* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
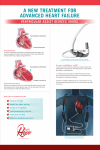
Download Ventricular assist devices are primarily indicated for either a one or a
Baker Heart and Diabetes Institute wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Electrocardiography wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Jatene procedure wikipedia , lookup
Heart failure wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Cardiac surgery wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
During my clinical experience, it was my privilege to spend time on the transplant unit. While there, I assisted in the care of several patients whose primary diagnosis was congestive heart failure. As a result of their weakened heart, these patients were provided a ventricular assist device to assist in the circulation of blood. The ventricular assist device was certainly the highlight of my clinical experience this semester and the purpose of this paper is to correlate the use of ventricular assist devices with other comorbidities. Ventricular assist devices are primarily indicated for either a one or a combination of several factors. These factors include destination therapy, bridge to transplant, bridge to recovery, and eligibility for transplant. Most often, congestive heart failure is the causative force that necessitates the placement of a VAD. Congestive heart failure can be defined as an inability of the heart to generate an adequate cardiac output to perfuse vital tissues. Cardiac output is dependent upon heart rate and stroke volume. Stroke volume is influenced by three major determinants: contractility, preload, and afterload. Any disease that disrupts the activity of the myocyte reduces contractility. Ejection fraction is the measurement used to quantify the force by which the heart is pumping blood. Normal ejection fraction ranges from 55 – 70%. This means that up to 70% of the total circulating blood volume is forced out through the left ventricle after one contraction. For one of the patients that I cared for, contractility was so diminished (ejection fraction of 15%) that continuous inotrope infusion was necessary to maintain a viable ejection fraction. CHF affects nearly 10% of individuals older than age 65. Ischemic heart disease and hypertension are the most important predisposing risk factors of congestive heart failure. Other risk factors include age, obesity, diabetes, renal failure, valvular heart disease, cardiomyopathies, myocarditis, congenital heart disease, and excessive alcohol use. Of these risk factors, my patient was diagnosed with hypertension, coronary artery disease, and diabetes. Some of the interventions necessary for a patient with a VAD in place are primarily preventative in nature. The goals of therapy include the prevention of infections and maintaining a therapeutic level of blood fluidity. Infections alone increase the risk of a thromboembolic event, further increasing the amount of anticoagulant therapy a patient may need (Wever-Pinzon, et al., 2012). Pharmacological choices of anticoagulation and antiplatelet therapy recommendations vary largely, partly due to the variance between devices. Dabigtran is a new medication recently approved by the Food and Drug Administration. This medication is a direct thrombin inhibitor that disrupts the clotting cascade of both free and clot-bound thrombin (Wever-Pinzon, et al., 2012). For the patient in my care, maintaining the balance between bleeding and thrombus formation and preventing infections were the priority interventions. This was accomplished through the use of aspirin and warfarin, and periodically checking clotting times. When necessary, times of increased clotting, heparin was initiated to return the patient to a therapeutic level of anticoagulation. Meticulous care was practiced during the VAD driveline dressing change. The effects of infection thwart almost every aspect of VAD therapy and the nurses’ attention to detail was indicative of this knowledge. Between the recommended interventions and the therapeutic measures I witnessed during my time on the transplant unit, I noticed no gaps of care. Moreover, the attention to detail of the nurses’ I shadowed inspired me to incorporate such diligence within my own nursing practice. I thoroughly enjoyed my time on the unit and learned a great deal about how caring, compassionate, and competent nurses operate on a daily basis. I look forward to working with nurses of similar dedication once I graduate from this program. Bibliography Drakos, S. G., Kfoury, A. G., Selzman, C. H., Verma, D. R., & Nanas, J. N. (2011). Left ventricular assist device unloading effects on myocardial structure and function: current status of the field and call for action. Current Opinions Cardiology , 26 (3), 245-255. Wever-Pinzon, O., Stehlik, J., Kfoury, A., Terrovitis, J., Diakos, N., Charitos, C., et al. (2012). Ventricular assist devices: Pharmacological aspects of a mechanical therapy. Pharmacology & Therapeutics , 134 (2), 189-199.