of the Cardiovascular System A. The cardiovascular system is divided into two circuits - Fig. 20.1 • • • Pulmonary circuit • blood to and from the lungs Systemic circuit • blood to and from the rest of the body Vessels carry the blood through the circuits • • • Arteries carry blood away from the heart Veins carry blood to the heart Capillaries permit exchange II. Anatomy of the Heart A. The pericardia - Fig. 20.2 • • Visceral pericardium or epicardium Parietal pericardium • Pericardial fluid B. Superficial Anatomy of the Heart - Fig. 20.3 • • The heart consists of four chambers • Two atria and two ventricles Major blood vessels of the heart include • • Inferior and superior vena cavae Aorta and pulmonary trunk C. The Heart Wall - Fig. 20.4, 20.5 • Components of the heart wall include • Epicardium • Myocardium • Endocardium D. Internal Anatomy and Organization - Fig. 20.6 • • • • Atria • Thin walled chambers that receive blood from the vena cavae Ventricles • Thick walled chambers separated from the atria by AV valves Chordae tendineae • Tendinous fibers attached to the AV valves Papillary muscle and trabeculae carneae • Muscular projections on the inner wall of ventricles E. Blood flow through the heart • Right atria • Right ventricle • • • • • • Tricuspid valve Pulmonary valve Pulmonary circuit Left atria • Bicuspid valve Left ventricle • Aortic valve Aorta and systemic circuit F Heart chambers and valves - Fig. 20.7, 20.8 • • Structural Differences in heart chambers • The left side of the heart is more muscular than the right side Functions of valves • • AV valves prevent backflow of blood from the ventricles to the atria Semilunar valves prevent backflow into the ventricles from the pulmonary trunk and aorta F. Blood Supply to the Heart - Fig. 20.9 • • Arteries include the right and left coronary arteries, marginal arteries, anterior and posterior interventricular arteries, and the circumflex artery Veins include the great cardiac vein, anterior and posterior cardiac veins, the middle cardiac vein, and the small cardiac vein III. The Heartbeat A. Cardiac Physiology - Fig. 20.11 • Two classes of cardiac muscle cells • • Specialized muscle cells of the conducting system Contractile cells B. The Conducting System - Fig. 20.12 • The conducting system includes: • • • Sinoatrial (SA) node Atrioventricular (AV) node Conducting cells • Atrial conducting cells are found in internodal pathways • Ventricular conducting cells consist of the AV bundle, bundle branches, and Purkinje fibers C. Impulse Conduction through the heart - Fig. 20.13 • • • • • SA node begins the action potential Stimulus spreads to the AV node Impulse is delayed at AV node Impulse then travels through ventricular conducting cells Then distributed by Purkinje fibers D. The electrocardiogram (ECG) - Fig. 20.14 • A recording of the electrical events occurring during the cardiac cycle • • • The P wave accompanies the depolarization of the ventricles The QRS complex appears as the ventricles depolarize The T wave indicates ventricular repolarization F. The cardiac cycle - Fig. 20.16, 20.17 • • The period between the start of one heartbeat and the beginning of the next During a cardiac cycle • • Each heart chamber goes through systole and diastole Correct pressure relationships are dependent on careful timing of contractions 1) Pressure and volume changes: atrial systole • • • rising atrial pressure pushes blood into the ventricle atrial systole the end-diastolic volume (EDV) of blood is in the ventricles 2) Pressure and volume changes: ventricular systole • • Isovolumetric contraction of the ventricles: ventricles are contracting but there is no blood flow Ventricular pressure increases forcing blood through the semilunar valves 3) Pressure and volume changes: ventricular diastole • • The period of isovolumetric relaxation when all heart valves are closed Atrial pressure forces the AV valves open G. Heart sounds - Fig. 20.18 • • Auscultation – listening to heart sound via stethoscope Four heart sounds • • • • S1 – “lubb” caused by the closing of the AV valves S2 – “dupp” caused by the closing of the semilunar valves S3 – a faint sound associated with blood flowing into the ventricles S4 – another faint sound associated with atrial contraction IV. Cardiodynamics A. Stroke Volume and Cardiac Output - Fig. 20.19, 20.20 • Cardiac output – the amount of blood pumped by each ventricle in one minute • Cardiac output equals heart rate times stroke volume B. Factors Affecting Heart Rate • Autonomic innervation • Cardiac reflexes • Tone • SA node • Hormones • Epinephrine (E), norepinephrine(NE), and thyroid hormone (T 3) • Venous return C. Factors Affecting stoke volume - Fig. 20.23 • • EDV • Frank-Starling principle ESV • Preload • Contractility • Afterload D. Summary: Regulation of Heart Rate and Stroke Volume • Sympathetic stimulation increases heart rate • Parasympathetic stimulation decreases heart rate • Circulating hormones, specifically E, NE, and T 3, accelerate heart rate • Increased venous return increases heart rate • EDV is determined by available filling time and rate of venous return • ESV is determined by preload, degree of contractility, and afterload